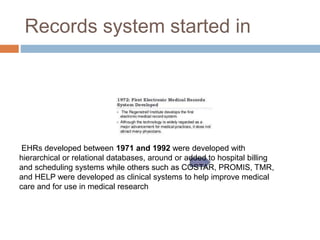
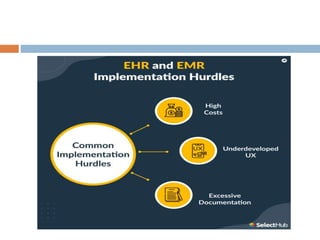
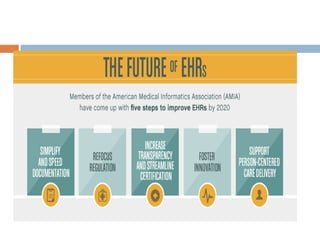
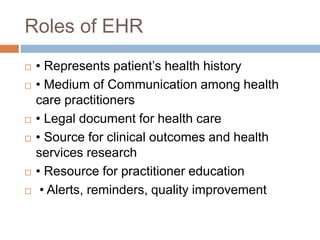
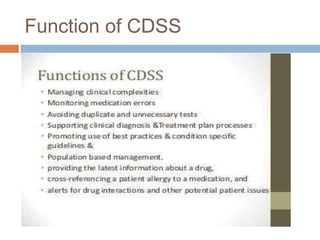
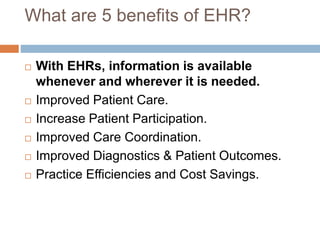
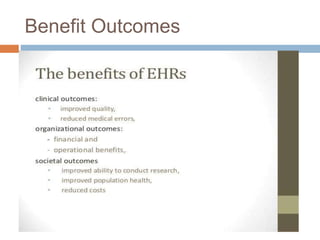
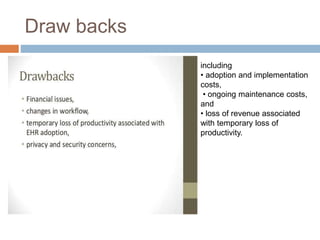
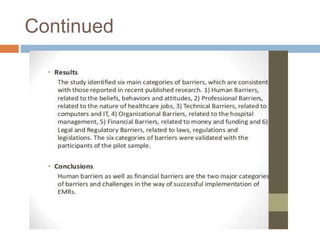
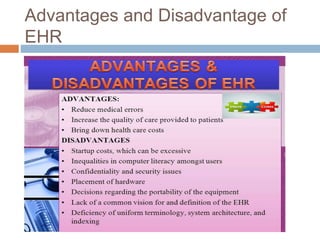
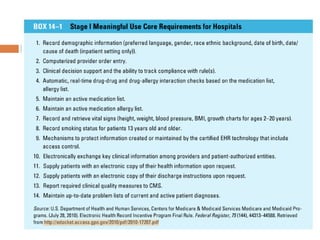
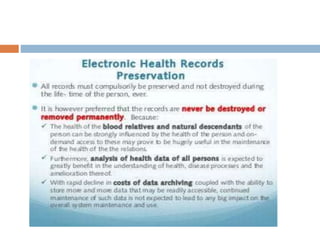
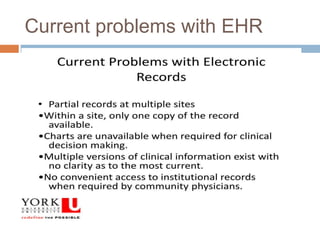
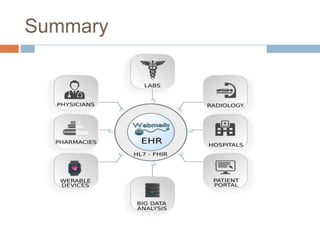
The document discusses the evolution and significance of Electronic Health Records (EHR), detailing their development from the 1960s to the present, including the introduction of the problem-oriented medical record by Larry Weed and the widespread adoption of EHRs by healthcare providers. It highlights the benefits of EHRs such as improved patient care, care coordination, and safety, while also acknowledging challenges like adoption costs and ongoing maintenance. The text concludes with an emphasis on the future of EHRs, particularly in relation to trends such as improved accessibility and integrated telehealth visits.





![References
• IOM. Crossing the quality chasm: a new health system for the
21st century. Washington, DC: Institute of Medicine; 2001.
[PubMed]
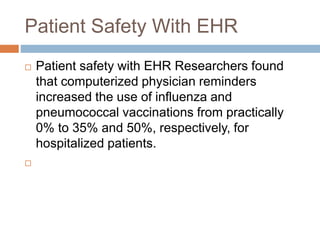
• Dexter PR, Perkins S, Overhage JM, et al. A computerized
reminder system to increase the use of preventive care for
hospitalized patients. N Engl J Med. 2001;345(13):965–970.
[PubMed]
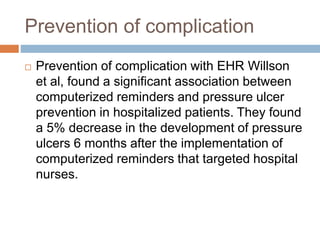
• Willson D, Ashton C, Wingate N, et al. Computerized support
of pressure ulcer prevention and treatment protocols. Proc
Annu Symp Comput Appl Med Care. 1995:646–650. [PMC
free article][PubMed]
• Rossi RA, Every NR. A computerized intervention to decrease
the use of calcium channel blockers in hypertension. J Gen
Intern Med. 1997;12(11):672–678. [PMC free article]
[PubMed]
• Tierney WM, Miller ME, McDonald CJ. The effect on test
ordering of informing physicians of the charges for outpatient
diagnostic tests. N Engl J Med. 1990;322(21):1499–1504.](https://image.slidesharecdn.com/componentsofehrppt-221207070155-5ac22d75/85/components-of-EHR-ppt-pptx-65-320.jpg)
![Continued
• Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized
physician order entry and a team intervention on prevention of
serious medication errors. JAMA. 1998;280(15):1311– 1316.
[PubMed]
• Bates DW, Teich JM, Lee J, et al. The impact of computerized
physician order entry on medication error prevention. J Am Med
Inform Assoc. 1999;6(4):313–321. [PMC free article] [PubMed]
• The National Alliance for Health Information Technology. Report to
the Office of the National Coordinator for Health Information
Technology on Defining Key Health Information Technology Terms.
[Accessed April 18,
2011].http://healthit.hhs.gov/portal/server.pt/community/healthit_
hhs_gov__reports/1239.
• Walker J, Pan E, Johnston D, et al. The value of health care
information exchange and interoperability. Health Aff (Millwood)
2005;Suppl:W5-10–15-18. [PubMed]](https://image.slidesharecdn.com/componentsofehrppt-221207070155-5ac22d75/85/components-of-EHR-ppt-pptx-66-320.jpg)