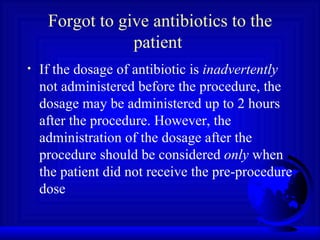
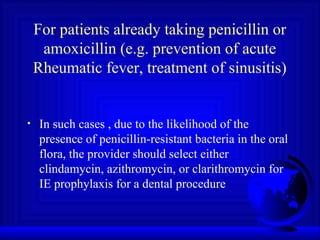
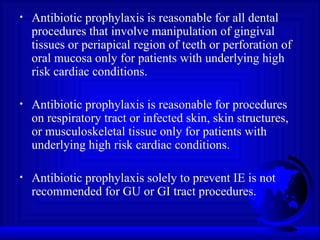
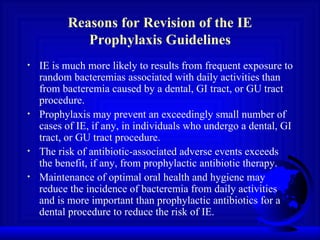
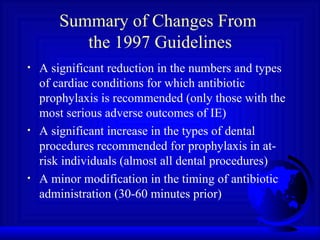
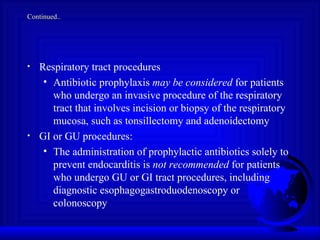
The document summarizes changes over time to guidelines from the American Heart Association regarding antibiotic prophylaxis for infective endocarditis. The key changes are: (1) prophylaxis is now only recommended for those cardiac conditions with the most serious outcomes from IE, (2) prophylaxis is recommended for almost all dental procedures for at-risk individuals, and (3) timing of antibiotics is 30-60 minutes before a procedure rather than both before and after. Prophylaxis is no longer routinely recommended for other conditions, gastrointestinal/genitourinary procedures, or daily activities that may cause minor bacteremia, as the risks of antibiotics outweigh the small potential benefits of prevention in those cases.


![Cardiac Conditions for Which Prophylaxis of IE is Recommended Prosthetic cardiac valve Previous infective endocarditis Congenital heart disease (CHD) [except for the conditions listed below, Antibiotic prophylaxis is no longer recommended for any other form of CHD] Unrepaired cyanotic CHD, including those with palliative shunts and conduits Completely repaired CHD with prosthetic material or device either by surgery or catheter intervention during first 6 months after procedure (to allow time for endothelial covering of the material) Repaired CHD with residual defects at the site or adjacent to the site of a prosthetic patch or prosthetic device which inhibits endothelialization Cardiac transplantation recipients who develop cardiac valvulopathy](https://image.slidesharecdn.com/infectiveendocarditisprophylaxis-100620065946-phpapp01/85/Infective-endocarditis-prophylaxis-7-320.jpg)