This document provides information about exercise stress testing, including:
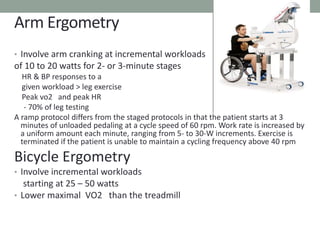
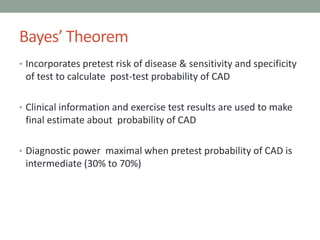
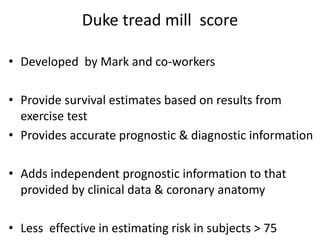
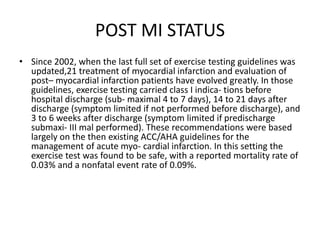
1. Exercise stress testing is a fundamental test used to evaluate cardiovascular disease that is easy to perform, flexible, reliable, and inexpensive.
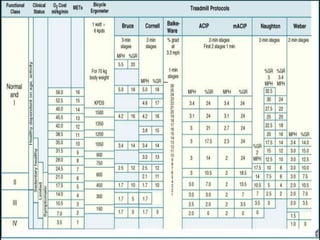
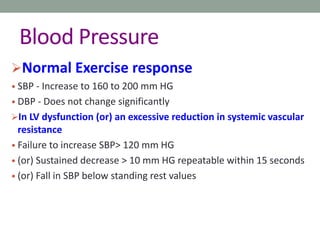
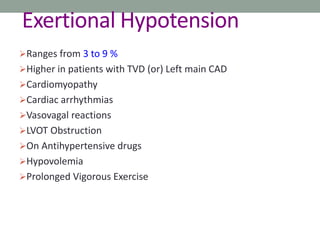
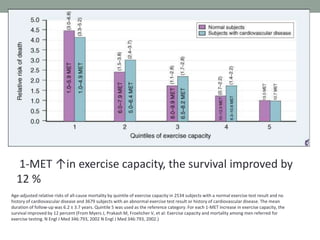
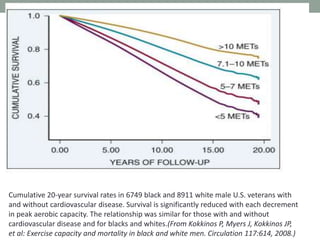
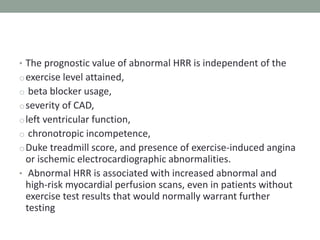
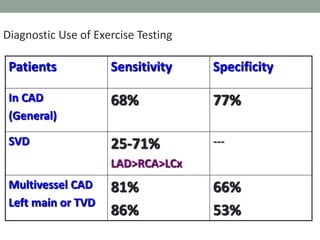
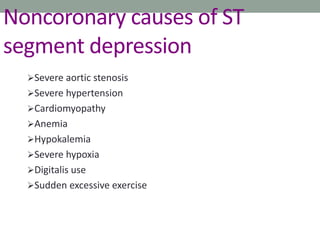
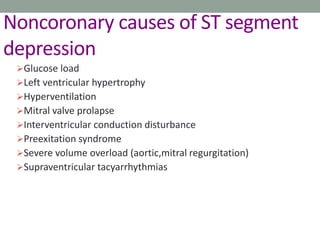
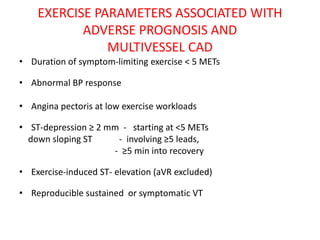
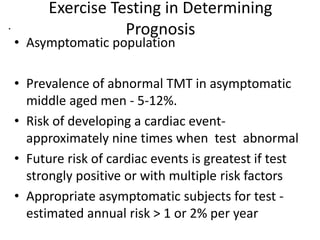
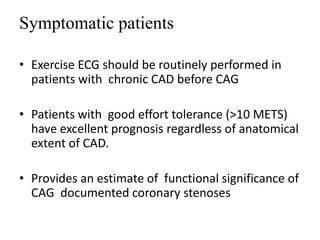
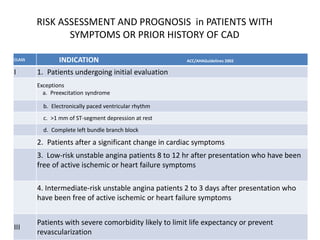
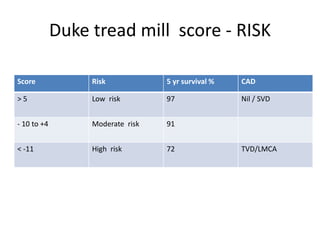
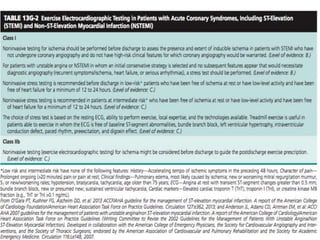
2. Exercise stress testing can elicit abnormalities not seen at rest, estimate functional capacity and prognosis of coronary artery disease, and evaluate many cardiovascular conditions.
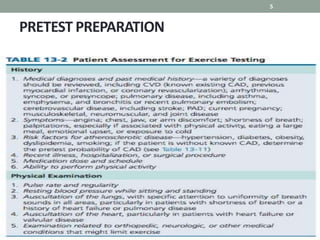
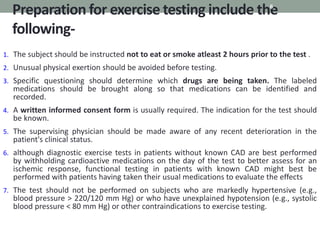
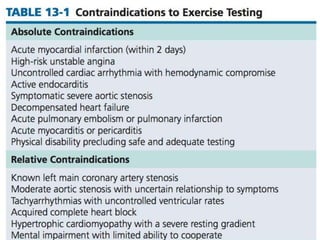
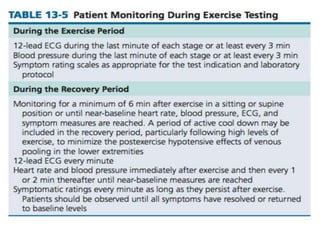
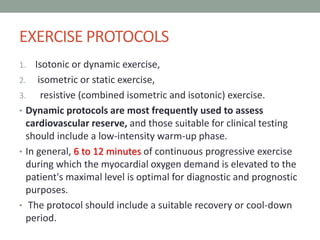
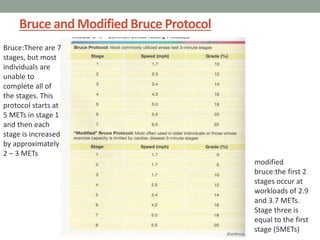
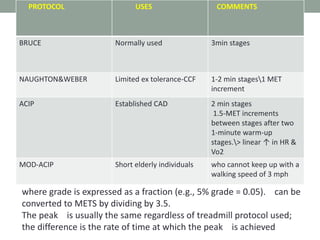
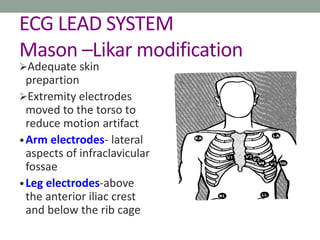
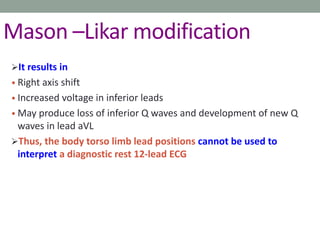
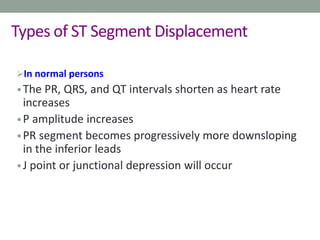
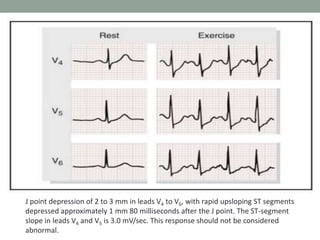
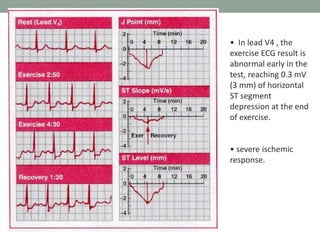
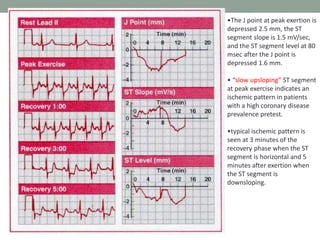
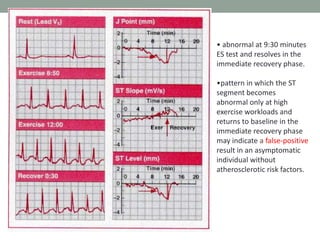
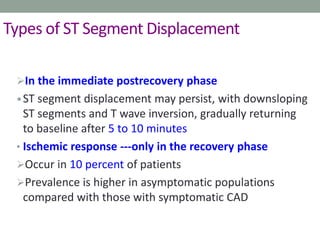
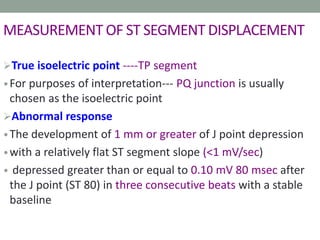
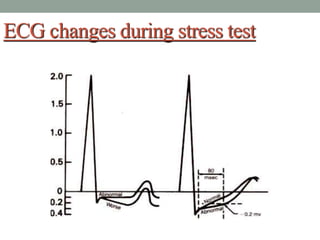
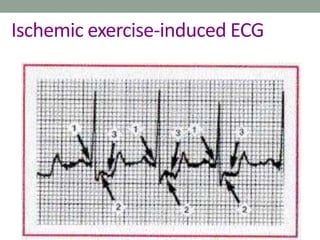
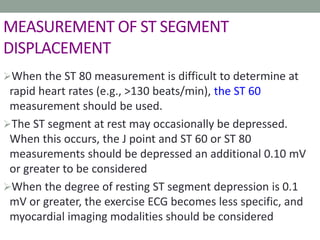
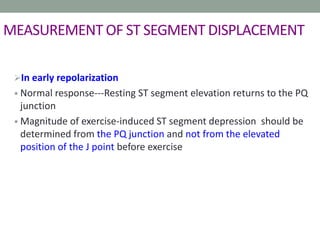
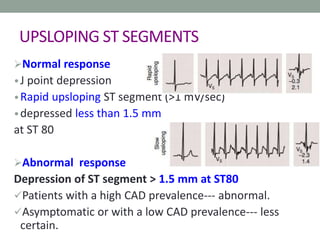
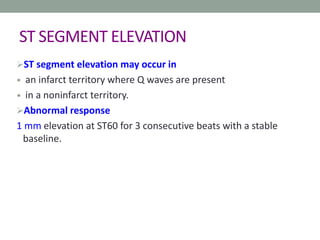
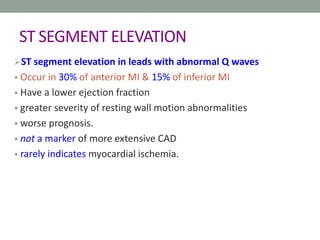
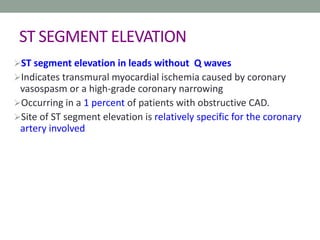
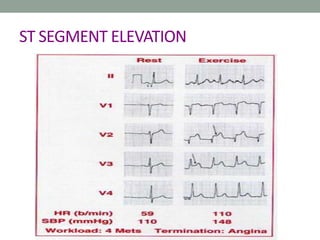
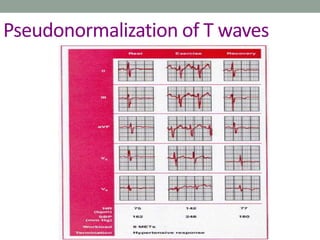
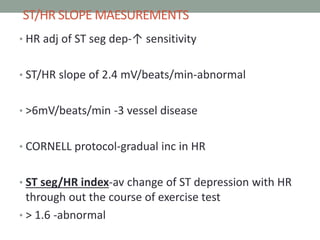
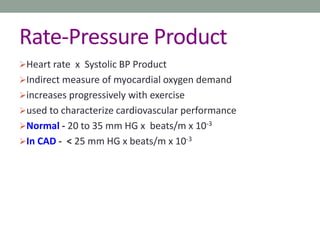
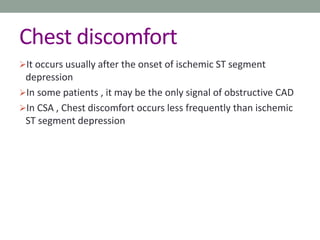
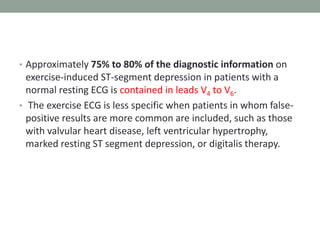
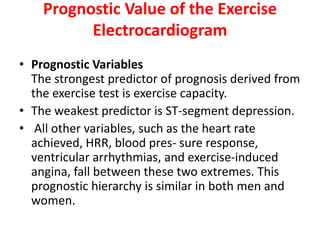
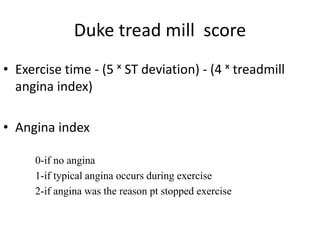
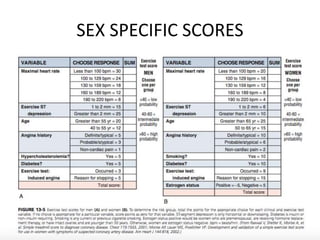
3. Proper patient preparation, test protocol selection, monitoring during the test, and follow up are important to ensure safety and accurate results. Electrocardiogram measurements during the test help identify ischemic changes indicative of cardiovascular disease.