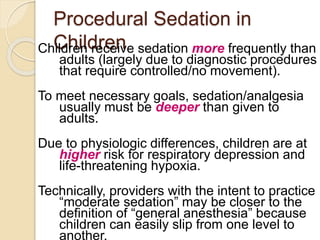
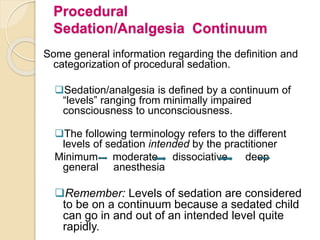
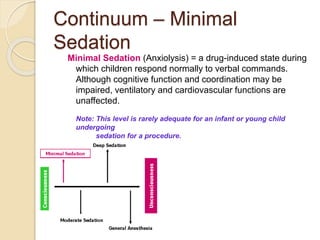
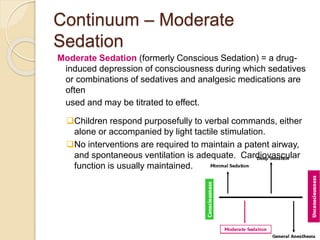
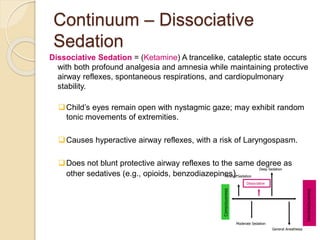
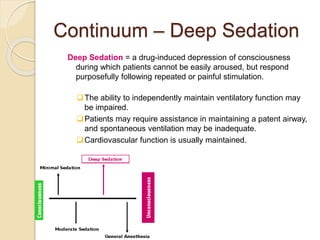
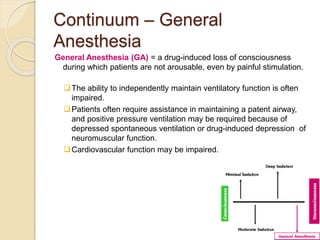
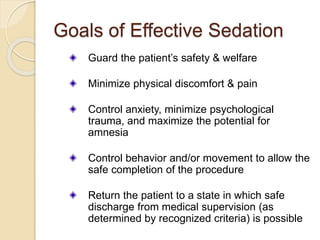
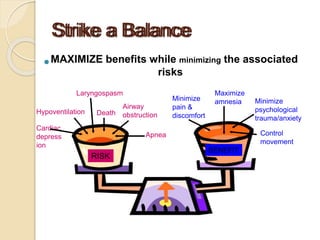
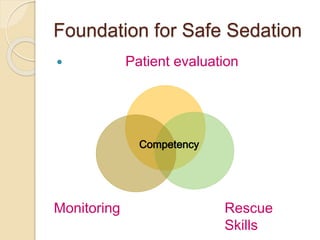
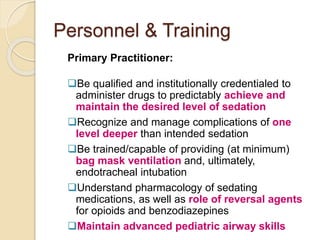
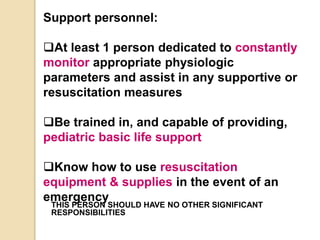
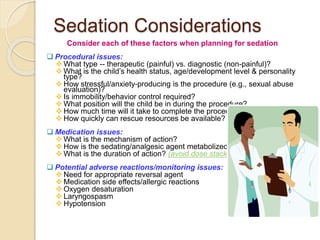
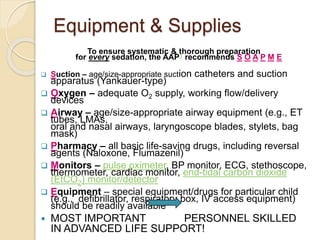
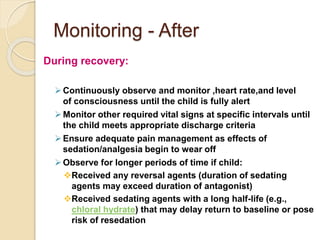
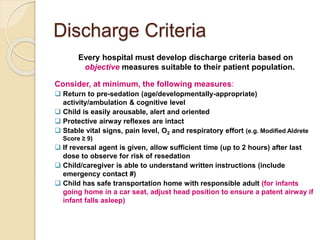
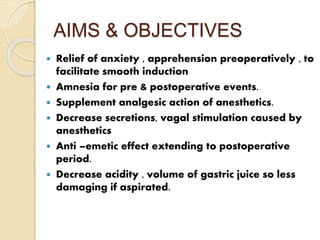
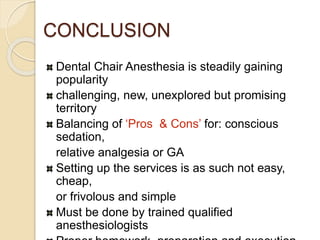
This document discusses principles of conscious sedation for pediatric patients. It begins by introducing conscious sedation and its increasing use for painful procedures in non-traditional settings. The purpose is to familiarize providers with standards for safe and effective pediatric moderate sedation. Key points discussed include: the procedural sedation continuum; increased risks for children requiring deeper sedation than adults; importance of patient evaluation, monitoring, and rescue skills; and guidance on supervision, staffing, equipment and disposition for safe sedation. Specific considerations are outlined for sedation agents, levels of practitioner training, and factors to consider for each sedation case.