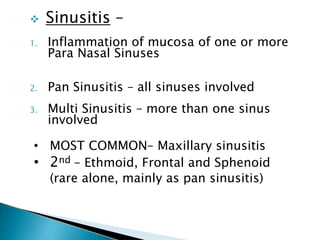
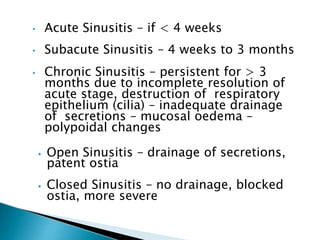
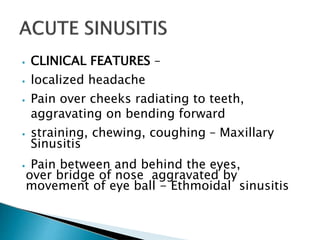
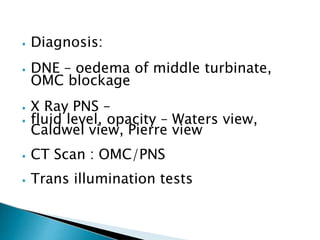
1. Sinusitis is the inflammation of the paranasal sinuses which can be acute, subacute, or chronic depending on duration of symptoms.
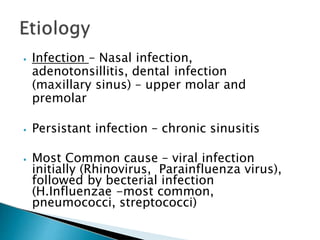
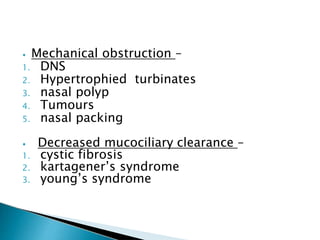
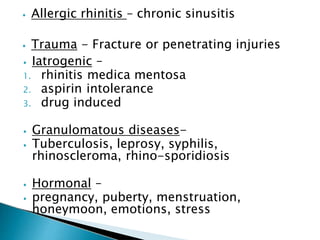
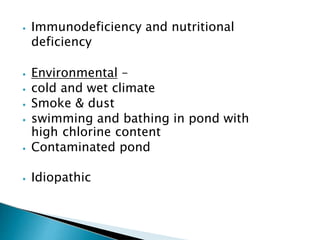
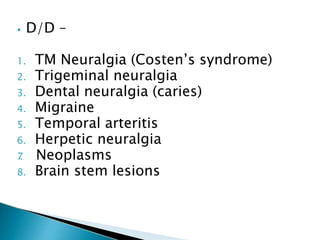
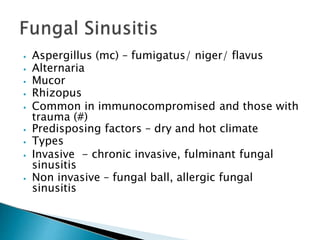
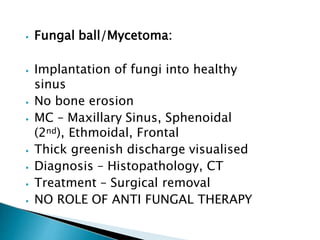
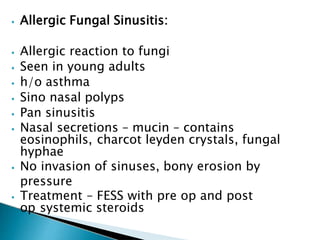
2. Common causes include viral or bacterial infections, allergies, structural abnormalities, and dental issues.
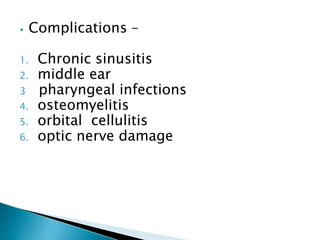
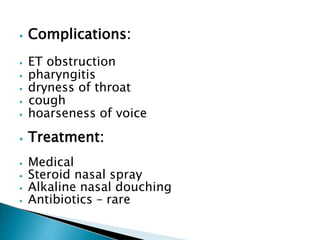
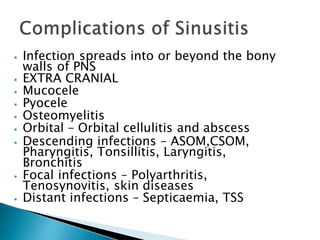
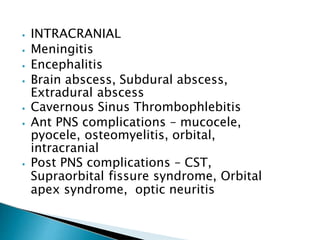
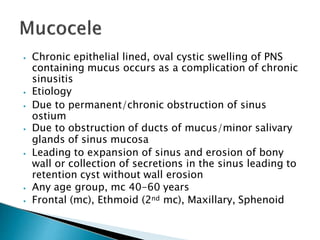
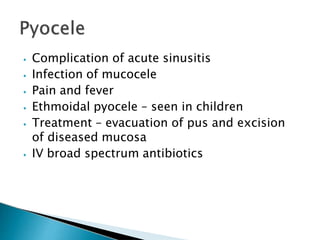
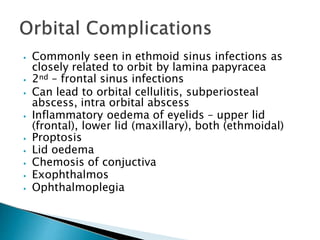
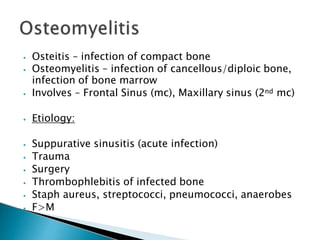
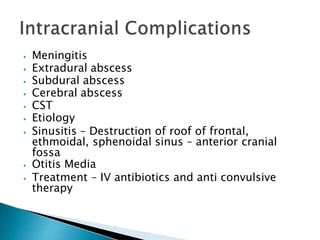
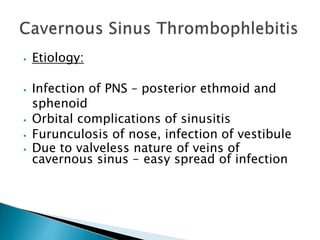
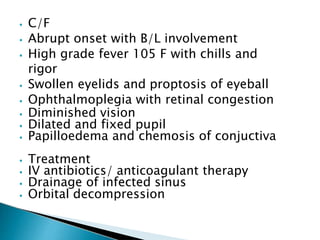
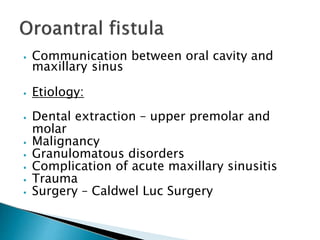
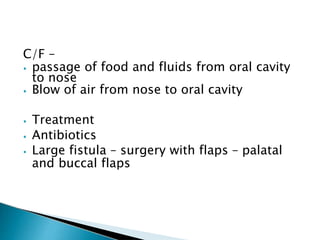
3. Potential complications include orbital cellulitis, osteomyelitis, intracranial infections like meningitis or brain abscesses if the infection spreads beyond the sinus walls.
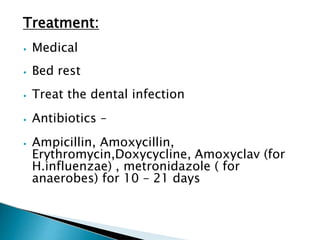
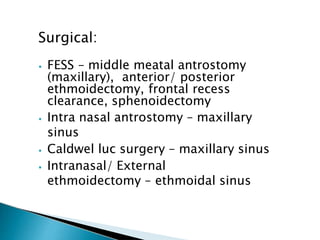
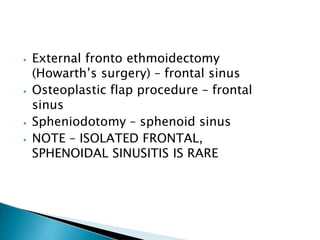
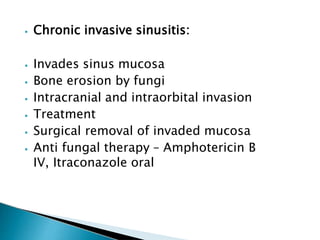
4. Treatment involves antibiotics, nasal saline irrigation, surgery to improve drainage if medical management fails.