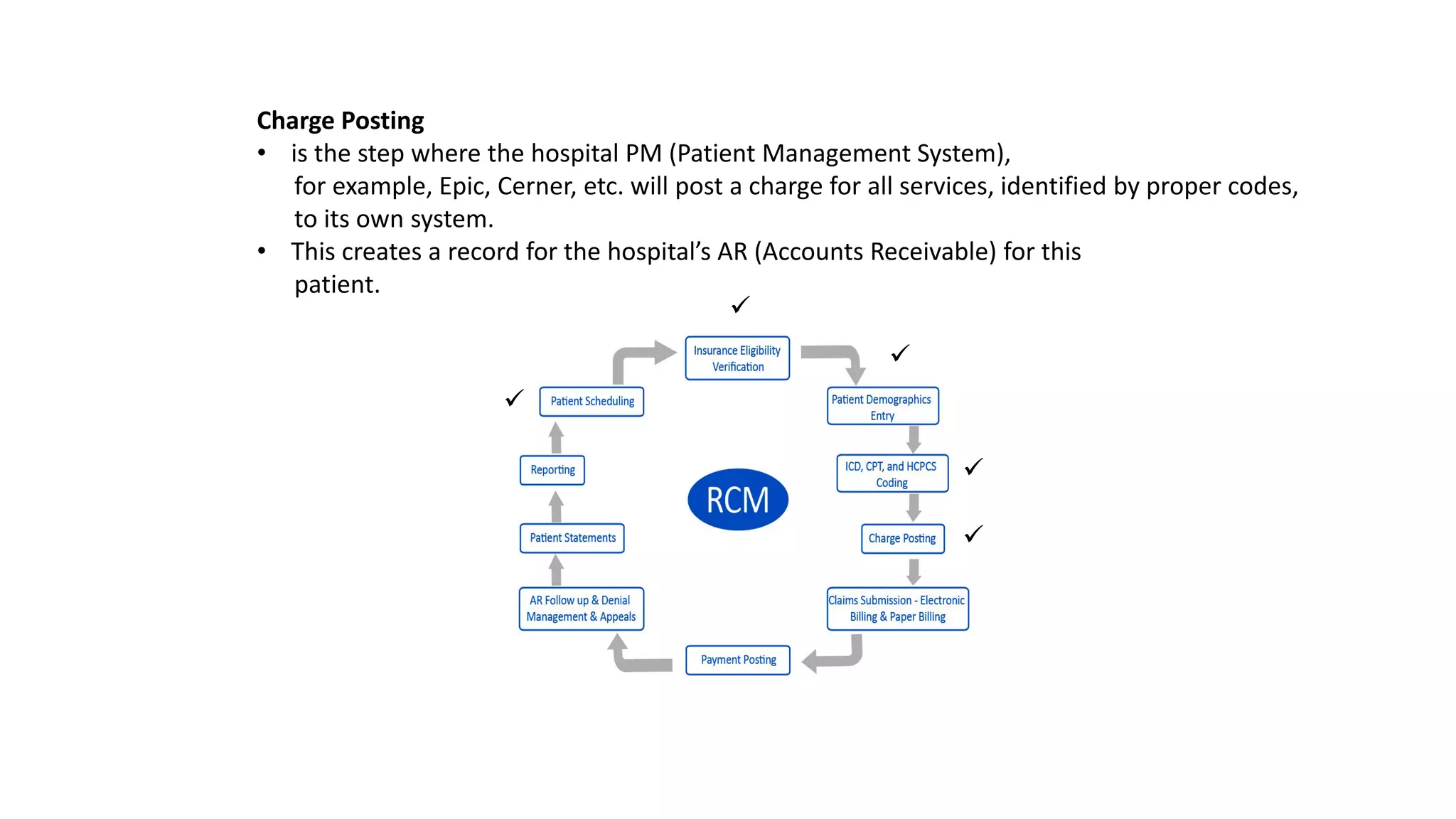
The document discusses revenue cycle management (RCM) in healthcare, emphasizing the importance of accurate patient registration, insurance verification, medical coding, charge posting, claims submission, and payment posting. It highlights the need for expertise in coding and quick follow-ups on claims to maximize payments while addressing the challenges of insurance fraud. Additionally, it notes the impact of value-based reimbursement on the revenue cycle, stressing that performance affects financial outcomes for hospitals and providers.