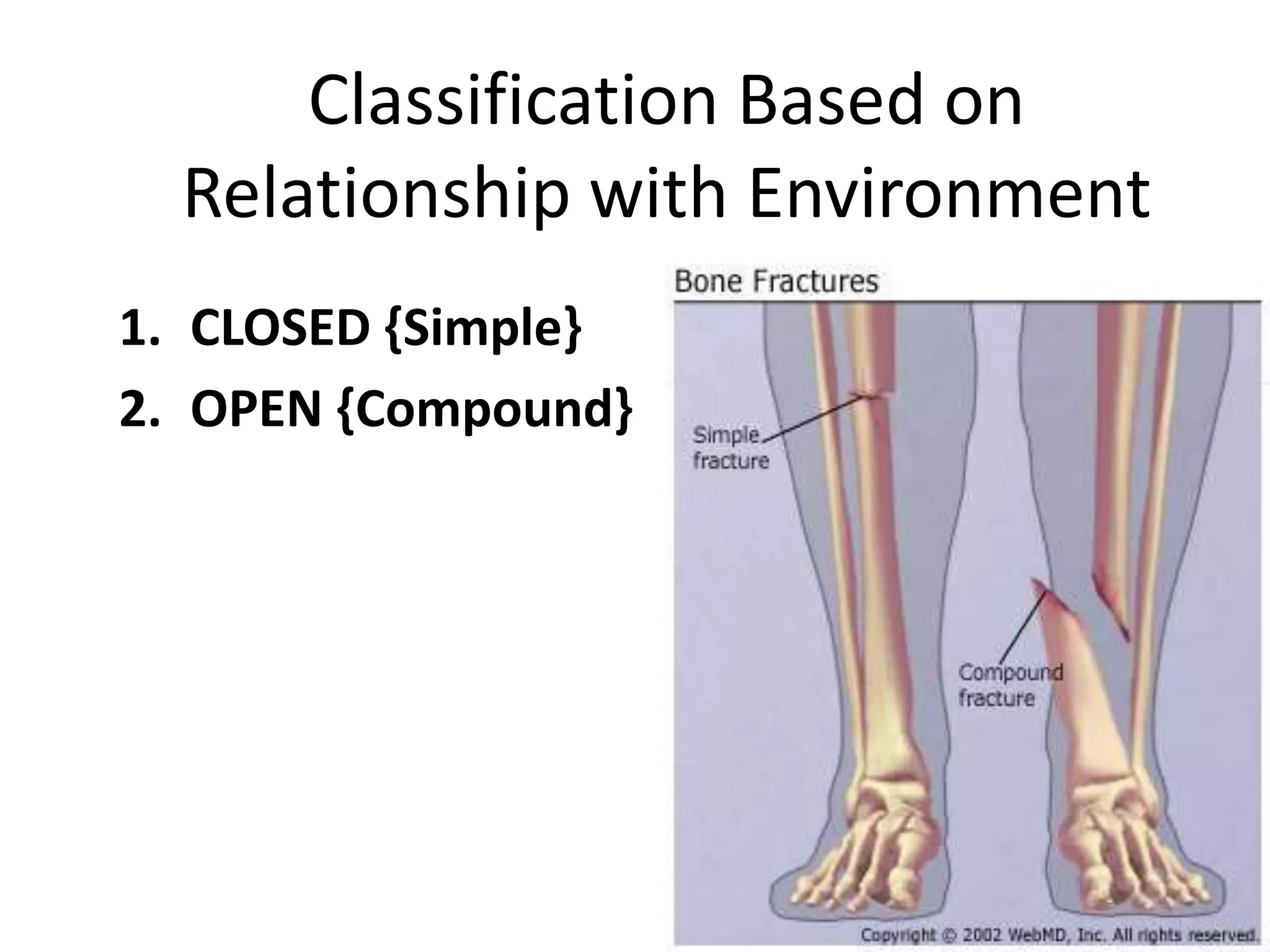
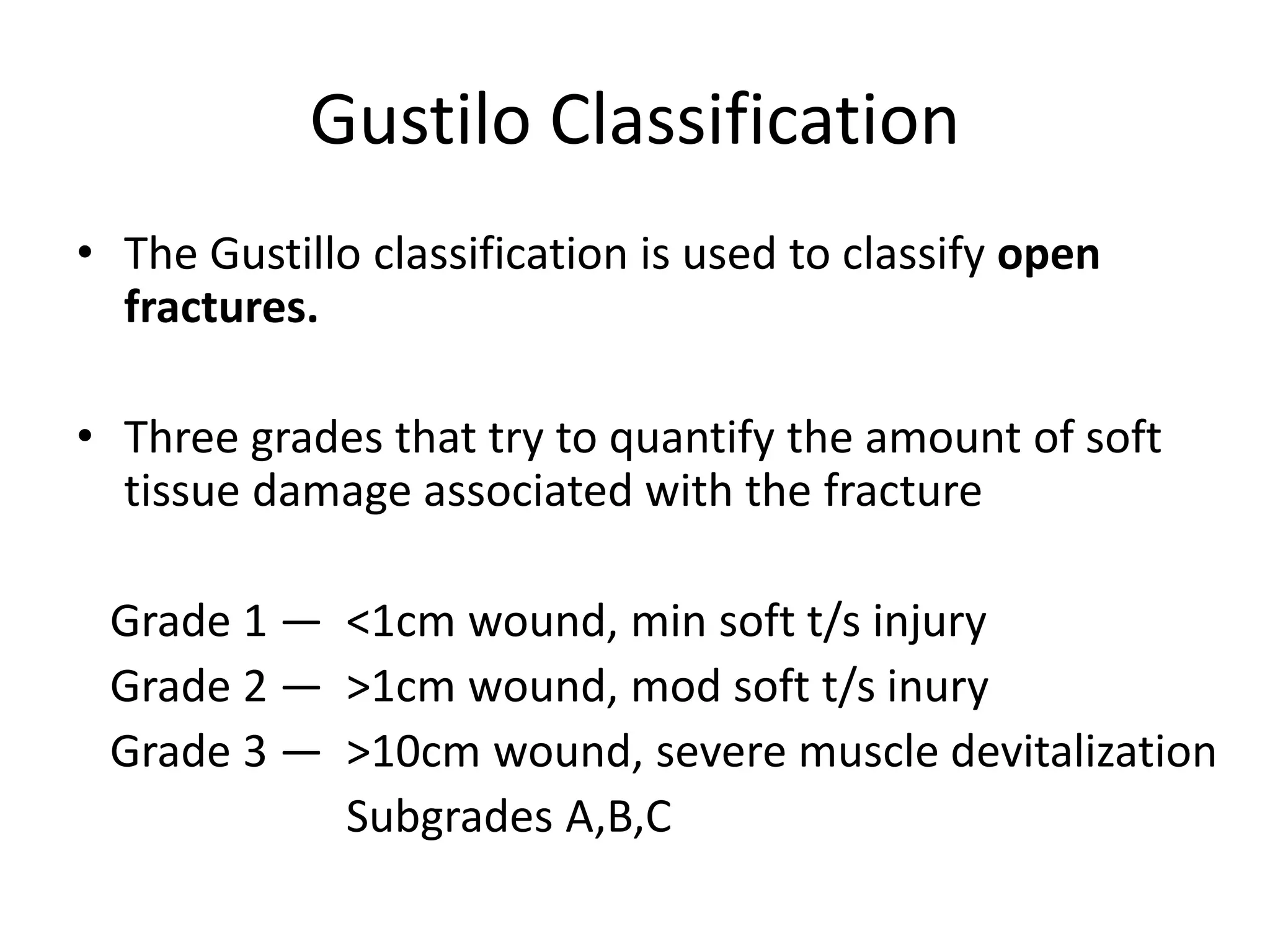
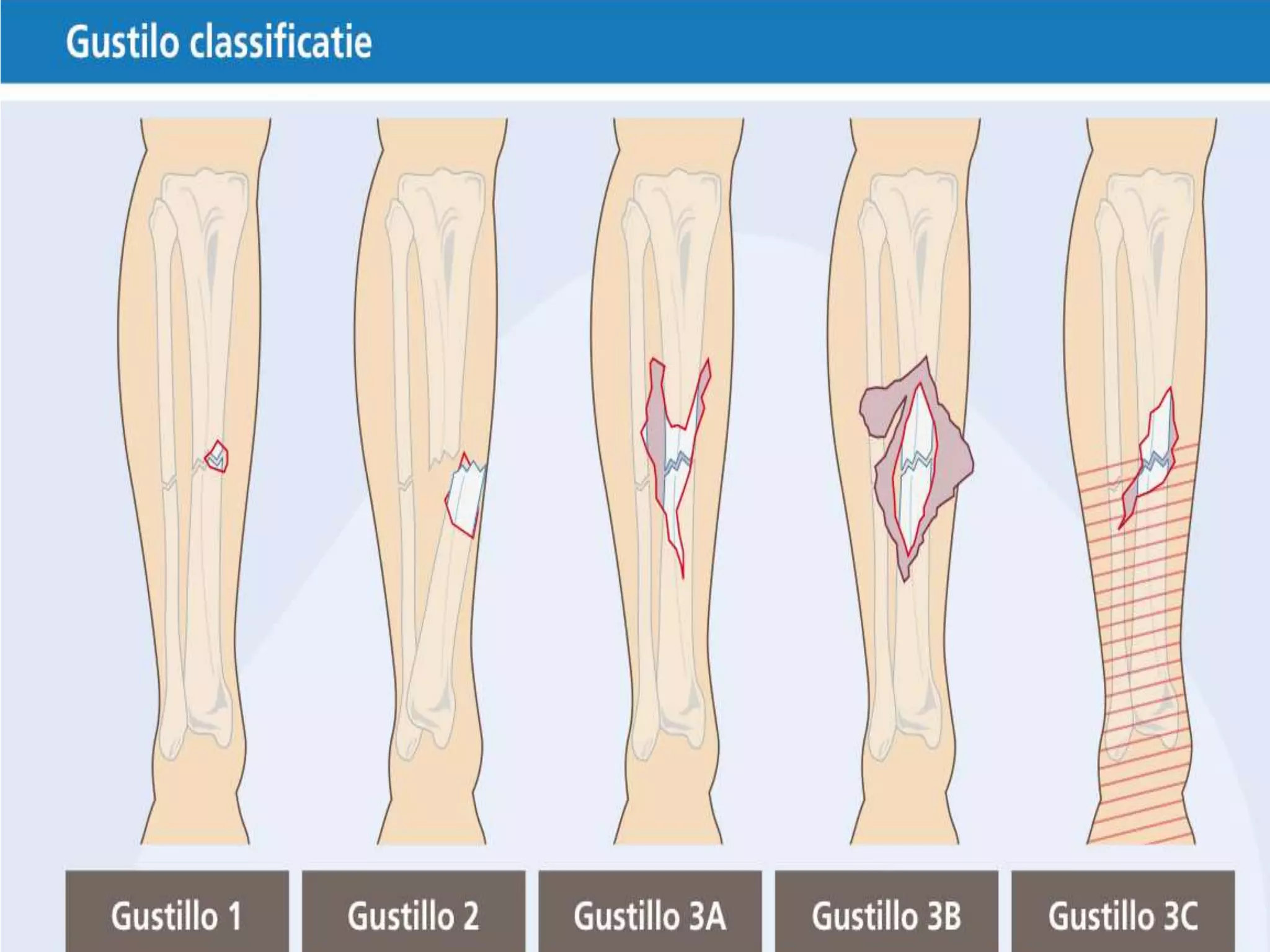
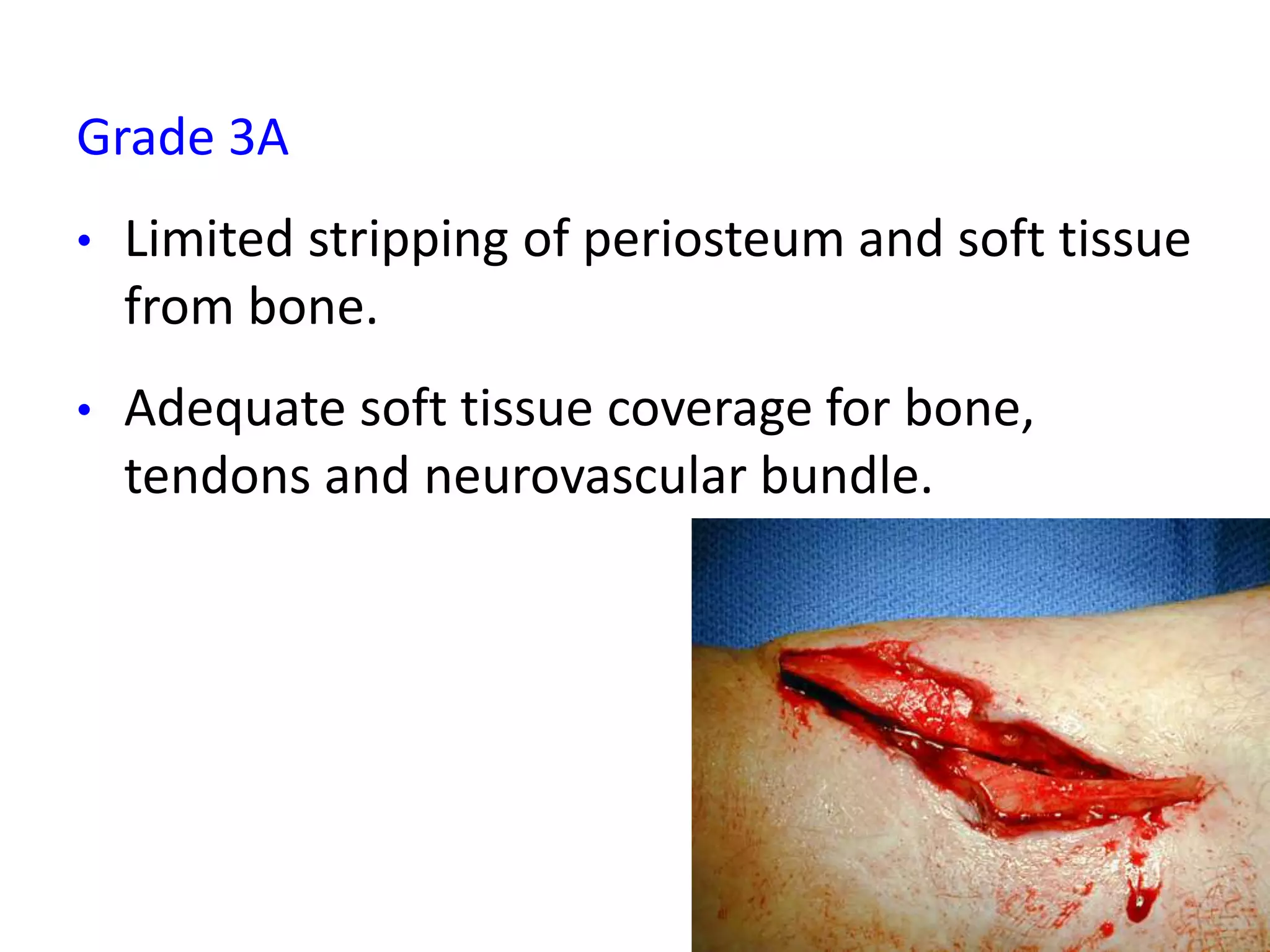
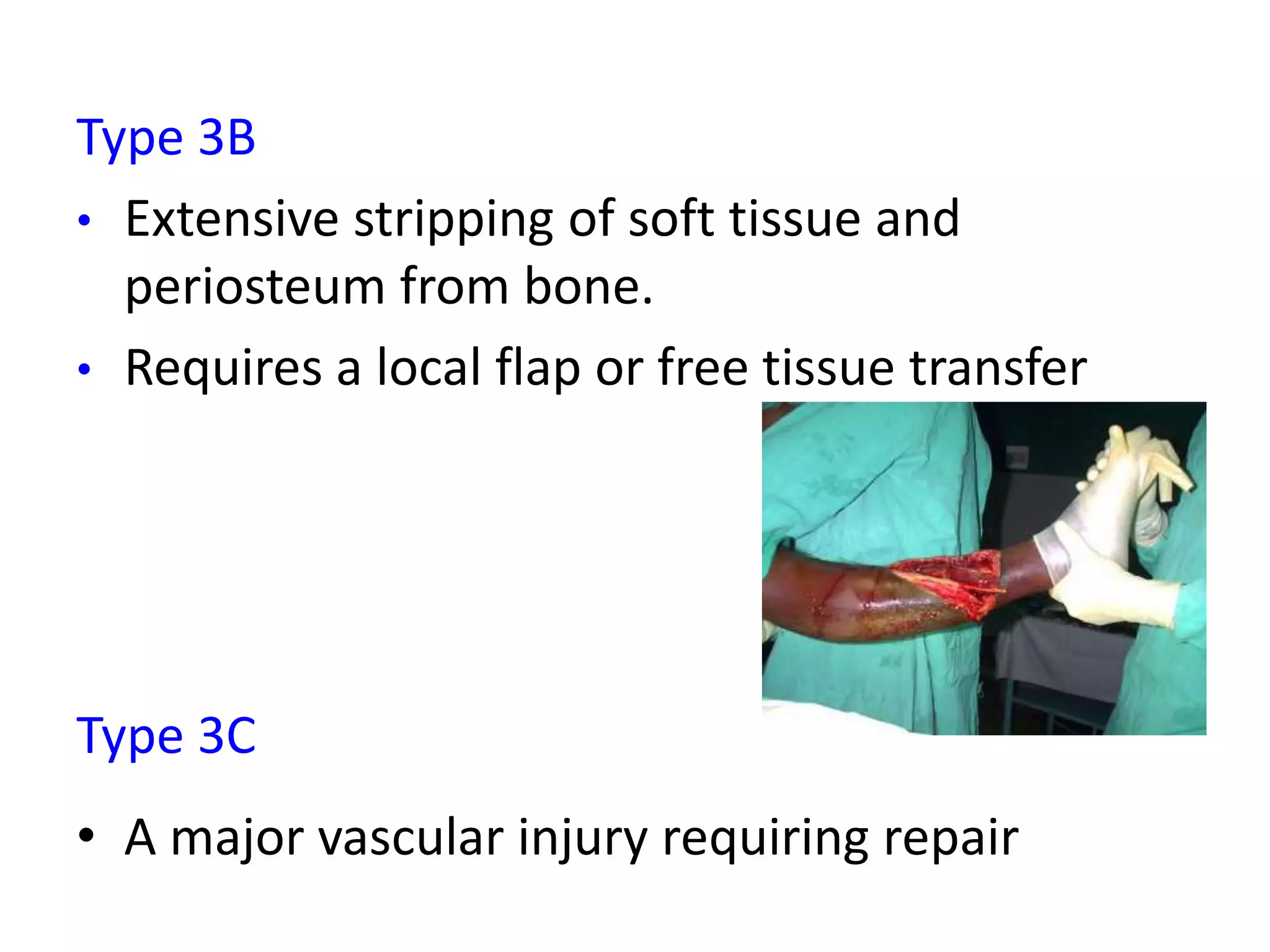
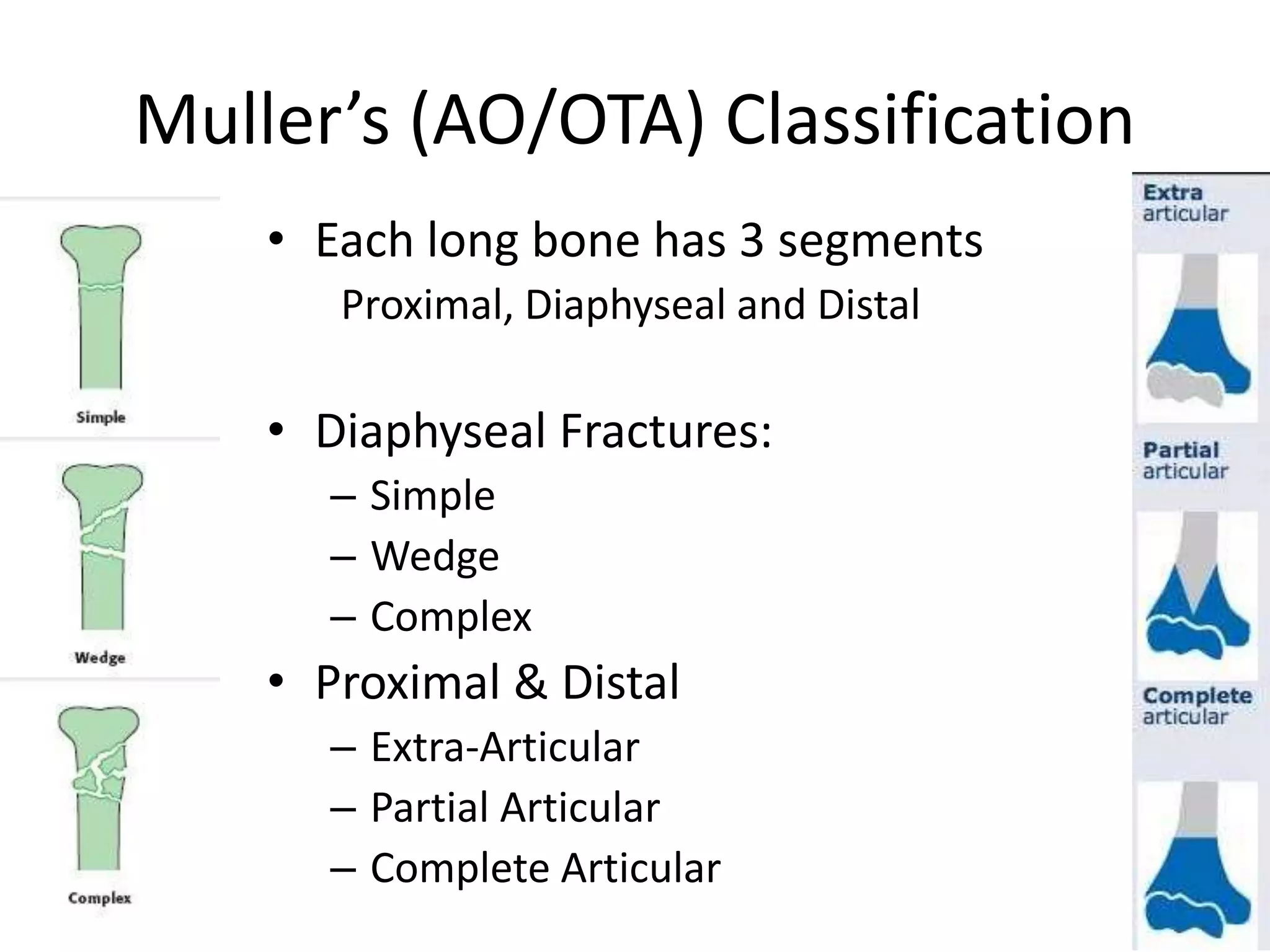
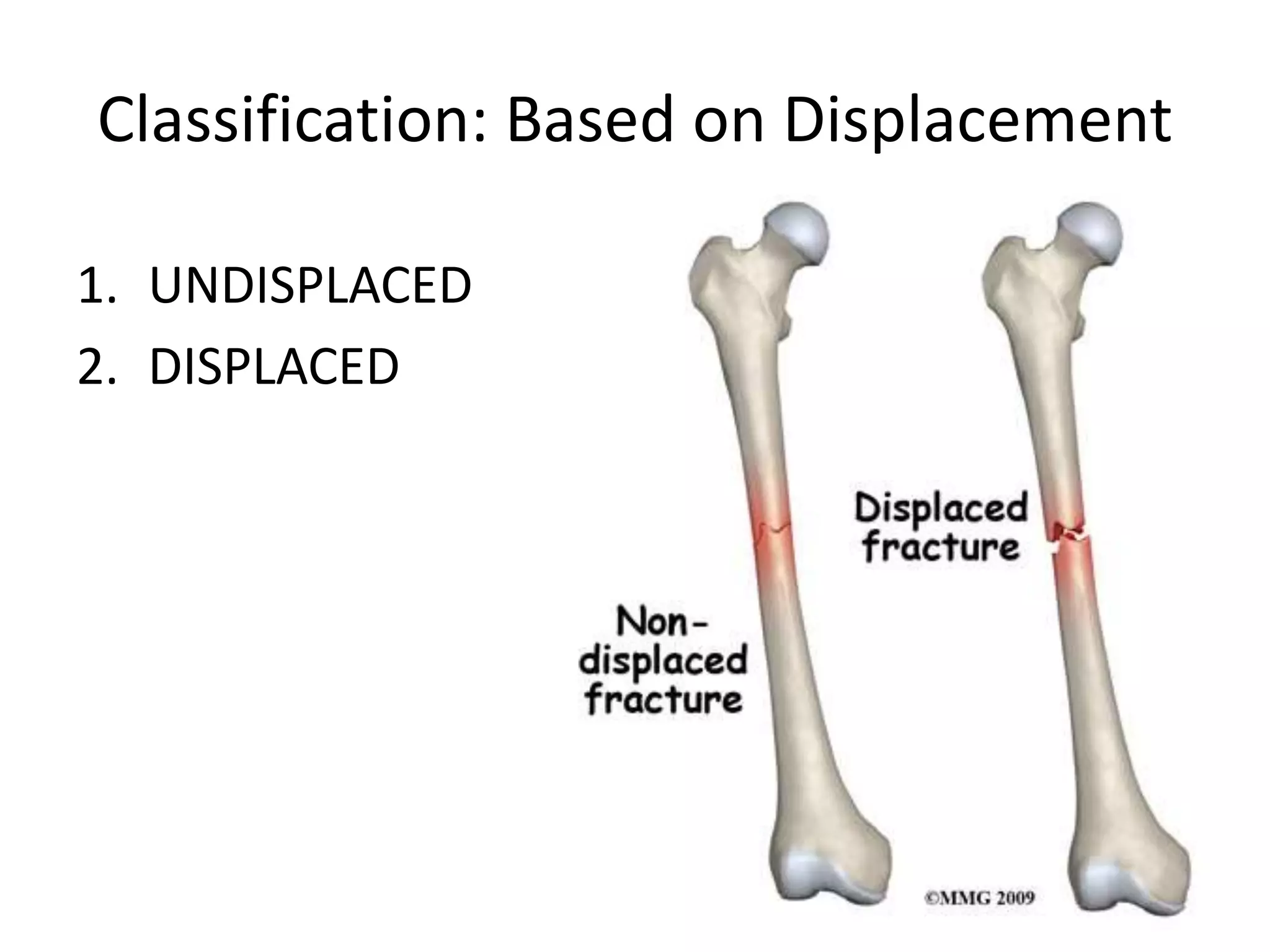
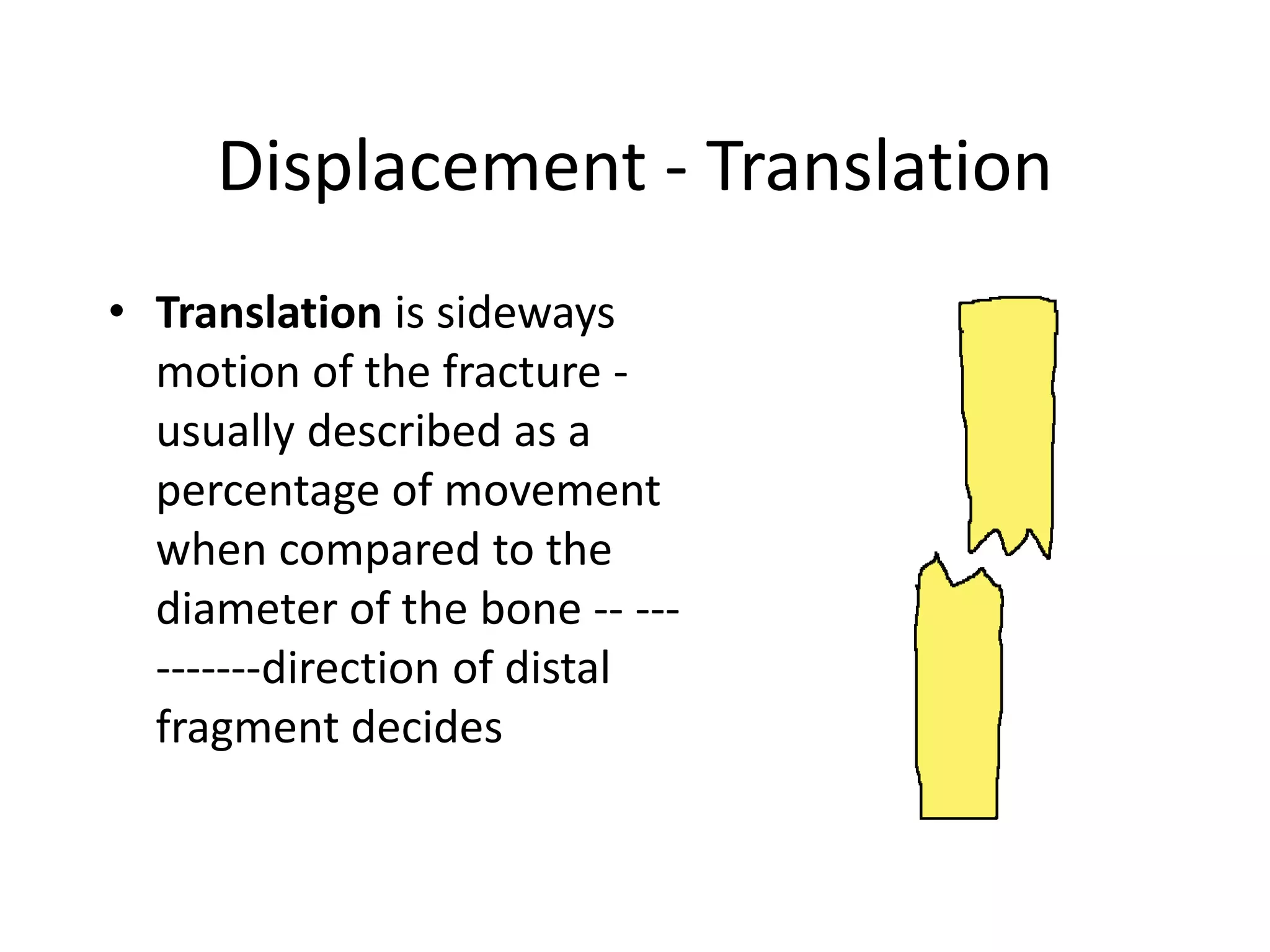
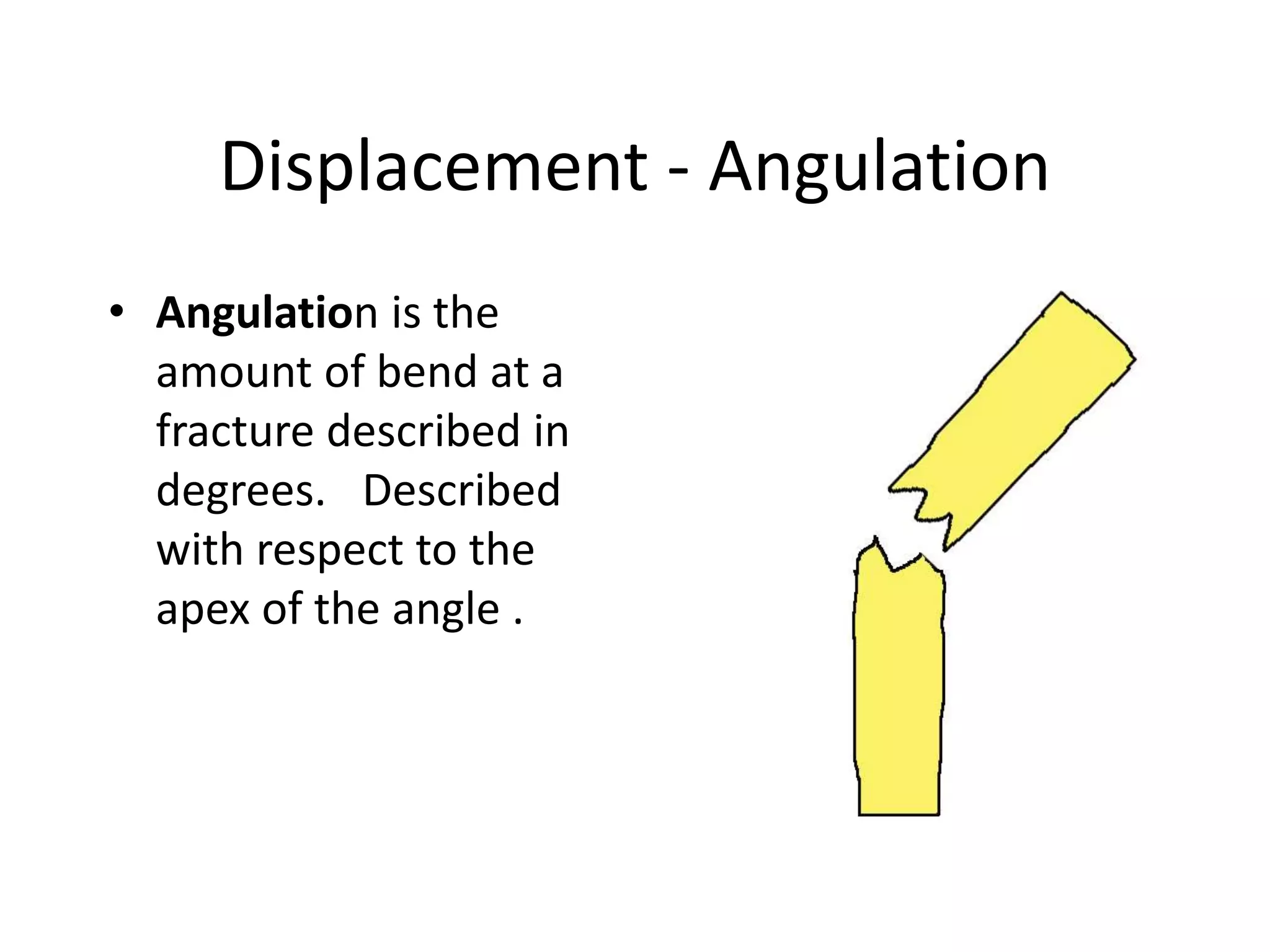
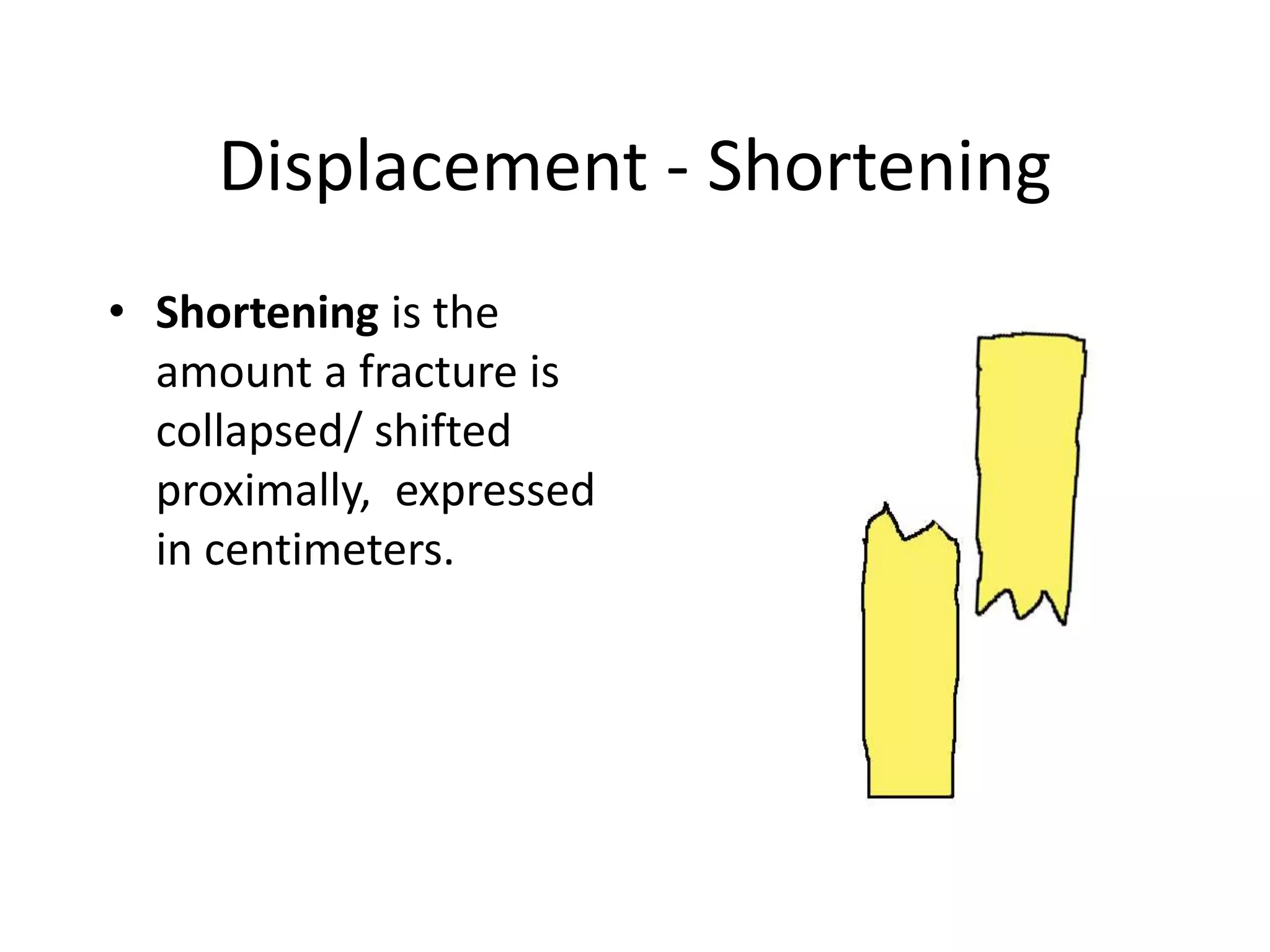
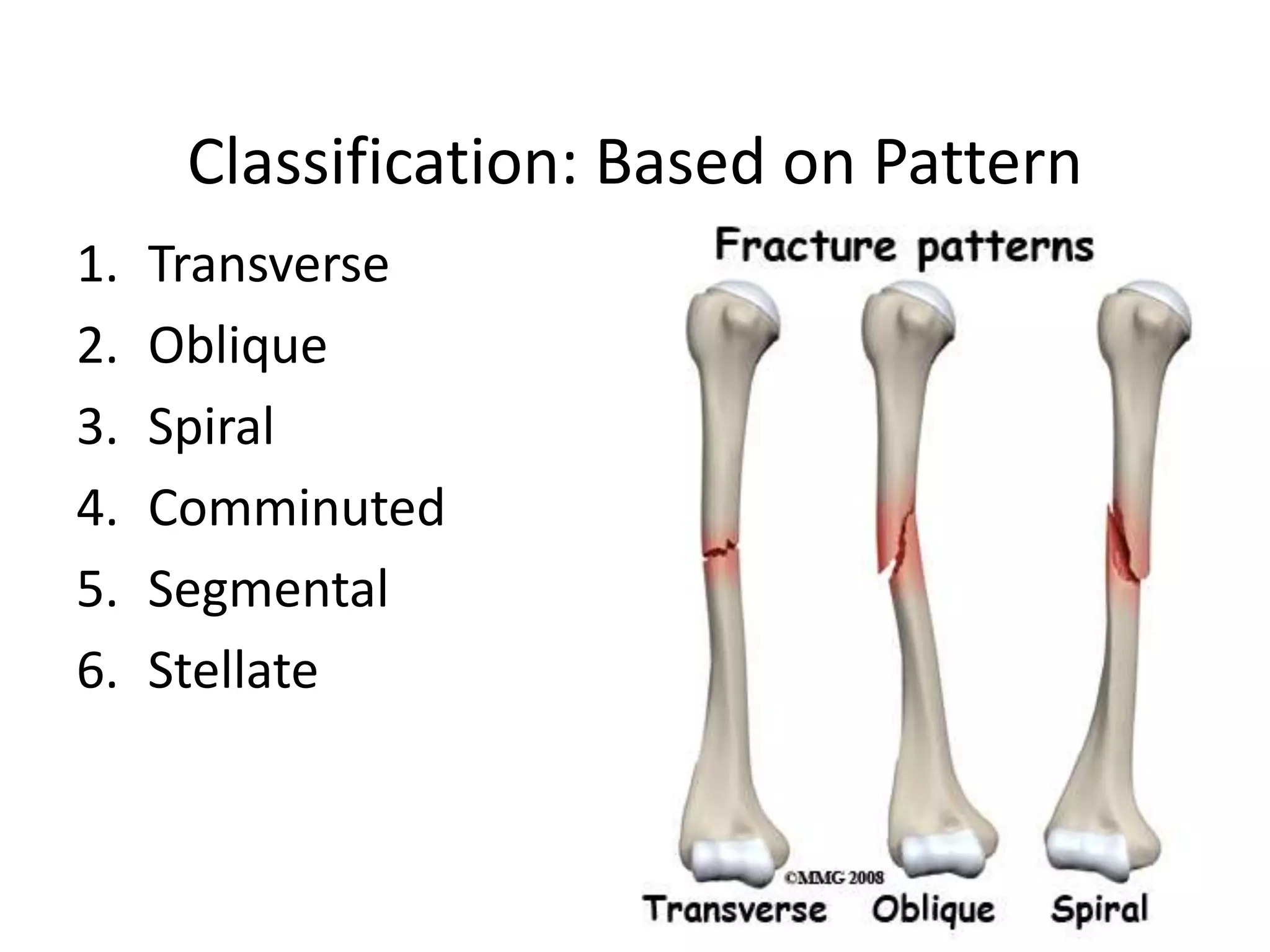
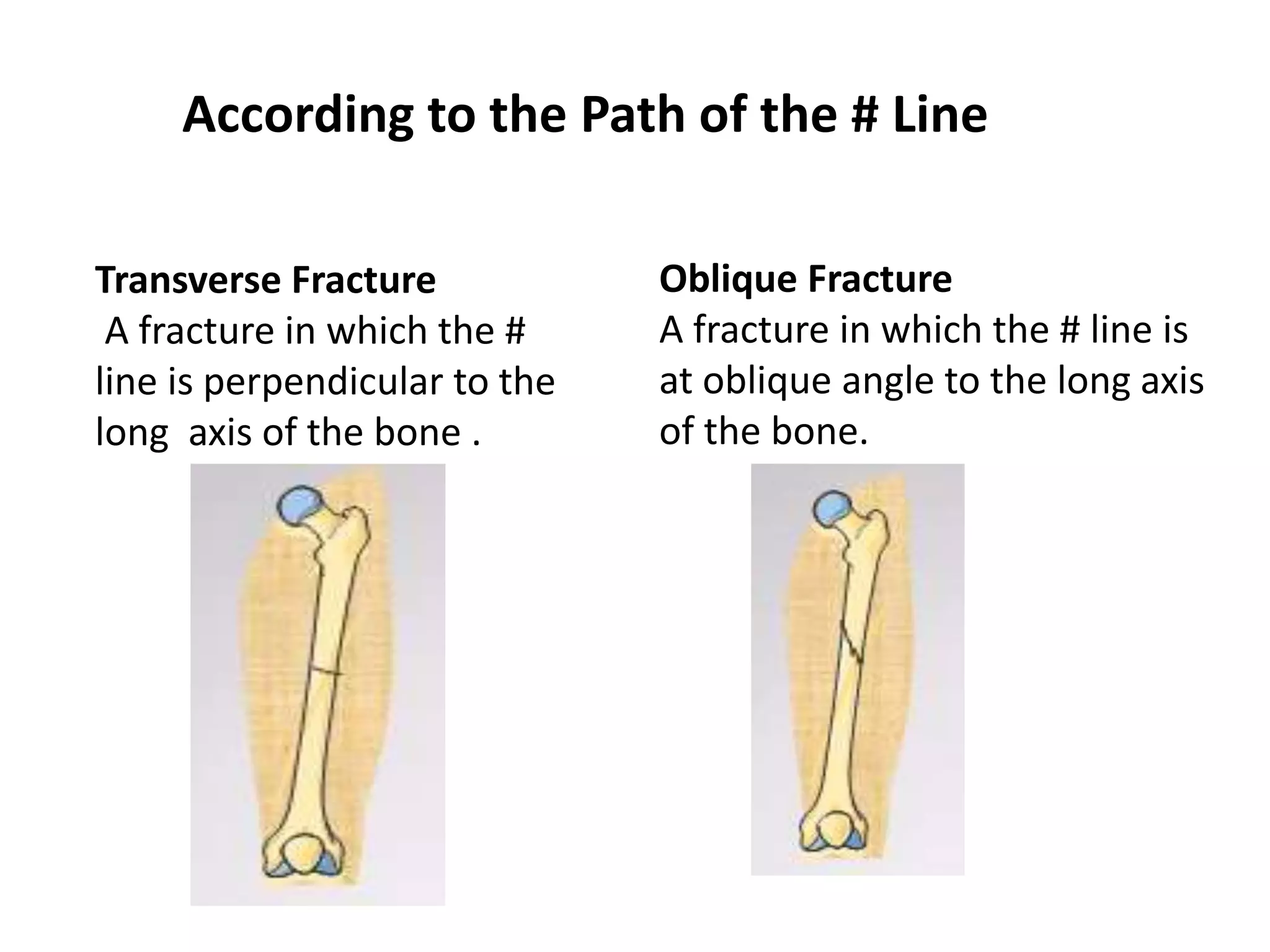
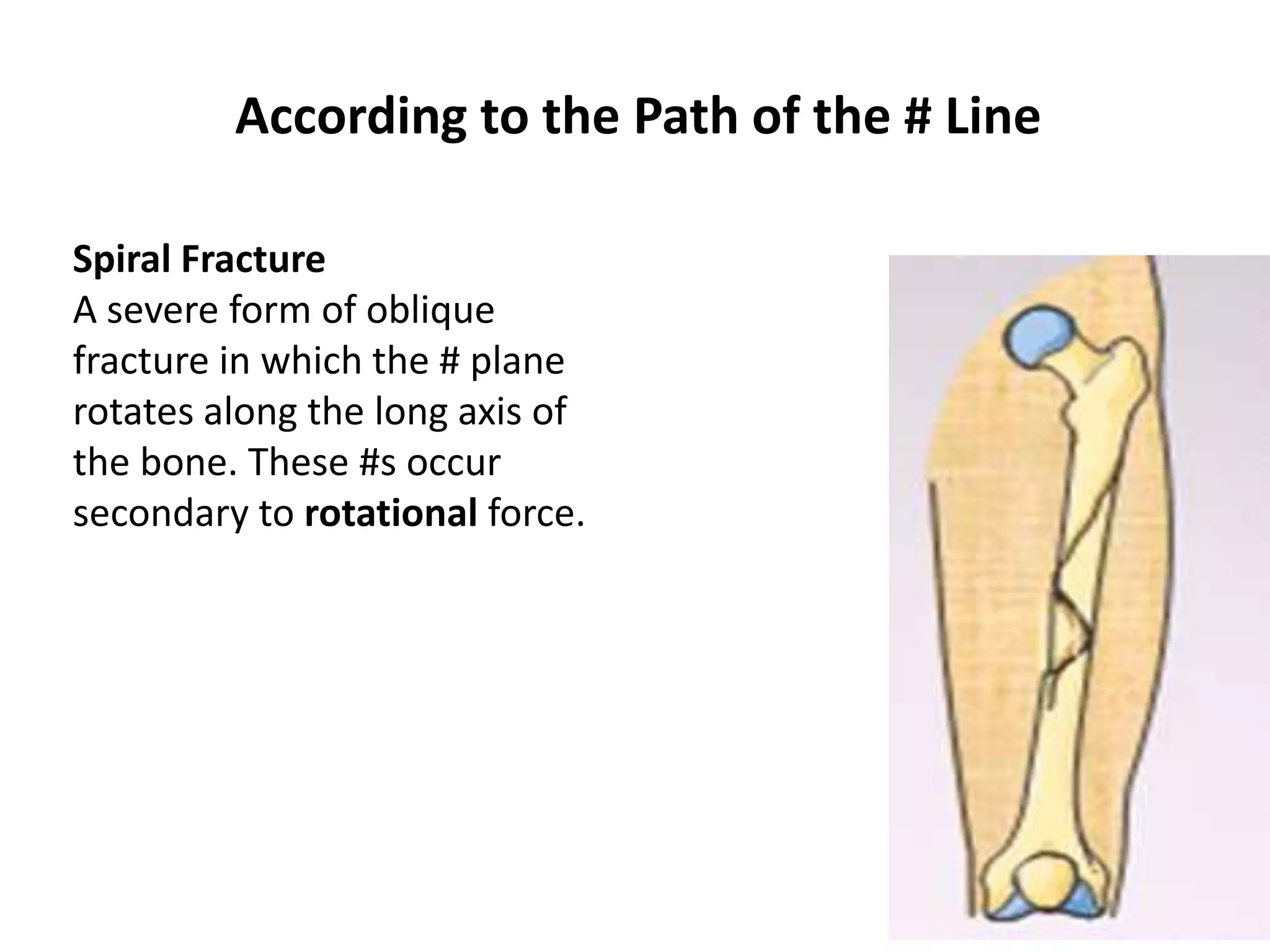
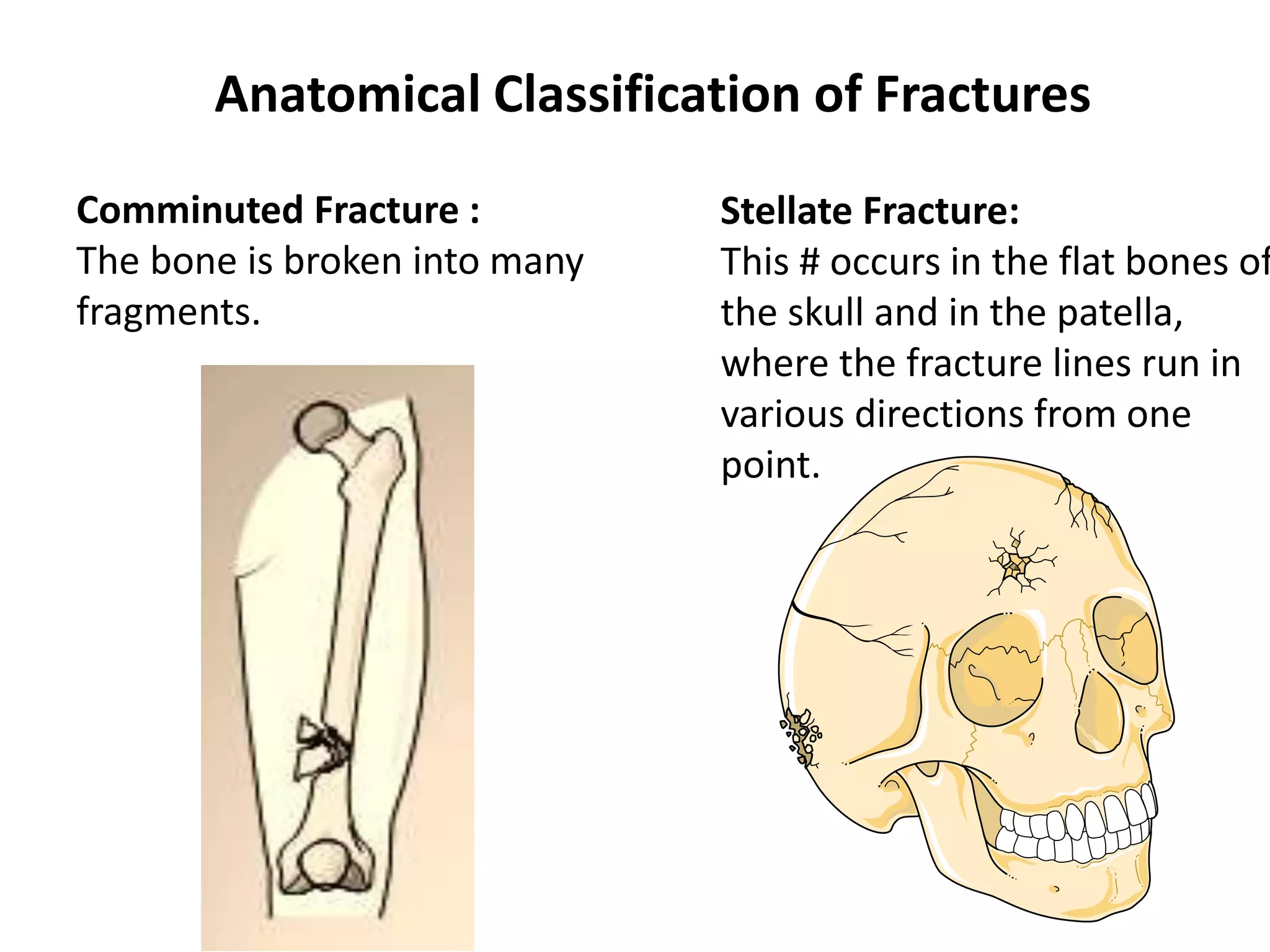
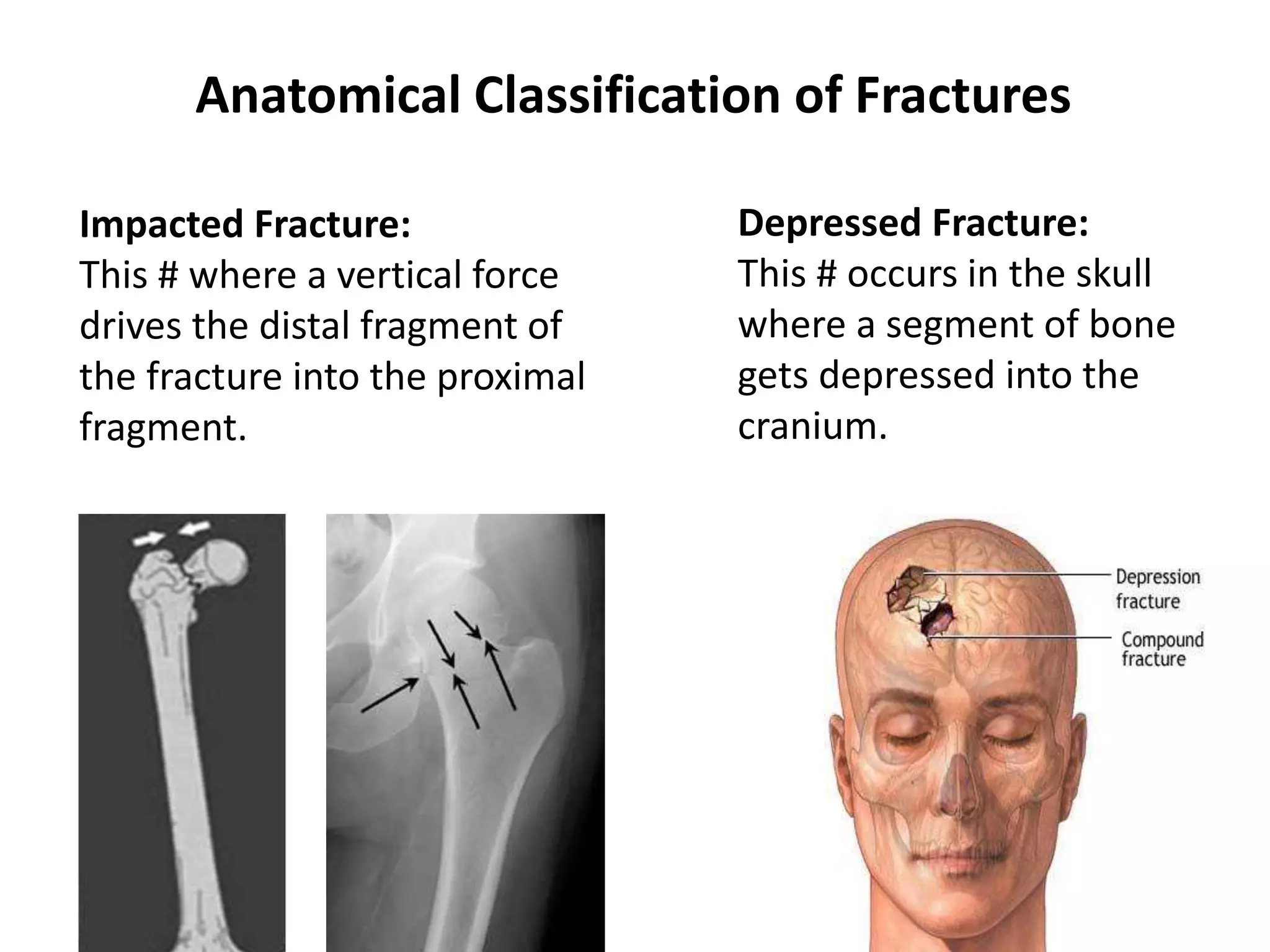
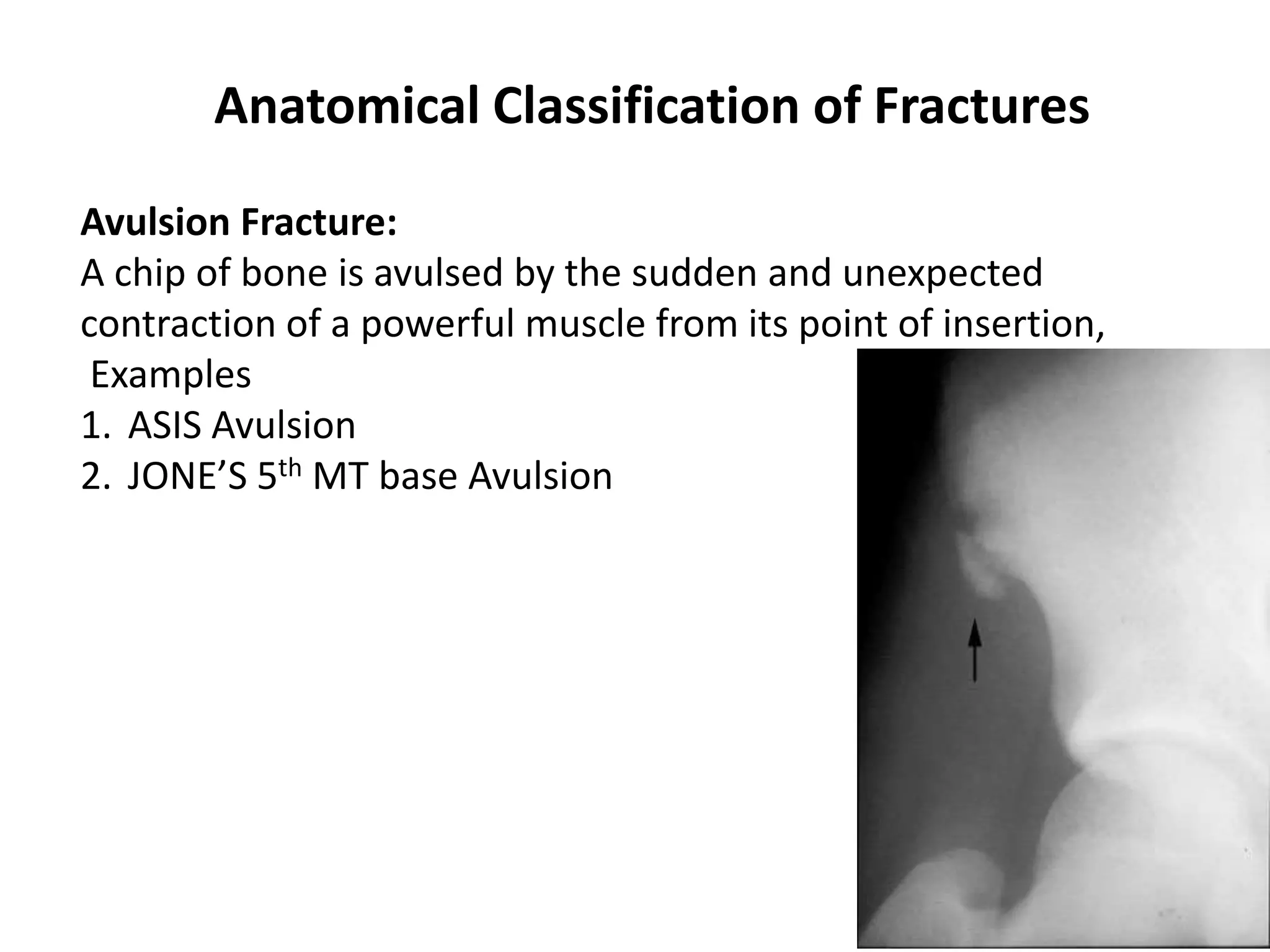
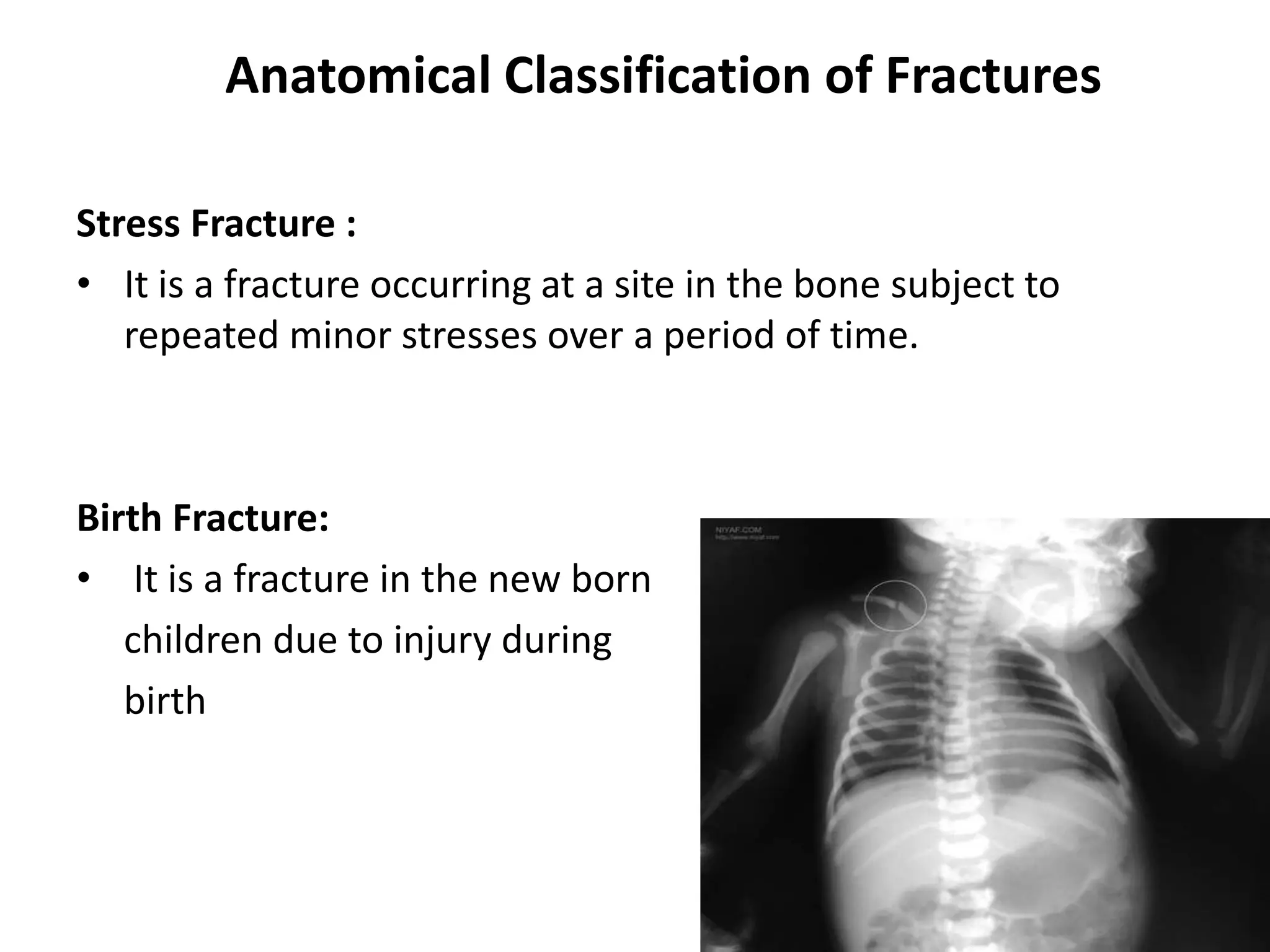
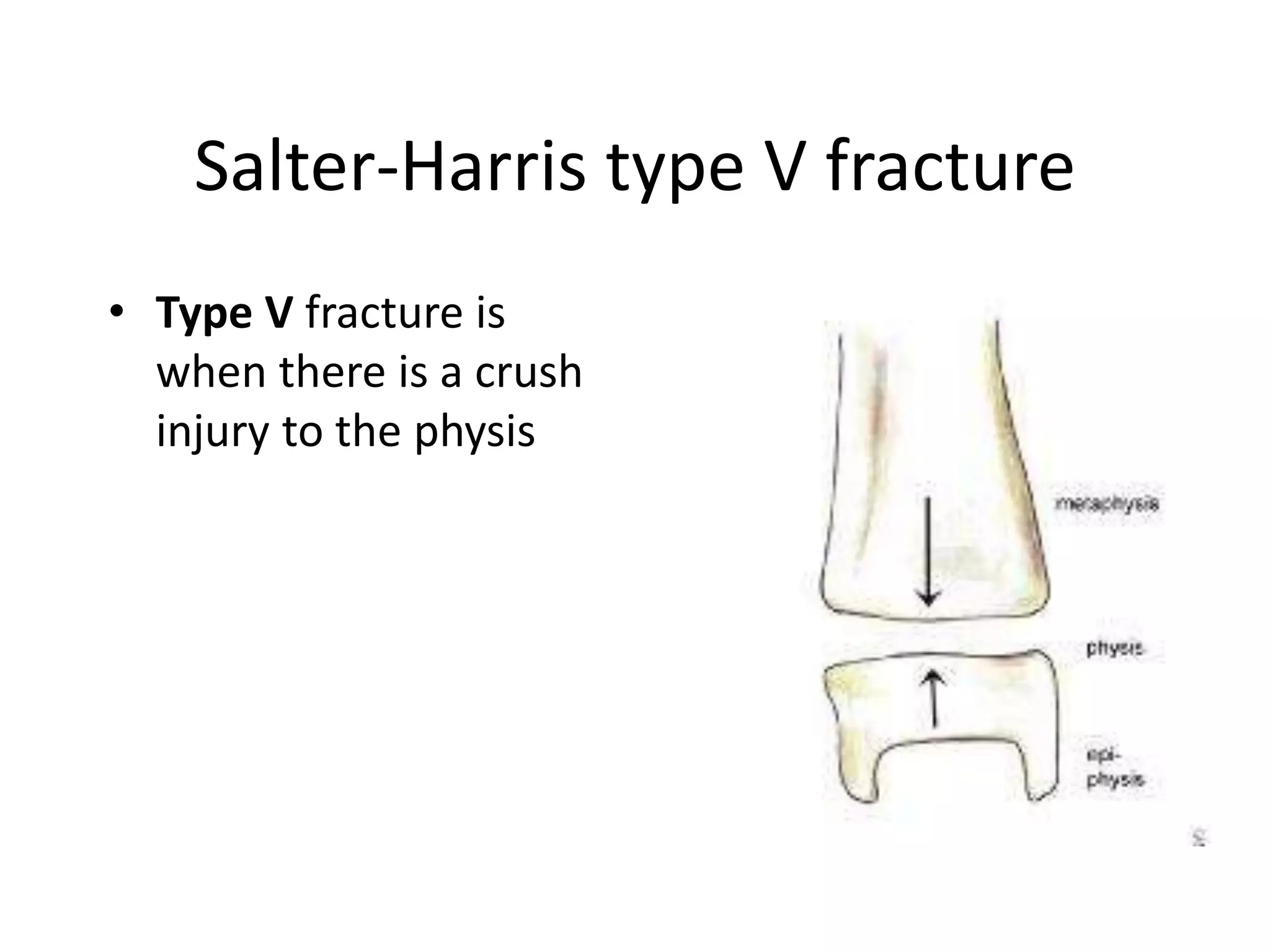
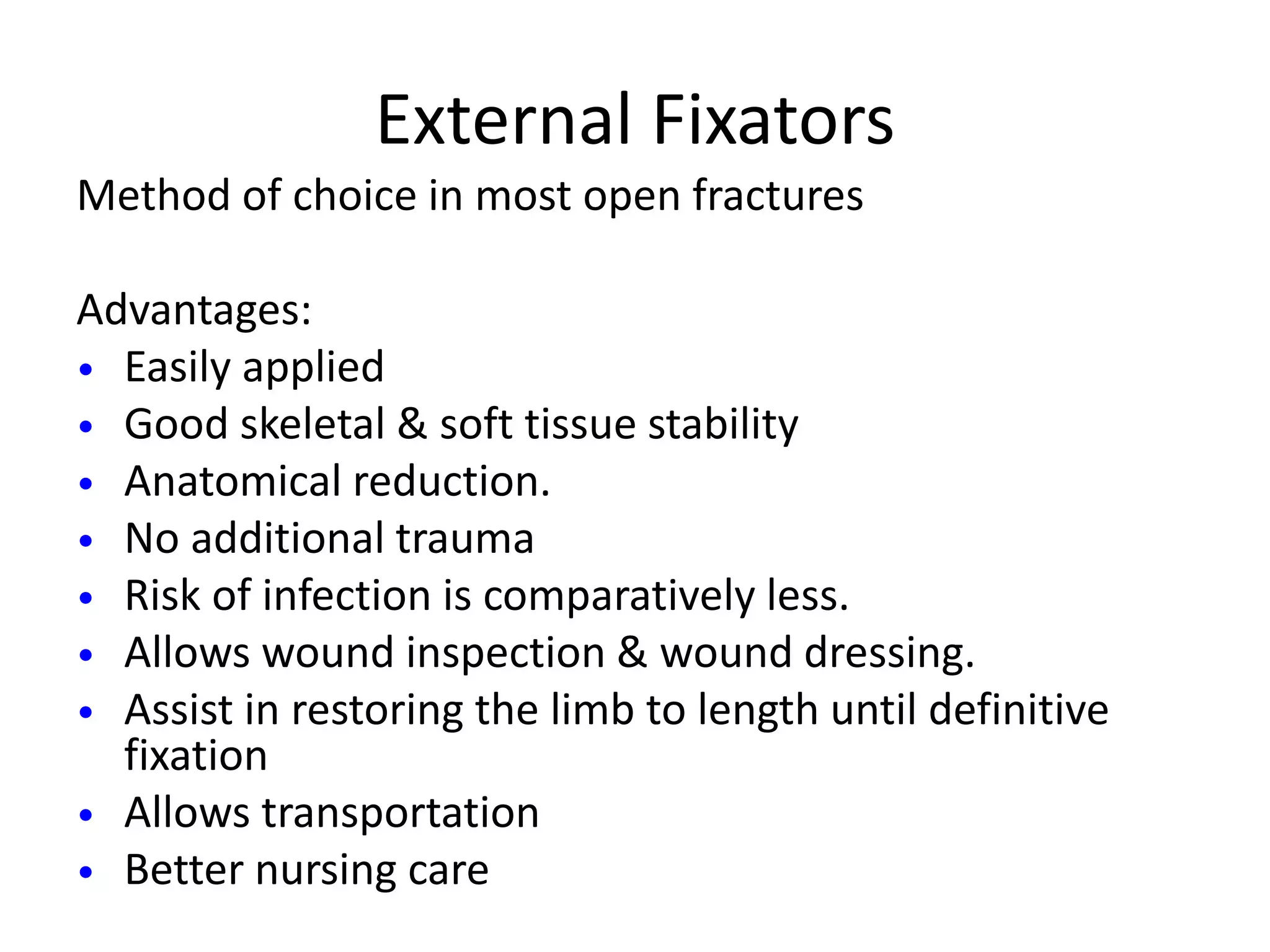
This document discusses the classification and management of fractures, including compound fractures. It describes several classification systems for fractures based on their relationship to the environment, degree of displacement, fracture pattern, and etiology. It also discusses the Gustilo classification system for open fractures. For treatment of compound fractures, the document emphasizes the importance of antibiotic prophylaxis, debridement of the wound and fracture, stabilization of the fracture, and early wound coverage. It describes various methods of fracture stabilization, including external and internal fixation.