More Related Content
Similar to Terapia fotodinamica en el tto furcas
Similar to Terapia fotodinamica en el tto furcas (20)
Terapia fotodinamica en el tto furcas
- 1. Photodynamic therapy in the
treatment of class II furcation:
a randomized controlled clinical
trial
Luchesi VH, Pimentel SP, Kolbe MF, Ribeiro FV, Casarin RC, Nociti FH Jr,
Sallum EA, Casati MZ. Photodynamic therapy in the treatment of class II
furcation: a randomized controlled clinical trial. J Clin Periodontol 2013; 40: 781–788.
doi: 10.1111/jcpe.12121.
Abstract
Aim: To investigate the effect of photodynamic therapy (PDT) as adjunct to
mechanical therapy in furcations.
Materials and Methods: A double-blind, parallel, randomized controlled clinical
trial was conducted in subjects presenting class II furcations. The subjects were
randomly allocated to a test (PDT; n = 16) or control group (non-activated laser/
only photosensitizer; n = 21). At baseline, 3 and 6 months, clinical, microbiologi-
cal and cytokine pattern evaluation was performed. Clinical attachment level was
defined as the primary outcome variable.
Results: Clinical parameters improved after both therapies (p < 0.05) with no
differences between groups at any time point (p > 0.05). At 6 months, real-time
PCR evaluation showed a decrease in Porphyromonas gingivalis and Tannerella
forsythia only in the PDT group (p < 0.05) with no inter-group differences.
Regarding cytokines, IL-4 and IL-10 levels increased in both groups at 6 months.
GM-CSF, IL-8, IL-1b and IL-6 levels decreased only in the PDT group after
3 months (p < 0.05). At 3 months, inter-group analyses showed that GM-CSF,
IFN-c, IL-6 and IL-8 levels were lower in the PDT group. At 6 months, lower
IL-1b levels were also observed in the PDT group (p < 0.05).
Conclusion: Photodynamic therapy did not promote clinical benefits for class II
furcations; however, advantages in local levels of cytokines and a reduction in
periodontopathogens were demonstrated.
Vanessa H. Luchesi1
,
Suzana P. Pimentel1
,
Maria F. Kolbe1
,
Fernanda V. Ribeiro1
,
Renato C. Casarin1
,
Francisco H. Nociti Jr2
,
Enilson A. Sallum2
and
Marcio Z. Casati1
1
Dental Research Division, School of
Dentistry, Paulista University S~ao Paulo, S~ao
Paulo, Brazil; 2
Department of Prosthodontics
and Periodontics, School of Dentistry at
Piracicaba, University of Campinas
(UNICAMP) Piracicaba, S~ao Paulo, Brazil
Key words: chronic periodontitis; cytokines;
furcation defects; microbiology; periodontal
pocket; photochemotherapy; root planing
Accepted for publication 1 May 2013
Photodynamic therapy (PDT) as an
adjunct to subgingival mechanical
debridement has been considered to
be a promising therapeutic approach
for periodontal therapy (Braun et al.
2008, Campos et al. 2013). PDT com-
bines the use of a photoactivatable
non-toxic chemical agent (photosensi-
tizer) with low-level light energy
(Chan & Lai 2003). Photodynamic
therapy is considered a non-invasive
therapeutic method able to selectively
target periodontal pathogens, thus
avoiding damage to the host tissues
(Soukos et al. 1998).
Furcation involvements are fre-
quently observed in individuals
presenting with periodontitis and
approximately 50% of the molars in
patients above 40 years of age
exhibit these conditions (Svardstr€om &
Wennstr€om 1996). In addition,
Conflict of interest and source of
funding
This study was supported by FAPESP
(S~ao Paulo Research Foundation) –
processes 2010/51218-8 and the National
Council for Technological and Scientific
Development (CNPq) – processes
303693/2009-6. The authors report
no conflicts of interest related to this
study.
© 2013 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd 781
J Clin Periodontol 2013; 40: 781–788 doi: 10.1111/jcpe.12121
- 2. longitudinal trials have revealed that
in molars with furcation involvement
responding least favourably to peri-
odontal therapy, they are more sus-
ceptible to further attachment loss
and are considered at greater risk of
extraction compared with defects sur-
rounding single-rooted teeth (Kaldahl
et al. 1990, Wang et al. 1994, Tomasi
et al. 2007, Ekuni et al. 2009).
The use of locally applied antimi-
crobials as an adjunct to mechanical
debridement may be considered as a
treatment option for these sites.
However, it has been shown that
the association between non-surgical
debridement and the use of different
antimicrobials provides limited or no
additional clinical benefits during the
treatment of class II furcation
involvements (Tonetti et al. 1998, del
Peloso Ribeiro et al. 2006, Danne-
witz et al. 2009, Ribeiro Edel et al.
2010, Tomasi & Wennstr€om 2011).
Thus, alternative anti-infective thera-
peutic strategies in treating class II
furcations are required.
Taking into account promising
outcomes observed with the applica-
tion of PDT in diseased periodontal
sites (Braun et al. 2008, Pinheiro
et al. 2010, Lui et al. 2011, Theod-
oro et al. 2012, Campos et al. 2013),
it could be expected that PDT
adjunctive to periodontal therapy
could yield additional benefits in
treating furcation lesions. To date,
no study has evaluated the clinical
effects of using PDT combined with
conventional periodontal therapy in
the management of molars with class
II furcation defects. Thus, the objec-
tive of this study was to investigate
the clinical, microbiological and
immunological effects of a single
PDT as an adjunct to scaling and
root planing (SRP) in class II furca-
tion sites. We hypothesized that this
therapeutic approach would promote
a better clinical, microbiological and
cytokine profile for the treatment of
furcated molars.
Materials and Methods
Study design
This study was designed as a prospec-
tive, parallel, double-blind, random-
ized, controlled clinical trial (RCT) to
compare the effects of PDT (test
group) with non-activated laser/only
photosensitizer (control group), both
following SRP, for the treatment of
class II furcation sites in chronic peri-
odontitis subjects. The study was
approved by the ethics committee
of Paulista University. All patients
received a detailed description of the
proposed treatment and gave their
informed and written consent.
Population screening
Subject recruitment started in Febru-
ary 2011 and was completed by the
end of August 2011. The clinical
procedures and evaluations were car-
ried out between September 2011
and May 2012. Data entry and sta-
tistical analyses were performed by
the end of July 2012. All patients in
the study were recruited from the
population of patients referred to
Paulista University.
Among the inclusion criteria, sub-
jects had a diagnosis of chronic peri-
odontitis [according to the 1999
international classification criteria
(Armitage1999)] and one buccal or
lingual class II furcation (Hamp et al.
1975) with probing pocket depth
(PPD) ≥ 5 mm and bleeding on prob-
ing (BoP). Exclusion criteria were
pregnancy, lactation, current smoking
and smoking within the past 10 years,
antibiotic therapies in the previous
6 months, use of long-term adminis-
tration of anti-inflammatory and
immunosuppressive medications, use
of mouth rinses containing antimicro-
bials in the preceding 2 months, sys-
temic conditions reported during
anamneses that could affect the pro-
gression of periodontitis (e.g. diabetes
mellitus, unstable or life-threatening
conditions), furcation involvement in
molars with periapical disease or with
signs of mobility and traumatic occlu-
sion, and SRP in the preceding
6 months. All eligible subjects were
thoroughly informed of the nature
and potential risks and benefits of
their participation in the study
and signed their informed consent
documents.
Treatment protocol
Initially, patients were submitted to
dental calculus removal, exodontia,
provisional restorations, and SRP in
all non-experimental sites. The sites
presenting class II furcation lesions
were randomly assigned, by a com-
puter-generated list, to receive PDT
or non-activated laser/only photo-
sensitizer, both following SRP.
The laser system included a hand-
held battery-operated diode laser
(Thera Lase – DMC, S~ao Paulo, Bra-
zil) with a wavelength of 660 nm, a
power output of 60 mW and energy
dose of 129 J/cm2
, together with
methylene blue as a photosensitizer
(10 mg/ml) (Campos et al. 2013).
Photodynamic therapy (test group)
Scaling and root planing was per-
formed using periodontal curettes
(Gracey, Hu-Friedy, Chicago, IL,
USA) and an ultrasonic device (Cavi-
tron, Dentsply, Tulsa, OK, USA)
with specific tips (UI25KSF10S,
Hu-Friedy). Photosensitizer was then
applied to the bottom of the peri-
odontal pocket in a coronal direction.
After 1 min., the pocket was rinsed
with water and subgingivally exposed
to the diode soft laser light using a
corresponding sterile fibre optics
(diameter of 600 lm) which was
applied to the bottom of the peri-
odontal pocket and moved in a coro-
nal direction for 1 min. (Fig. 1a–d).
Non-activated laser/only photosensitizer
(control group)
The same sequence of events des-
cribed for the PDT group sites was
carried out, but the laser was applied
without light activation.
All procedures were performed
under anaesthesia by the same oper-
ator (MFK). The randomization
code was not broken until all data
had been collected.
Sample size calculation
The sample size was calculated using
a = 0.05 and 80% power. For the
variability (r = SD), a value of 1 mm
was used, with clinical attachment
level (CAL) change defined as the pri-
mary outcome variable. The mini-
mum clinically significant value (d)
considered was 1 mm (del Peloso
Ribeiro et al. 2007). It was deter-
mined that a minimum sample of 16
patients per group would be needed.
However, considering that some
patients may be lost during follow-
up, the number of subjects enrolled
per group in this study was 21. The
primary variable, CAL, achieved 0.86
power value with the present data
using the program sample power
SPSS 21 (IBM, Armonk, NY, USA).
© 2013 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd
782 Luchesi et al.
- 3. Clinical parameters
All clinical measurements were evalu-
ated at baseline and at 3 and 6 month
follow-up visits. An individual stent
was made to standardize the loca-
tion of periodontal probe (North
Carolina, Hu-Friedy) to assess the
following parameters: position of the
gingival margin (PGM) – the distance
from the stent to the gingival margin,
relative CAL (RCAL) – the distance
from the stent to the bottom of the
periodontal pocket, and PPD, calcu-
lated by deducting PGM from RCAL
(Fig. 1e). The presence or absence of
BoP at experimental sites was also
assessed, and full-mouth plaque
scores (FMPS) (Ainamo & Bay 1975)
and bleeding scores (FMBS) (Muhle-
mann & Son 1971) were calculated.
The same examiner (VHL), who
was blinded to the therapies, carried
out all measurements of clinical
evaluation. To perform the intra-
examiner calibration, 15 non-study
subjects presenting with furcation
defects were selected. The examiner
measured the RCAL of all patients
twice within 24 h. The examiner was
judged to be reproducible after fulfill-
ing the pre-determined success criteria
(the percentage of agreement within Æ
1 mm between repeated measurements
had to be at least 90%). The intra-
class correlation was calculated as
94% reproducibility.
Microbiological evaluation
Sample collection and real-time PCR
analyses were performed at baseline
and at three and six month re-evalu-
ations Following removal of the su-
pragingival biofilm, the areas
corresponding to furcation defects
were washed with a water spray, iso-
lated with cotton rolls and dried. A
sterile paper point was inserted into
the bottom of the periodontal pocket
for 30 s. The paper points were
placed into sterile tubes containing
300 ll of Tris-EDTA 0.1 mM and
immediately stored at À20°C. One
examiner (VHL) collected all micro-
bial samples. Microbiological assays,
primers and reaction templates were
performed as described previously
(Casarin et al. 2010) to measure the
absolute quantification of Aggrega-
tibacter Actinomycetemcomitans,
Porphyromonas gingivalis and Tanne-
rella forsythia. The level of detection
was set at 103 bacteria per plaque
sample for all target bacteria.
Cytokine profile assessment using
multiplexed bead immunoassay (Luminex)
Gingival crevicular fluid (GCF) was
collected from furcation sites at
baseline and at 3 and 6 month
re-evaluations by the same examiner
(VHL). The area was isolated, dried
and GCF was collected by placing
filter paper strips (Periopaper, Ora-
flow, Plainview, NY, USA) into the
pocket until the clinician perceived a
slight resistance, and then leaving in
place for 15 s. The fluid volume was
measured with a calibrated device
(Periotron 8000, Oraflow). The strips
were placed into sterile tubes con-
taining 400 ll of phosphate-buffered
saline (PBS) with 0.05% Tween-20.
GCF samples were immediately
stored at À20°C until multiplexed
using a bead immunoassay assay.
Cytokine levels [granulocyte-
macrophage colony-stimulating fac-
tor (GM-CSF), interferon (IFN)-c,
interleukin (IL)-10, IL-12, IL-13, IL-
1b,IL-4, IL-6, IL-8 and tumour
necrosis factor (TNF)-a] in GCF were
determined using the high sensitivity
human cytokine 10-plex (Millipore
Corporation, Billerica, MA, USA).
Assays were carried out according to
the manufacturer’s recommendations
using the MAGpixTM
instrument
(MiraiBio, Alameda, CA, USA). The
samples were individually analysed
(each pocket separately), and concen-
trations were estimated from the stan-
dard curve using a five-parameter
polynomial equation using Xponentâ
software (Millipore Corporation). The
mean concentration of each marker
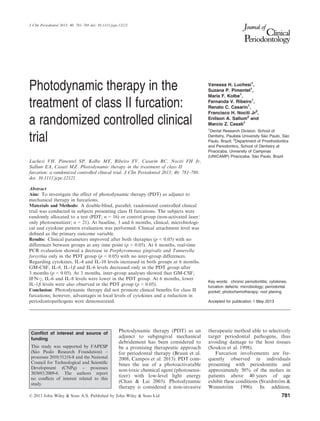
(a) (b)
(c) (d) (e)
Fig. 1. Preoperative clinical view (a) of furcation defect on the buccal aspect of upper
molar. Scaling and root planing at furcation lesion (b) using an ultrasonic device with
specific tips. Application of photosensitizer to the bottom of the periodontal pocket (c).
Exposition of pocket to the diode soft laser light using a corresponding sterile fibre optics
(d). Clinical aspect at 6 months follow-up (e). Note that clinical parameters were mea-
sured using an individual stent made to standardize the location of periodontal probe.
© 2013 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd
Photodynamic therapy in furcations 783
- 4. was calculated using the individual as a
statistical unit and expressed as pg/ml.
Re-assessment evaluations
Re-assessment visits occurred every
15 days during the first month and
monthly until the sixth month. At
the end of each appointment, supra-
gingival prophylaxis was performed.
Primary and secondary outcome
measures
The primary outcome measurement
of the study was RCAL. Secondary
outcomes included (1) PPD, (2)
PGM, (3) BoP at sites, (4) FMPS and
FMBS, (5) cytokine and (6) microbio-
logical levels.
Data management and statistical analysis
The percentage of sites with BoP and
the mean of PPD, RCAL and PGM
were computed for the control and
test groups, separately. Data were
examined for normality using the
Kolmogorov–Smirnov test. Once
normal distribution were obtained,
repeated measures analysis of vari-
ance (ANOVA) and Tukey’s test were
used to detect intra-group and
inter-group differences in clinical
parameters (PGM, PPD and RCAL)
and microbiological data. For non-
normal distribution variables (BoP,
FMPS, FMBS and cytokine levels),
Friedman and Mann–Whitney tests
were, respectively, used to detect
intra-group and inter-group differ-
ences in BoP, FMPS, FMBS and
cytokine levels. Gender and ethnicity
were assessed by Chi-square test. Fur-
cation distribution was assessed by
Fisher’s exact test. Clinical changes
(from baseline to 6 months) of each
group were compared by non-paired
Student’s t-test. An experimental level
of significance was determined at 5%
for all statistical analyses. The biosta-
tician was unaware of the treatment
allocation of the quadrants. Statisti-
cal tests were performed using the
SAS 9.01 program (SAS Institute,
Cary, NC, USA).
Results
Subject accountability
Initially, 21 patients per group were
included in the study. However, five
patients in the test group were lost
during follow-up – three due to
address changes and two due to the
administration of antibiotic medica-
tion for medical reasons. Thus, 21
subjects in the control group and 16
subjects in the test group were
included in the statistical analyses
(Fig. 2). The subjects did not report
adverse effects after therapies.
Clinical outcomes
Patient and furcation defect charac-
teristics for both groups at baseline
are presented at Table 1. Most of fur-
cation lesions were in lower molars
(62.50% and 71.42%, for test and
control groups, respectively). Among
furcations treated at lower molars,
10.00% (test group) and 26.66%
(control group) were buccal and
30.00% (test group) and 13.33%
(control group) were in first molars.
Regarding furcations treated at upper
molars, 50.00% and 16.00%, for
test and control groups, respectively,
were in first molars. No significant
difference were observed between
groups regarding age, gender or fur-
cation distribution (p > 0.05).
The FMPS, FMBS and percentage
of BoP-positive sites are presented in
Table 2. No significant changes from
baseline in FMPS and FMBS were
detected in either group at any time
point (p > 0.05). A significant reduc-
tion in the number of BoP-positive
sites was detected in both test and con-
trol groups at 3 months (p < 0.05). At
6 months, a significant change from
baseline was observed only in the PDT
group (p < 0.05). No significant inter-
group differences were observed for
these parameters at any time point
(p > 0.05).
The means of PPD, RCAL and
PGM at the experimental sites were
not statistically different between
groups at baseline (p > 0.05; Table 3).
At 3 and 6 months, a reduction in
PPD and an increase in RCAL was
observed in both test and control
groups, compared with mean values
Fig. 2. Flowchart of the study.
Table 1. Patient and furcation defect characteristics for both groups at baseline
Test group Control group
Age (years) 50.75 Æ 8.18 50.24 Æ 10.89
Gender (% female) 68.75 71.42
Ethnicity (% caucasian) 81.25 71.43
PPD (mm) 5.53 Æ 1.36 5.14 Æ 1.80
RCAL (mm) 10.56 Æ 1.79 10.43 Æ 2.66
No significant inter-group differences were observed at baseline, p < 0.05.
PPD, probing pocket depth; RCAL, relative clinical attachment level.
© 2013 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd
784 Luchesi et al.
- 5. at baseline (p < 0.05; Table 3). No
inter-group baseline to 6 month-
differences in PPD, RCAL and PGM
were observed (p > 0.05; Table 3).
Cytokine levels
At 3 months post-therapy, lower con-
centrations of pro-inflammatory
GM-CSF, IFN-c, IL-6 and IL-8 were
observed in the PDT group compared
with control group (p < 0.05). In
addition, at 6 months, the levels of
IL-1b were lower in the test group
than the control group (p < 0.05;
Table 4). Inter-group analysis showed
that the levels of anti-inflammatory
IL-4 and IL-10 increased from base-
line in both groups at 6 months post-
therapy, while GM-CSF, IL-8, IL-1b
and IL-6 levels decreased only in the
PDT group at 3 months post-therapy
(p < 0.05; Table 4).
Microbiological assays
Real-time PCR analysis revealed no
significant inter-group differences in
the quantities of A. actinomycetem-
comitans, P. gingivalis and T. for-
sythia at any time point (Table 5). No
significant intra-group differences in
the quantities of A. actinomycetem-
comitans were observed at either 3 or
6 months when compared to baseline
(p > 0.05). Regarding P. gingivalis,
statistically significant reductions
were achieved at 3 months’ follow-up
compared with baseline (p < 0.05) in
both groups, although this reduction
was maintained at 6 months only in
the PDT group (p < 0.05). The T. for-
sythia log concentration was also sta-
tistically reduced in the PDT group
only at 6 months post-therapy
(p < 0.05).
Discussion
The use of PDT in periodontal ther-
apy has demonstrated promising
outcomes in previous studies (Lui
et al. 2011, Theodoro et al. 2012,
Campos et al. 2013); therefore, it is
important to determine the impact
of this therapy during the treatment
of furcation lesions. Thus, the cur-
rent RCT has investigated the role
of PDT combined with non-surgical
mechanical debridement in treating
class II furcation defects.
Earlier research revealed that
PDT in association with non-surgical
debridement achieved higher reduc-
tions in PPD and gains in CAL in
non-furcated teeth (Andersen et al.
2007, Braun et al. 2008). However,
these clinical advantages promoted
by PDT in non-furcated teeth were
not observed in the current trial
which evaluated its effects in class II
furcation sites. In this study, a sig-
nificant mean reduction in PPD of
1.59 mm and a mean CAL gain of
0.78 mm were observed in the test
group, whereas for the control group
the respective numbers were
1.50 mm and 1.00 mm (p > 0.05).
Accordingly, the conservative
therapy of furcation lesions using
non-surgical debridement associated
with local application of antimicro-
bial agents has not provided any evi-
dence of promising clinical outcomes
during initial periodontal therapy or
supportive maintenance care. Tonetti
et al. (1998) did not demonstrate
improvement of CAL after SRP
combined with local controlled drug
delivery with tetracycline fibres dur-
ing SPT in the therapy of class II
furcations. del Peloso Ribeiro et al.
(2006) evaluated the performance of
topically applied polyvinylpyrroli-
done and iodine (PVP-I) adjunctive
to SRP during initial periodontal
therapy of class II furcation involve-
ment. The authors revealed that the
use of PVP-I did not provide any
additional benefits in treating class
II furcation involvements. Danne-
witz et al. (2009) reported that
although doxycycline gel adjunct to
SRP had a short-term effect on fur-
cation lesions at 3 months of follow-
up, it failed to reduce the frequency
of re-instrumentation at furcation
defects at up to 12 months. Tomasi
& Wennstr€om (2011) confirmed that
adjunctive use of locally delivered
doxycycline during SPT failed to
improve the treatment outcome in
furcation involvements.
In this study, the absence of clini-
cal differences between therapies
may be related to the application of
photosensitizer dye in the control
sites, which could have optimized
the clinical outcomes in the control
Table 2. Percentages of FMPS, FMBS and BoP at experimental sites at baseline, 3 and
6 months
Parameter Group Baseline 3 months 6 months
FMPS (mean Æ SD) Test 25.14 Æ 31.06 24.53 Æ 23.56 16.42 Æ 13.81
Control 31.74 Æ 32.82 26.31 Æ 20.33 24.11 Æ 18.15
FMBS (mean Æ SD) Test 35.89 Æ 23.82 27.28 Æ 13.68 27.56 Æ 11.20
Control 38.60 Æ 21.28 27.53 Æ 17.30 28.63 Æ 12.03
BoP Test 100 31.25* 37.50*
Control 100 42.85* 55.00
*Indicates difference from baseline by Friedman test, p < 0.05. No significant inter-group
differences were observed from the Mann–Whitney test, p > 0.05.
SD, standard deviation; FMPS, full mouth plaque score; FMBS, full mouth bleeding score;
BoP, bleeding on probing.
Table 3. Mean (ÆSD) of PPD, RCAL and PGM at baseline, 3 and 6 months
Test group Control group
Baseline 3 months 6 months 0–6 months
difference
Baseline 3 months 6 months 0–6 months
difference
PPD (mm) 5.53 Æ 1.36 4.06 Æ 1.12* 3.94 Æ 1.61* 1.59 Æ 1.11 5.14 Æ 1.80 3.81 Æ 1.12* 3.65 Æ 1.39* 1.50 Æ 1.73
RCAL (mm) 10.56 Æ 1.79 9.97 Æ 1.68* 9.78 Æ 2.33* 0.78 Æ 1.54 10.43 Æ 2.66 9.71 Æ 1.79* 9.50 Æ 2.14* 1.00 Æ 1.69
PGM (mm) 5.03 Æ 0.94 5.91 Æ 1.19* 5.84 Æ 1.26* À0.81 Æ 1.05 5.29 Æ 1.45 5.90 Æ 1.51* 5.85 Æ 1.46* À0.50 Æ 1.00
*Indicates difference from baseline by ANOVA/Tukey’s test, p < 0.05. No significant inter-group differences were observed by ANOVA/Tukey’s
test, p > 0.05.
SD, standard deviation; PPD, periodontal probing depth; RCAL, relative clinical attachment level; PGM, position of the gingival margin.
© 2013 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd
Photodynamic therapy in furcations 785
- 6. group, contrary to other previous
investigations in the literature
(Andersen et al. 2007, de Oliveira
et al. 2007, Braun et al. 2008,
Christodoulides et al. 2008) that
compared the performance of PDT
plus SRP with the use of mechanical
debridement alone. It should be
pointed out that the photosensitizer
alone can also exhibit bactericidal
action (Usacheva et al. 2001, 2003a,
b). Wilson et al. (1992) revealed that
the subgingival application of methy-
lene blue as monotherapy in sites
with chronic periodontitis achieved
superior benefits in microbiological
parameters when compared to con-
trol sites that received sterile water.
Another investigation also demon-
strated that the application of tolui-
dine blue O (TBO) alone resulted in
a significant reduction in periodonto-
pathogens on contaminated dental
implant surfaces (Dortbudak et al.
2001).
However, it may be hypothesized
that the maintenance of reduced lev-
els of periodontopathogens through-
out the re-evaluation period is
dependent upon the PDT approach,
as revealed in the outcomes of the
present trial. In terms of a reduction
in P. gingivalis and T. forsythia,
advantages were observed for the
PDT group. It was shown that the
T. forsythia decrease from baseline
was achieved only in the PDT
group, 6 months after therapy. In
addition, although a decline in the
levels of P. gingivalis from baseline
was observed after 3 months for
both treatments, this reduction
remained until 6 months post-therapy
only in the PDT group.
These changes in microbiological
profile in the test group are in line
with the reduction in BoP at these
sites. In this study, the significant
reduction in BoP-positive sites
detected for both therapies at
3 months was only maintained with
lower levels at 6 months in the PDT
group. BoP is a relevant outcome
parameter since the absence of BoP
in maintenance patients has been
associated with successful clinical
stability over time (Lang et al.
1990). In line with the outcomes
obtained in the current trial, Chond-
ros et al. (2009) also showed that
the combination of PDT with non-
surgical therapy promoted a higher
reduction in BoP scores compared
with non-surgical debridement used
alone during SPT.
In fact, researchers have pointed
out the effect of low-level energy
lasers on cells and tissues, an effect
known as “photobiomodulation”.
The light has a positive influence on
the surrounding tissues and cells
during tissue healing, successfully
influencing the repair of tissues and
diminishing periodontal inflamma-
tion as a result of the potential bio-
modulatory effects (Woodruff et al.
2004, Qadri et al. 2005). These posi-
tive effects associated with laser use
may have contributed to a reduction
in BoP at furcation sites treated by
PDT throughout the present investi-
gation. These biomodulatory effects
of PDT may be related to the posi-
tive outcomes observed in this study
concerning the levels of key markers
that regulate the immune response
and bone metabolism.
Overall, it was demonstrated that
PDT achieved improvements in mod-
ulating the local levels of inflamma-
tory mediators throughout 6 months
of follow-up. Although both thera-
peutic approaches have achieved
increased levels of anti-inflammatory
IL-4 and IL-10 at 6 months post-
therapy, only the test group yielded
lower levels of the pro-inflammatory
GM-CSF, IL-8, IL-1b and IL-6 after
3 months when compared to baseline
levels. In addition, the amounts of
Table4.Mean(ÆSD)ofconcentrations(pg/ll)ofmediatorsforbothgroupsatbaseline,andat3and6monthspost-therapy
GroupPeriodGM-CSFIFNcIL-10IL-12IL-13IL-1bIL-4IL-6IL-8TNFa
TestBaseline0.17Æ0.300.26Æ0.450.19Æ0.230.15Æ0.250.04Æ0.0810.20Æ11.401.22Æ2.241.24Æ1.47312.30Æ733.450.11Æ0.17
3months0.06Æ0.100.13Æ0.180.17Æ0.250.11Æ0.130.01Æ0.026.82Æ8.42†
1.03Æ1.170.52Æ0.73†
78.46Æ106.74†
0.12Æ0.20
6months0.23Æ0.20‡
0.26Æ0.280.58Æ0.98†
0.22Æ0.250.04Æ0.076.81Æ8.302.30Æ2.94†,‡
1.39Æ1.97217.17Æ216.510.24Æ0.30
ControlBaseline0.11Æ0.130.17Æ0.210.22Æ0.320.10Æ0.090.03Æ0.038.20Æ15.120.91Æ1.111.95Æ2.70220.30Æ260.520.13Æ0.18
3months0.13Æ0.15*0.54Æ0.90*0.52Æ1.200.16Æ0.180.03Æ0.037.85Æ8.951.82Æ2.63†
1.35Æ1.54*177.70Æ180.92*0.13Æ0.13
6months0.26Æ0.350.35Æ0.350.60Æ0.66†
0.19Æ0.180.08Æ0.0910.35Æ8.43*2.23Æ2.52†
2.33Æ5.29252.92Æ264.830.25Æ0.30
*Representssignificantinter-groupdifferencesbyMann–Whitneytest,p<0.05.
†
Representssignificantintra-groupdifferencesfrombaselinebyFriedmantest,p<0.05.
‡
Representssignificantintra-groupdifferencesfrom3monthsbyFriedmantest,p<0.05.
GM-CSF,granulocyte-macrophagecolony-stimulatingfactor;IFN-c,interferon;IL-10,-12,-13,-1b,-4,-6,-8,interleukin;TNF-a,tumournecrosisfactor.
Table 5. Amount (log10 Æ SEM) of Aggregatibacter actinomycetemcomitans, Porphyromon-
as gingivalis and Tannerella forsythia at baseline, 3 and 6 months
Bacteria Group Baseline 3 months 6 months
Aa Test 2.96 Æ 3.25 2.92 Æ 3.03 1.61 Æ 2.55
Control 2.51 Æ 3.76 2.66 Æ 3.71 1.91 Æ 2.89
Pg Test 2.38 Æ 3.00 1.48 Æ 2.69* 1.56 Æ 2.69*
Control 2.59 Æ 3.11 1.70 Æ 2.77* 2.38 Æ 2.88
Tf Test 6.46 Æ 1.86 6.01 Æ 1.70 4.86 Æ 2.94*
Control 6.39 Æ 1.70 6.14 Æ 1.86 6.17 Æ 1.70
*Indicates statistical difference from baseline by ANOVA/Tukey’s test, p < 0.05. No significant
inter-group differences were observed by ANOVA, p < 0.05.
© 2013 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd
786 Luchesi et al.
- 7. GM-CSF, IFN-c, IL-6 and IL-8 were
lower for the test group at 3 months
when compared to the control group;
inferior levels of IL-1b were also
achieved in this group at 6 months
post-therapy.
Scarce and contradictory data are
available concerning the role of PDT
in the immune inflammatory media-
tor profile during periodontal ther-
apy. The levels of inflammatory
markers in the GCF of patients with
aggressive periodontitis 3 months
after PDT or SRP were evaluated by
de Oliveira et al. (2009). Both thera-
pies presented reductions in TNF-a
levels and no change in the receptor
activator of NF-kB ligand (RANKL)
levels over time, with no significant
differences between groups for any
marker. Accordingly, no differences
in the reduction in gene expression
of TNF-a, RANKL, osteoprotegerin,
matrix metalloproteinase (MMP-1),
IL-6 and IL-10 were observed in gin-
gival biopsies from dogs with induced
periodontitis treated by PDT, SRP or
PDT combined with SRP (de Oliveira
et al. 2011). Recently, Giannopoulou
et al. (2012), comparing the effects
of PDT, diode soft laser or SRP on
local levels of several cytokines and
acute-phase proteins in the therapy of
residual pockets, revealed that signifi-
cant changes were achieved regardless
of treatment modality throughout
6 months. However, no differences
were observed among the three treat-
ment modalities at any time point.
Conversely, previous findings
have suggested that PDT leads to an
immunomodulatory activity, decreas-
ing the stimulation of T lymphocytes
(King et al. 1999) and inactivating
key pro-inflammatory markers as
IL-1b and TNF-a (Braham et al.
2009). The capacity of PDT to mod-
ulate the host response seems to be
related to its ability to influence the
immunostimulatory attributes of
antigen-presenting cells (Levy 1998,
Seguier et al. 2010). In line, Seguier
et al. (2010) revealed that, 7 days
after PDT, the number of inflamma-
tory cell populations was reduced
during chronic periodontitis. Fur-
ther, Carvalho et al. (2011), in a rat
model of experimental periodontitis,
demonstrated that PDT-treated
animals presented decreased bone
resorption, as well as reduced neu-
trophil migration and lower TNF-a
expression, compared with animals
treated with photosensitizer alone,
which is in agreement with the
results presented here.
An important aspect to be dis-
cussed in the current trial is the
number of PDT episodes. This study
used a single PDT application as
adjunct to mechanical therapy and
this approach did not provide clini-
cal benefits for the treated sites in
terms of PPD reduction or CAL
gain. Conversely, Lulic et al. (2009)
revealed that additional PDT ses-
sions after non-surgical therapy pro-
vided benefits in clinical outcomes in
residual pockets during supportive
periodontal treatment, supporting
the use of repeated PDT applica-
tions. It may be speculated that the
effects of single-episode adjunctive
PDT, as performed in this study,
may not be sufficient to contribute
to clinical improvements in furcation
lesions. Future investigations are
needed to elucidate if multiple
courses of PDT may improve treat-
ment outcomes.
It should be kept in mind that
there are no data in the literature
from controlled clinical trials evalu-
ating the performance of PDT in
combination with SRP to treat
class II furcations. Thus, considering
the limitations of the therapeutic
approaches studied until now to
manage furcation sites, further stud-
ies with more longitudinal follow-up
periods are required. These locally
applied therapies in combination
with SRP could be an important and
safe strategy in treating furcation
involvements, representing an alter-
native to conventional chemothera-
pies even tested in this type of
periodontal defect. In addition, it is
essential to mention that topical
therapeutic strategies have several
advantages compared with the use of
systemic antibiotics as adjunctive
therapy. Negative aspects concerning
systemic antimicrobial usage in the
treatment of periodontally diseased
sites should be taken into account:
in particular, side-effects for individ-
ual patients such as gastrointestinal
disorders, as well as the development
of bacterial resistance, which is an
important global public health prob-
lem. In addition, based on these rea-
sons, patient compliance may also be
jeopardized.
In conclusion, PDT as an adjunct
to mechanical periodontal therapy
does not provide additional clinical
improvements in the treatment of
class II furcation lesions. However,
only PDT has yielded advantages in
the reduction in P. gingivalis and
T. forsythia and, moreover, this
therapeutic approach may reduce
levels of pro-inflammatory cytokines
GM-CSF, IFN-c, IL-1b, IL-6 and
IL-8 when compared with control
therapy.
References
Ainamo, J. Bay, I. (1975) Problems and pro-
posals for recording gingivitis and plaque.
International Dental Journal 25, 229–235.
Andersen, R., Loebel, N., Hammond, D.
Wilson, M. (2007) Treatment of periodontal
disease by photodisinfection compared to
scaling and root planing. Journal of Clinical
Dentistry 18, 34–38.
Armitage, G. C. (1999) Development of a classifi-
cation system for periodontal diseases and
conditions. Annals of Periodontology 4, 1–6.
Braham, P., Herron, C., Street, C. Darveau,
R. (2009) Antimicrobial photodynamic therapy
may promote periodontal healing through mul-
tiple mechanisms. Journal of Periodontology 80,
1790–1798.
Braun, A., Dehn, C., Krause, F. Jepsen, S.
(2008) Short-term clinical effects of adjunctive
antimicrobial photodynamic therapy in peri-
odontal treatment: a randomized clinical
trial. Journal of Clinical Periodontology 35,
877–884.
Campos, G. N., Pimentel, S. P., Ribeiro, F. V.,
Casarin, R. C., Cirano, F. R., Saraceni, C. H.
Casati, M. Z. (2013) The adjunctive effect of
photodynamic therapy for residual pockets in
single-rooted teeth: a randomized controlled
clinical trial. Lasers in Medical Science 28,
317–324.
Carvalho, A. S., Napimoga, M. H., Coelho-
Campos, J., Silva-Filho, V. J. Thedei, G. (2011)
Photodynamic therapy reduces bone resorption
and decreases inflammatory response in an
experimental rat periodontal disease model.
Photomedicine and Laser Surgery 29, 735–740.
Casarin, R. C., Ribeiro Edel, P., Mariano, F. S.,
Nociti, F. H. Jr, Casati, M. Z. Goncßalves,
R. B. (2010) Levels of Aggregatibacter actino-
mycetemcomitans, Porphyromonas gingivalis,
inflammatory cytokines and species-specific
immunoglobulin G in generalized aggressive
and chronic periodontitis. Journal of Periodon-
tal Research 45, 635–642.
Chan, Y. Lai, C. H. (2003) Bactericidal effects
of different laser wavelengths on periodonto-
pathic germs in photodynamic therapy. Lasers
in Medical Science 18, 51–55.
Chondros, P., Nikolidakis, D., Christodoulides,
N., R€ossler, R., Gutknecht, N. Sculean, A.
(2009) Photodynamic therapy as adjunct to
non-surgical periodontal treatment in patients
on periodontal maintenance: a randomized
controlled clinical trial. Lasers in Medical
Science 24, 681–688.
Christodoulides, N., Nikolidakis, D., Chondros,
P., Becker, J., Schwarz, F., R€ossler, R.
Sculean, A. (2008) Photodynamic therapy as an
adjunct to non-surgical periodontal treatment:
a randomized, controlled clinical trial. Journal
of Periodontology 79, 1638–1644.
© 2013 John Wiley Sons A/S. Published by John Wiley Sons Ltd
Photodynamic therapy in furcations 787
- 8. Dannewitz, B., Lippert, K., Lang, N. P., Tonetti,
M. S. Eickholz, P. (2009) Supportive
periodontal therapy of furcation sites: non-
surgical instrumentation with or without topical
doxycycline. Journal of Clinical Periodontology
36, 514–522.
Dortbudak, O., Haas, R., Bernhart, T.
Mailath-Pokorny, G. (2001) Lethal photosensi-
tization for decontamination of implant sur-
faces in the treatment of peri-implantitis.
Clinical Oral Implants Research 12, 104–108.
Ekuni, D., Yamamoto, T. Takeuchi, N. (2009)
Retrospective study of teeth with a poor prog-
nosis following non-surgical periodontal treat-
ment. Journal of Clinical Periodontology 36,
343–348.
Giannopoulou, C., Cappuyns, I., Cancela, J.,
Cionca, N. Mombelli, A. (2012) Effect of
photodynamic therapy, diode laser, and deep
scaling on cytokine and acute-phase protein
levels in gingival crevicular fluid of residual
periodontal pockets. Journal of Periodontology
8, 1018–1027.
Hamp, S. E., Nyman, S. Lindhe, J. (1975) Peri-
odontal treatment of multi-rooted teeth.
Results after 5 years. Jounal of Clinical Peri-
odontology 2, 126–135.
Kaldahl, W. B., Kalkwarf, K. L., Patil, K. D.
Molvar, M. P. (1990) Responses of four tooth
and site groupings to periodontal therapy.
Journal of Periodontology 61, 173–179.
King, D. E., Jiang, H., Simkin, G. O., Obochi,
M. O., Levy, J. G. Hunt, D. W. (1999) Pho-
todynamic alteration of the surface receptor
expression pattern of murine splenic dendritic
cells. Scandinavian Journal of Immunology 49,
184–192.
Lang, N. P., Adler, R., Joss, A. Nyman, S.
(1990) Absence of bleeding on probing. An
indicator of periodontal stability. Journal of
Clinical Periodontology 17, 714–721.
Levy, J. G. (1998) Immunomodulatory aspects of
photodynamic therapy. Expert Opinion on
Investigational Drugs 7, 57–64.
Lui, J., Corbet, E. F. Jin, L. (2011) Combined
photodynamic and low-level laser therapies as
an adjunct to nonsurgical treatment of chronic
periodontitis. Journal of Periodontal Reseach
46, 89–96.
Lulic, M., Leiggener Gorog, I., Salvi, G. E.,
Ramseier, C. A., Mattheos, N. Lang, N. P.
(2009) One-year outcomes of repeated adjunc-
tive photodynamic therapy during periodontal
maintenance: a proof-of-principle randomized-
controlled clinical trial. Journal of Clinical Peri-
odontology 36, 661–666.
Muhlemann, H. R. Son, S. (1971) Gingival sul-
cus bleeding – A leading symptom in initial
gingivitis. Helvetica Odontol Acta 15, 107–113.
de Oliveira, R. R., Schwartz-Filho, H. O.,
Novaes, A. B. Jr Taba, M. Jr (2007) Antimi-
crobial photodynamic therapy in the non-surgi-
cal treatment of aggressive periodontitis: a
preliminary randomized controlled clinical
study. Journal of Periodontology 78, 965–973.
de Oliveira, R. R., Novaes, A. B. Jr, Garlet, G.
P., de Souza, R. F., Taba, M. Jr, Sato, S., de
Souza, S. L., Palioto, D. B., Grisi, M. F.
Feres, M. (2011) The effect of a single episode
of antimicrobial photodynamic therapy in the
treatment of experimental periodontitis. Micro-
biological profile and cytokine pattern in the
dog mandible. Lasers in Medical Science 26,
359–367.
de Oliveira, R. R., Schwartz-Filho, H. O., Nov-
aes, A. B., Garlet, G. P., de Souza, R. F.,
Taba, M., Scombatti de Souza, S. L. Ribe-
iro, F. J. (2009) Antimicrobial photodynamic
therapy in the non-surgical treatment of aggres-
sive periodontitis: cytokine profile in gingival
crevicular fluid, preliminary results. Journal of
Periodontology 80, 98–105.
del Peloso Ribeiro, E., Bittencourt, S., Ambrosa-
no, G. M., Nociti, F. H. Jr, Sallum, E. A.,
Sallum, A. W. Casati, M. Z. (2006) Povi-
done-iodine used as an adjunct to non-surgical
treatment of furcation involvements. Journal of
Periodontology 77, 211–217.
del Peloso Ribeiro, E., Bittencourt, S., Nociti, F.
H. Jr, Sallum, E. A., Sallum, A. W. Casati,
M. Z. (2007) Comparative study of ultrasonic
instrumentation for the non-surgical treatment
of interproximal and non-interproximal furca-
tion involvements. Journal of Periodontology
78, 224–230.
Pinheiro, S.L, Donega, J.M, Seabra, L.M, Adabo,
M.D, Lopes, T., do Carmo, T.H, Ribeiro, M.C
Bertolini, P.F. (2010) Capacity of photody-
namic therapy for microbial reduction in peri-
odontal pockets. Lasers in Medical Science 25,
87–91.
Qadri, T., Miranda, L., Tuner, J. Gustafsson,
A. (2005) The short-term effect of low-level
laser as adjunct therapy in the treatment of
periodontal inflammation. Journal of Clinical
Periodontology 32, 714–719.
Ribeiro Edel, P., Bittencourt, S., Sallum, E. A.,
Sallum, A.W., Nociti, F. H. Jr Casati, M. Z.
(2010) Non-surgical instrumentation associated
with povidone-iodine in the treatment of inter-
proximal furcation involvements. Journal of
Applied Oral Science 18, 599–606.
Seguier, S., Souza, S. L., Sverzut, A. C., Simioni,
A. R., Primo, F. L., Bodineau, A., Corr^ea, V.
M., Coulomb, B. Tedesco, A. C. (2010)
Impact of photodynamic therapy on inflamma-
tory cells during human chronic periodontitis.
Journal of Photochemistry and Photobiology.B,
101, 348–354.
Soukos, N. S., Ximenez-Fyvie, L. A., Hamblin,
M. R., Socransky, S. S. Hasan, T. (1998)
Targeted Antimicrobial Photochemotherapy.
Antimicrobial Agent and Chemotherapy 42,
2595–2601.
Svardstr€om, G. Wennstr€om, J. L. (1996) Preva-
lence of furcation involvements in patients
referred for periodontal treatment. Journal of
Clinical Periodontology 23, 1093–1099.
Theodoro, L. H., Silva, S. P., Pires, J. R., Soares,
G. H., Pontes, A. E., Zuza, E. P., Spolidorio,
D. M., de Toledo, B. E. Garcia, V. G.
(2012) Clinical and microbiological effects of
photodynamic therapy associated with nonsur-
gical periodontal treatment. A 6-month follow-
up. Lasers in Medical Science 27, 687–693.
Tomasi, C., Leyland, A. H. Wennstr€om, J. L.
(2007) Factors influencing the outcome of non-
surgical periodontal treatment: a multilevel
approach. Journal of Clinical Periodontology
34, 682–690.
Tomasi, C. Wennstr€om, J. L. (2011) Locally
delivered doxycycline as an adjunct to mechani-
cal debridement at retreatment of periodontal
pockets: outcome at furcation sites. Journal of
Periodontology 82, 210–218.
Tonetti, M. S., Cortellini, P., Carnevale, G.,
Cattabriga, M., de Sanctis, M. Pini Prato,
G. P. (1998) A controlled multicenter study of
adjunctive use of tetracycline periodontal fibers
in mandibular class II furcations with persistent
bleeding. Journal of Clinical Periodontology 25,
728–736.
Usacheva, M. N., Teichert, M. C. Biel, M. A.
(2001) Comparison of the methylene blue and
toluidine blue photobactericidal efficacy against
Gram-positive and Gram-negative microorgan-
isms. Lasers in Surgery and Medicine 29,
165–173.
Usacheva, M. N., Teichert, M. C. Biel, M. A.
(2003a) The interaction of lipopolysaccharides
with phenothiazine dyes. Lasers in Surgery and
Medicine 33, 311–319.
Usacheva, M. N., Teichert, M. C. Biel, M. A.
(2003b) The role of the methylene blue and
toluidine blue monomers and dimers in the
photoinactivation of bacteria. Journal of Photo-
chemistry and Photobiology 71, 87–98.
Wang, H. L., Burgett, F. G., Shjr, Y. Ramfj-
ord, S. (1994) The influence of molar furcation
involvement and mobility on future clinical
periodontal attachment loss. Journal of Peri-
odontology 65, 25–29.
Wilson, M., Gibson, M., Strahan, D. Harvey,
W. (1992) A preliminary evaluation of the use
of a redox agent in the treatment of chronic
periodontitis. Journal of Periodontal Research
27, 522–527.
Woodruff, L. D., Bounkeo, J. M., Brannnon, W.
M., Dawes, K. D., Barham, C. D., Waddell,
D. L. Enwemeka, C. S. (2004) The efficacy
of laser therapy in wound repair: a meta-analy-
sis of the literature. Photomedicine and Laser
Surgery 22, 241–247.
Address:
Marcio Zaffalon Casati
Depto de Odontologia, Universidade
Paulista – UNIP, Av. Dr. Bacelar, 1212,
4o andar, Vila Clementino, 04026-002
S~ao Paulo, Brazil.
E-mail: mzcasati@gmail.com
Clinical Relevance
Scientific rationale for the study:
Furcation involvements represent a
clinical challenge. PDT has demon-
strated promising outcomes in peri-
odontal therapy. Thus, it would be
relevant to determine the impact of
PDT with scaling and root planing
(SRP) in the treatment of furcation
lesions.
Principal findings: Clinical improve-
ments after non-surgical therapy were
not enhanced by PDT. However, PDT
promoted advantages in local levels of
cytokines and was associated with a
reduction in red complex species.
Practical implications: PDT as an
adjunct to SRP may modulate
the host immune inflammatory
response and reduce periodonto-
pathogens, although this approach
did not provide additional clinical
benefits in the treatment of class II
furcations.
© 2013 John Wiley Sons A/S. Published by John Wiley Sons Ltd
788 Luchesi et al.