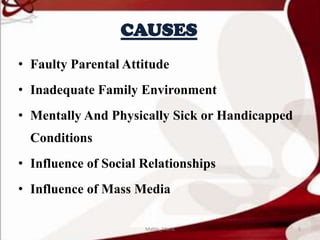
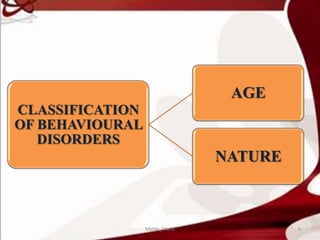
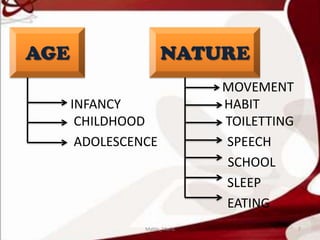
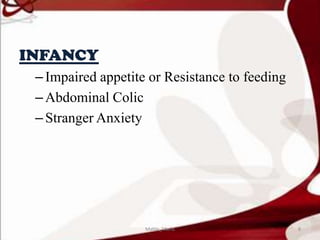
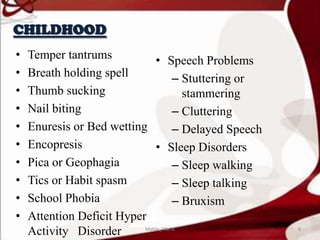
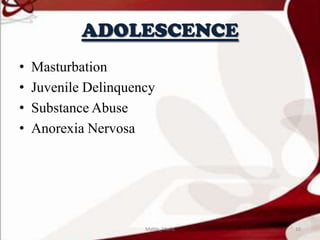
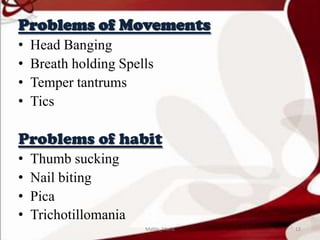
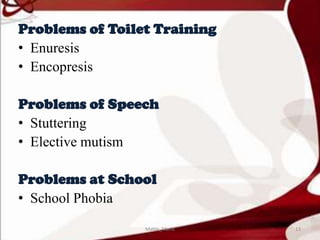
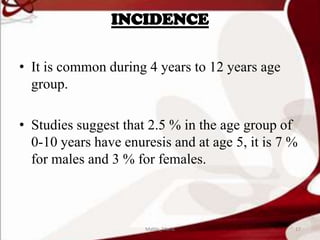
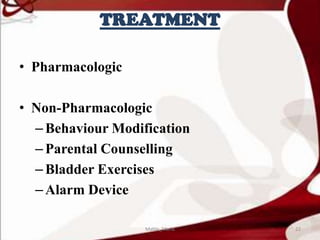
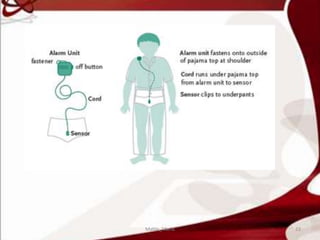
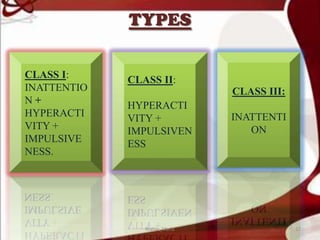
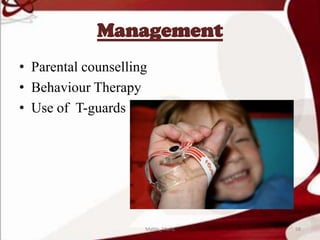
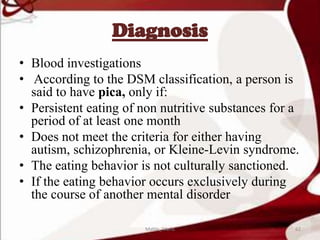
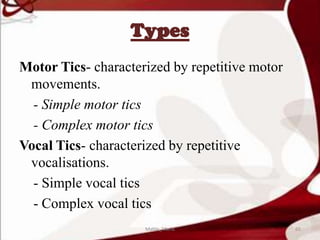
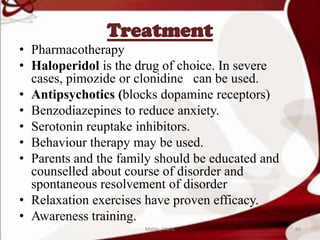
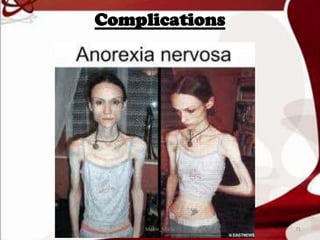
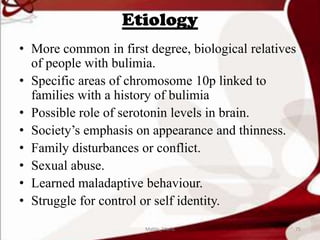
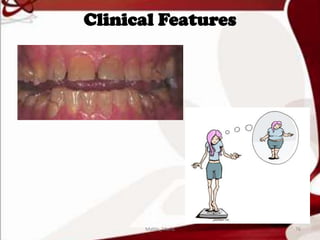
The document discusses various behavioral disorders seen in children and adolescents. It defines conditions like enuresis, encopresis, temper tantrums, breath holding spells, pica, tics, anorexia nervosa, bulimia nervosa, stuttering, cluttering, school phobia and stranger anxiety. It describes the incidence, causes, clinical features and management of each condition. The management involves both pharmacological and non-pharmacological approaches like behavioral therapy, counseling and lifestyle modifications.