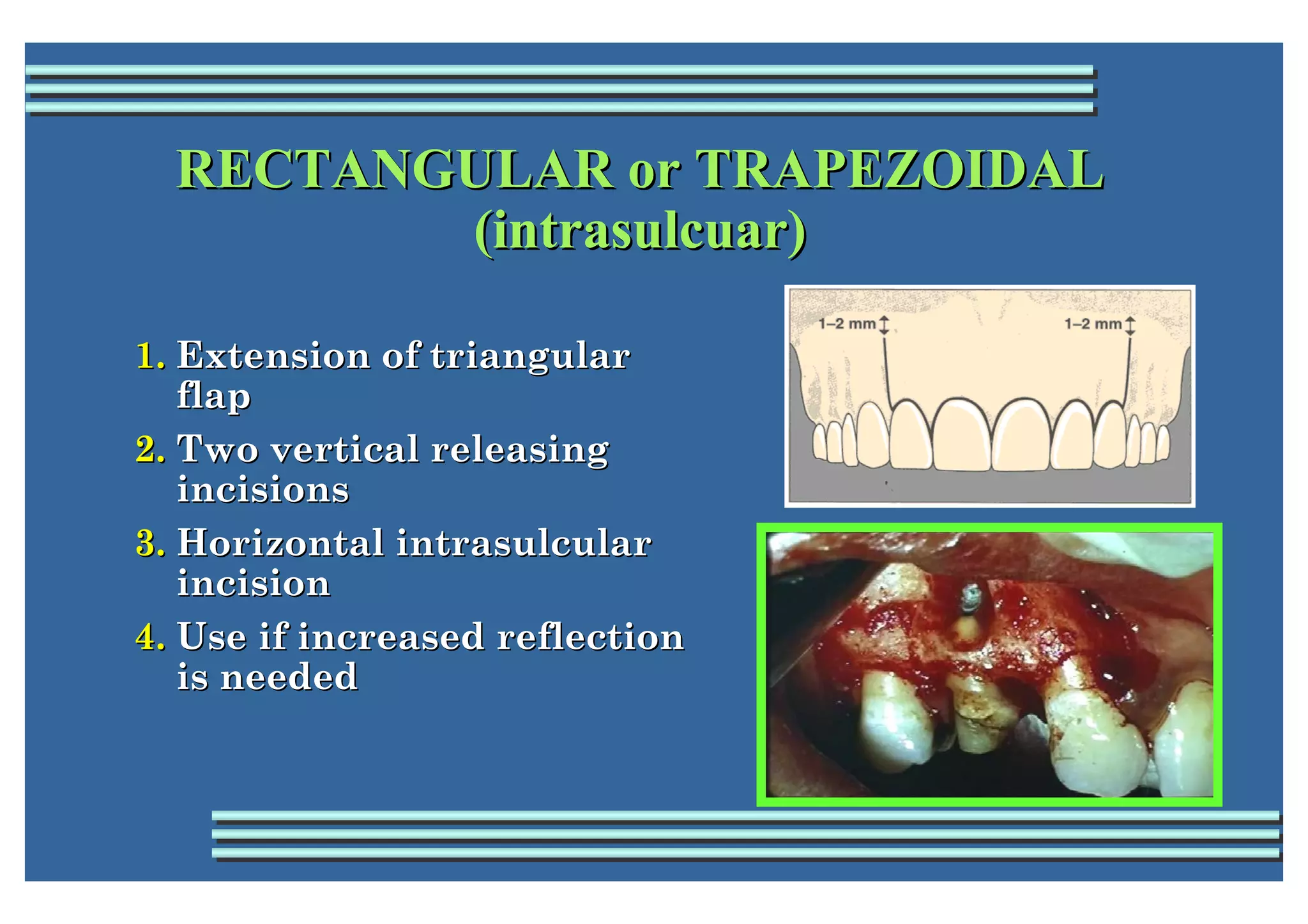
Endodontic surgery is a procedure performed to remove or correct causes of dental disease and restore tissues to health. It is often a last resort to save a tooth and requires great skill. Indications include inability to eliminate pathology with root canal treatment, inability to fully clean and fill the root canal, or iatrogenic problems like instrument breakage. Contraindications include resolved pathology, health issues, anatomic constraints, or periodontal disease. Preparation includes referral data, radiographs, diagnosis, and informed consent. Common flap designs are triangular, rectangular, or submarginal. Types of endodontic surgery include incision and drainage, trephination, periapical surgery like apicoectomy, repair of perforations,