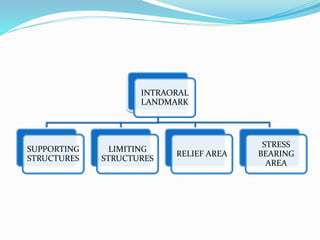
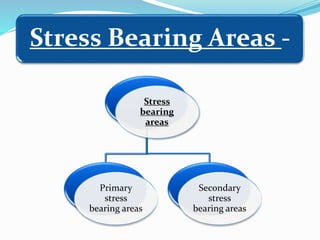
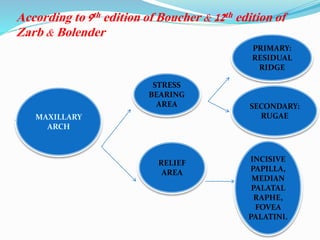
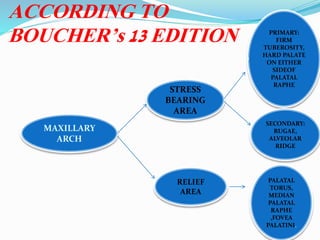
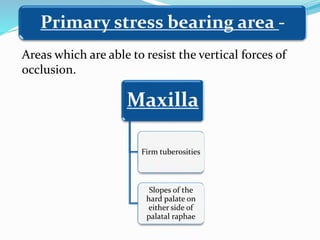
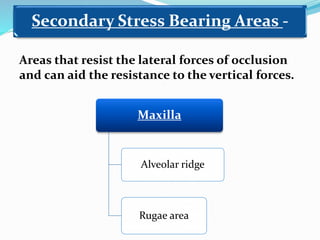
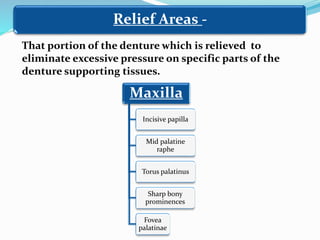
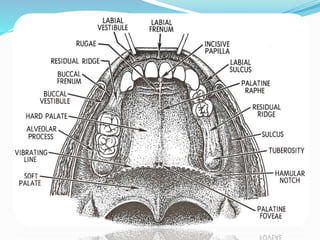
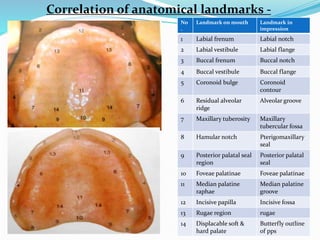
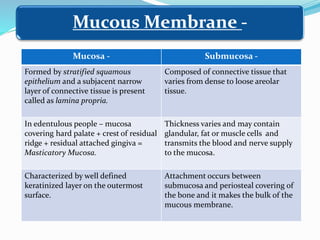
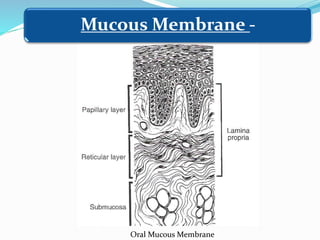
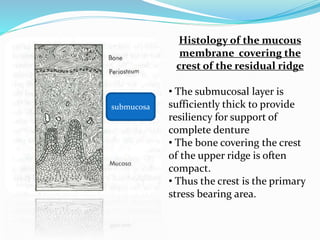
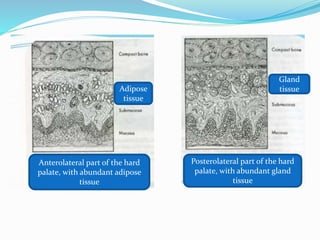
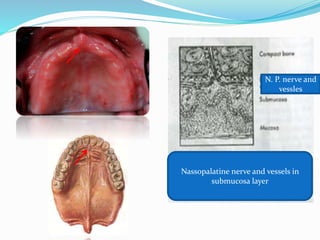
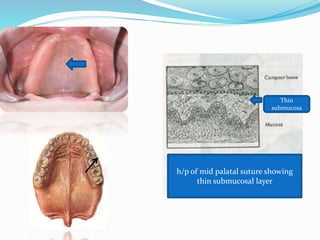
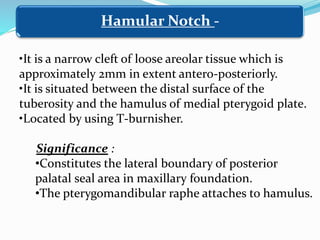
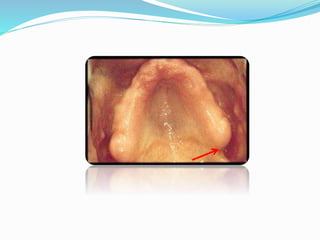
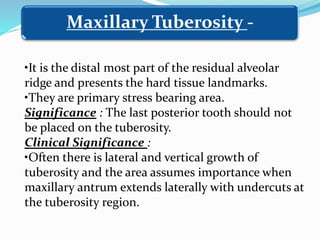
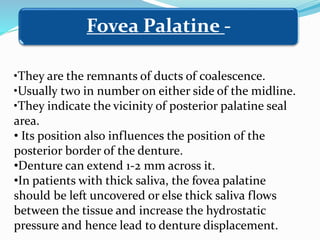
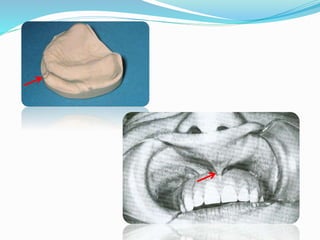
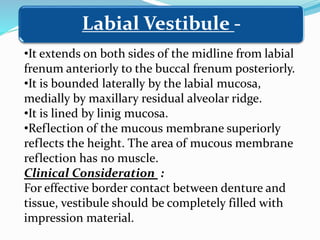
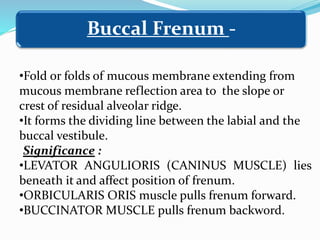
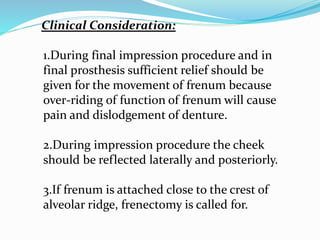
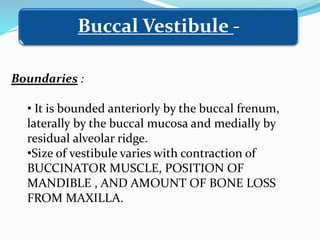
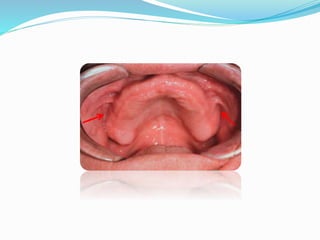
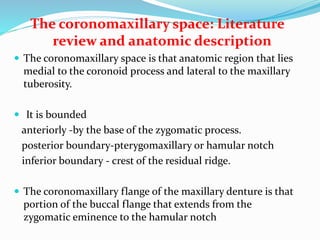
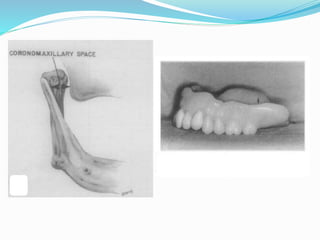
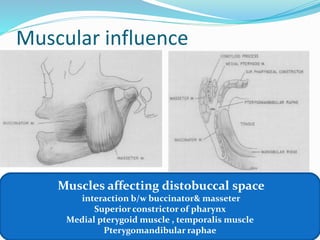
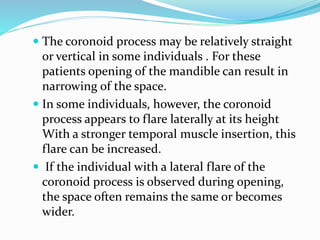
This document provides an overview of anatomical landmarks in the maxilla that are important for complete denture construction. It discusses intraoral landmarks like the labial and buccal frenums, as well as maxillary arch structures like the residual alveolar ridge, hard palate, palatal rugae, incisive papilla, hamular notch, maxillary tuberosity, and fovea palatinae that serve as stress bearing or relief areas. The document emphasizes understanding the histology and functions of these structures to ensure dentures are designed and placed to avoid placing undue pressure on supporting tissues.