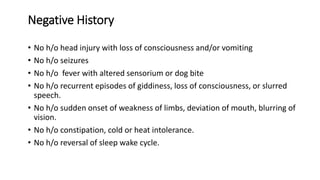
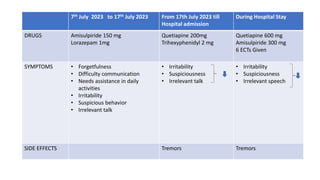
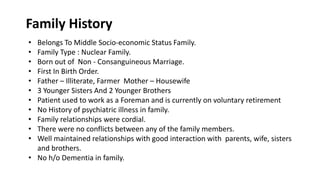
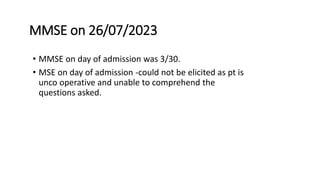
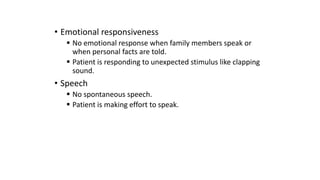
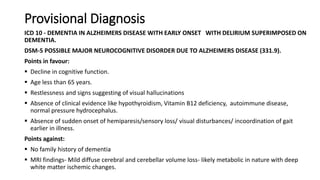
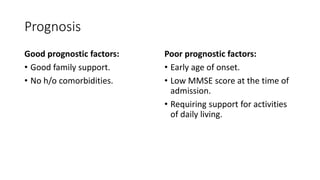
A 50-year-old male was brought by his wife with complaints of forgetfulness, difficulty communicating, and needing assistance with daily activities over the past 5 years. His symptoms had been progressively worsening. On examination, he had low MMSE scores, impaired speech and language skills, and decreased responsiveness. Brain MRI showed cerebral and cerebellar atrophy and white matter changes. He was diagnosed with probable major neurocognitive disorder due to Alzheimer's disease with superimposed delirium. He was started on cholinesterase inhibitors and memantine for his dementia along with antipsychotics to address behavioral issues.