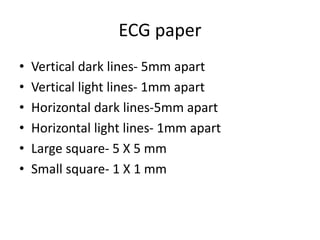
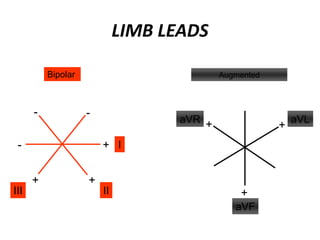
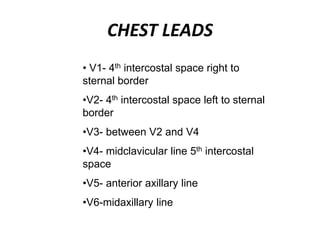
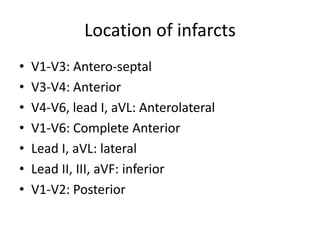
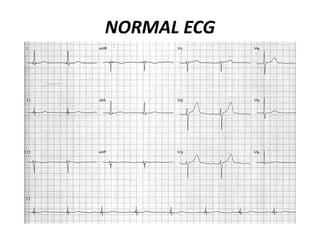
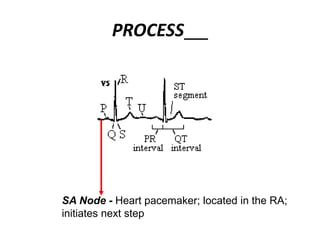
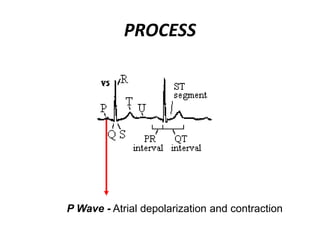
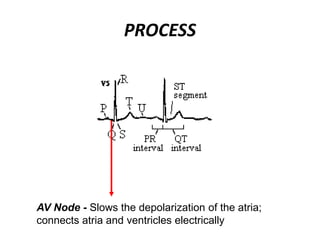
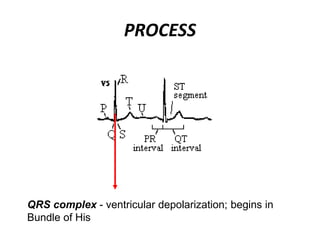
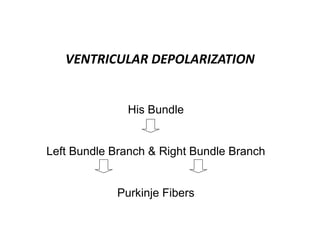
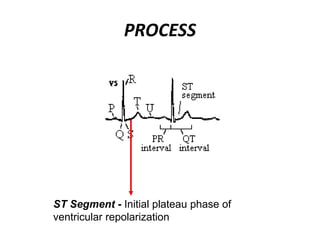
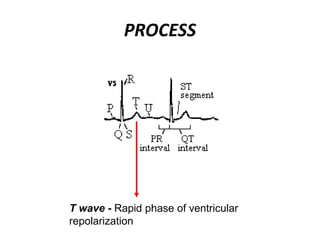
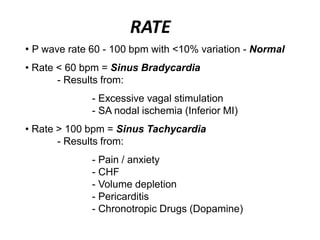
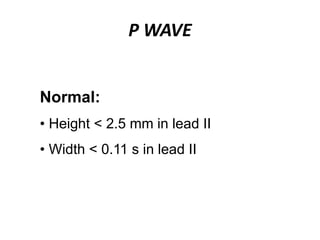
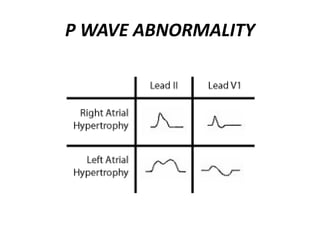
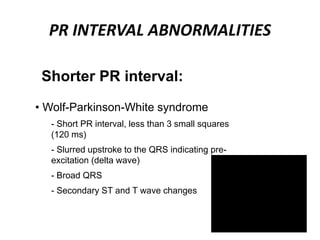
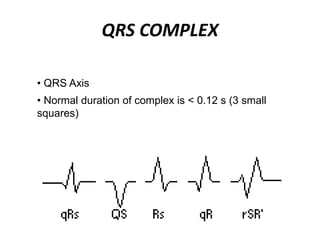
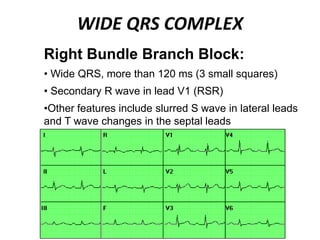
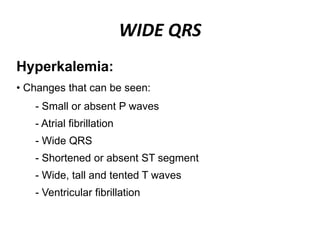
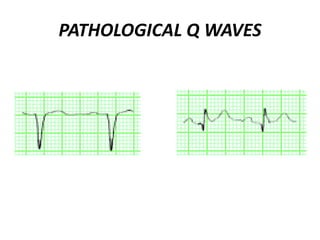
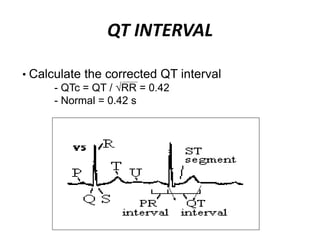
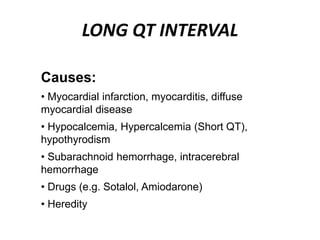
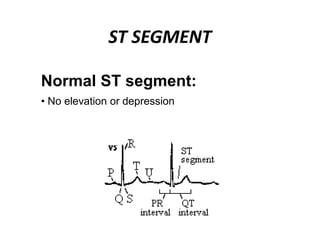
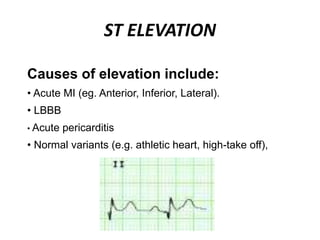
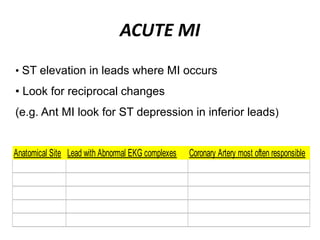
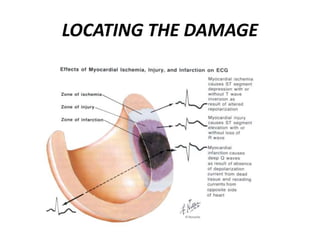
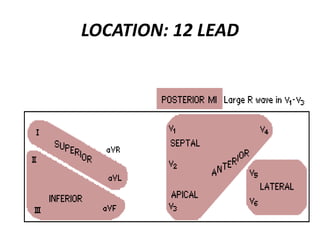
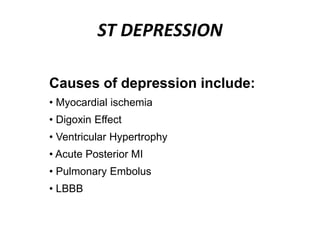
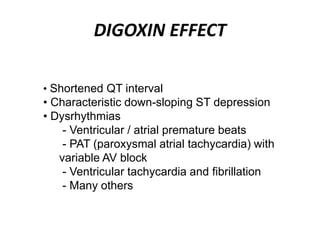
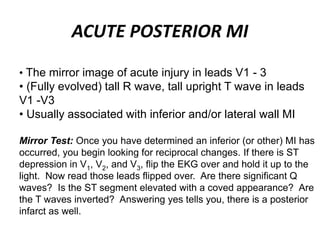
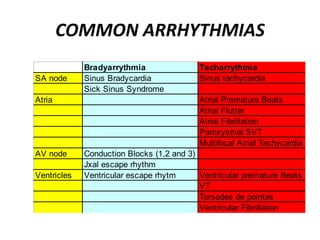
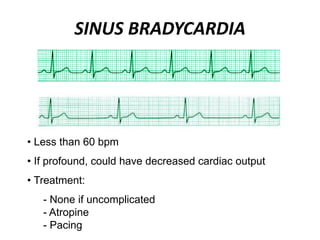
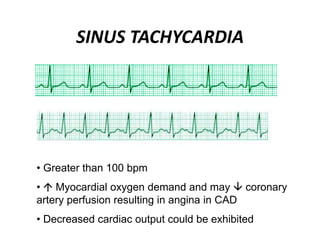
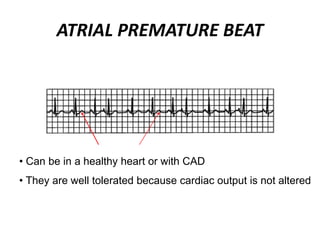
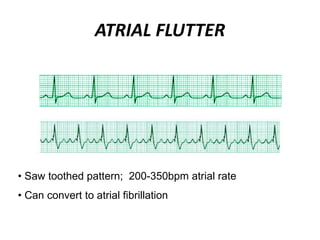
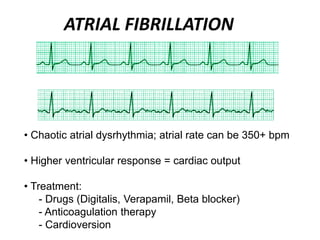
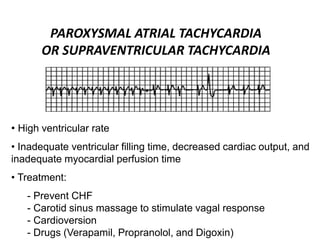
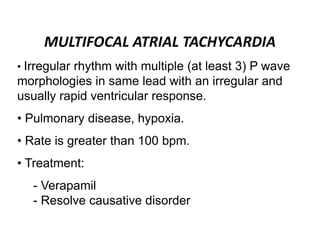
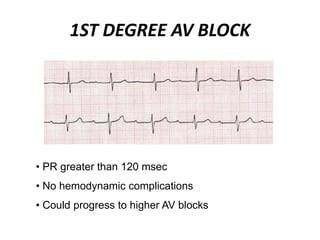
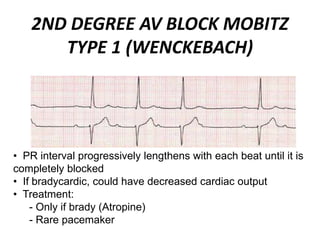
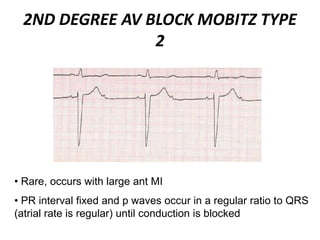
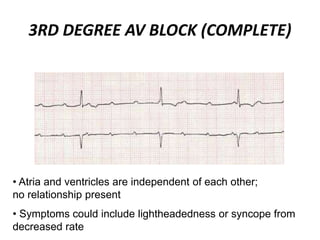
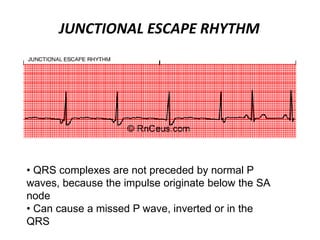
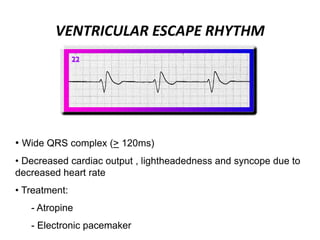
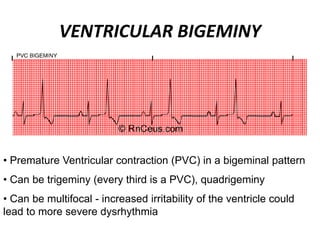
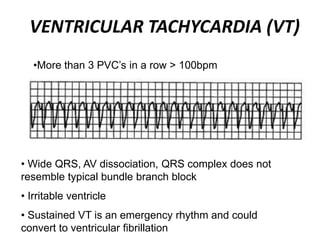
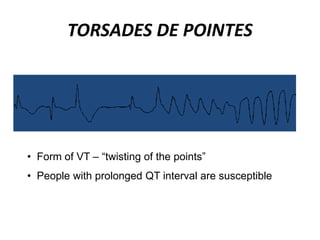
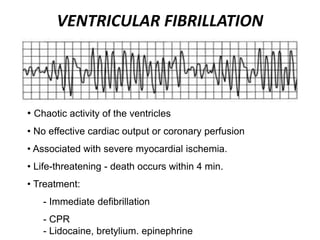
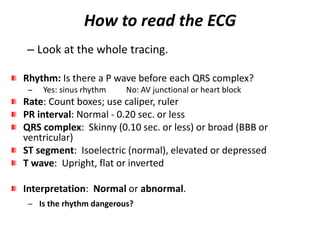
This document provides information on electrocardiograms (ECGs), including ECG paper layout, lead placement, interpretation steps, and how to locate infarcts based on ECG findings. Common arrhythmias are summarized, including definitions and treatments for sinus bradycardia, atrial fibrillation, heart blocks, premature ventricular contractions, ventricular tachycardia, and more. Overall health impacts and treatments are discussed for various rhythms.