Osteoarthritis general
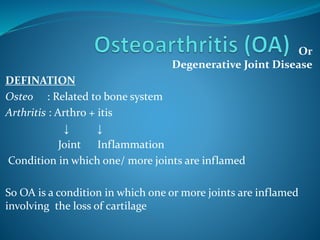
- 1. Or Degenerative Joint Disease DEFINATION Osteo : Related to bone system Arthritis : Arthro + itis ↓ ↓ Joint Inflammation Condition in which one/ more joints are inflamed So OA is a condition in which one or more joints are inflamed involving the loss of cartilage
- 2. It is progressive disorder of joints which is caused by gradual loss of cartilage resulting in development of bony spurs and crysts at the margins of the joints. In addition to damage and loss of articular cartilage, there is remodelling of subarticular bone, osteophyte formation, ligamentous laxity, weakening of periarticular muscles, and, in some cases, synovial inflammation These changes may occur as a result of an imbalance in the equilibrium between the breakdown and repair of joint tissue
- 3. The most common joints involved • Distal Interphalangeal joints • Proximal Interphalangeal joints • Carpometacarpal joints of thumb • Weight Bearing joints (Hip, knee) • Metatarsophalangeal joints of the foot • Cervicle and lumbar vartebrae
- 4. The articular cartilage is slippery tissue that covers the end of the bones in the joints Healthy cartilage allows bones to glid over each other & helps to absorb shock of movement
- 5. In OA the top layer of cartilage breaks down and wear away ↓ Rubbing of bones under the cartilage ↓ Due to which there is Pain Swelling Loss of motion of joints ↓ Over the time joint may lose its normal shape and also there is growth of bony spurs on the edge of the joint ↓ Bits of bones/cartilage can break off and float inside the joint space ↓ Which cause more pain and damage
- 7. So in OA there is progressive distruction of articular cartilage and also there is involvement of • Diarthrodial joint • Synovium • Capsule • Subchondral bone • Surrounding ligaments • Muscles Changes in structure and function of this tissues leads to clinical Osteoarthritis Which is characterized by • Joint pain • Tenderness • Decrease range of motion • Weakness • Joint instability • Disability
- 8. Classification ↙ ↘ Primary OA Secondary OA (idiopathic) (Due to some other disease) A. Localised Hands Hip Knee Spine B. Generalised Small joints Large joints Mixed C. Erosive osteoarthritis i) Congenital and developmental disorders, bone dysplasias ii) Post-surgery / injury – meniscectomy iii) Endocrine –acromegaly, iv) Metabolic –hemachromatosis, ochronosis, Marfan syndrome, Ehler-Danlos syndrome, Paget disease, gout, pseudogout, Wilson’s disease, Hurler disease, Gaucher disease v) Rheumatologic– rheumatoid arthritis vi) Neurological– Charcot joints.
- 9. Epidemiology OA is one of the core reason for disability Nearly everyone who lives long is affected by OA at any point of life, most probably after the age of 55 to 60. Approximately 15% of population is affected by OA ↙ ↘ ↙ ↘ 50 % of those 85% of those over 65 age over 75 age OA is most widely assessed in studies using the Kellgren and Lawrence (K&L) score. The overall grades of severity are determined from 0 to 4 and are related to the presumed sequential appearance of osteophytes, joint space loss, sclerosis and cysts
- 10. The World Health Organization (WHO) adopted these criteria as the standard for epidemiological studies on OA Prevalence of osteoarthritis varies with I. Age II. Gender III. Genetics IV. Ethic Group V. Specific Joint Involved VI. Method For Diagnosis
- 11. AGE With increasing age the prevalence OA also increases Generally for person age 25 – 75,prevalence is estimated 12% and for those with age over 70, it is 60 – 70% affectet Hip OA ← ← AGE → → Hand OA ↙ ↘ ↓ ↙ ↘ Age : 30 – 40 Age : >70 Knee OA Age : 40 Age : 80 Pre : 1.6 % Pre : 14% ↙ ↘ Pre: 5% Pre : 65% Age : >25 Age : 55 Pre : 5% Pre : 12%
- 12. Gender ↙ ↘ Age > 50 Age >60 Men are more affacted Women are more affacted(26%) Due to higher rate of sports and Due to repeated use of Injuries weight bearing joints Genetics ↙ ↘ Pre : 9% Pre : 4% White population Black & Asian population Prevalence of OA is 22% to 39% in India
- 14. Etiology The etiology of OA is multifactorial Many patients have more than one risk factor for developing the OA. The most common risk factor for the development of OA includes • Obesity • Occupation • Participation in certain sports (Often) • History of joint trauma • Genetic • Age • Sex • Bone density • Joint location
- 15. Obesity Increased body weight is strongly associated with hip, knee, and hand OA Obesity often precedes OA and contributes to its development, rather than occurring as a result of inactivity from joint pain In a three-decade Framingham Study, the highest quintile of body mass was associated with a higher relative risk of knee OA (relative risk of 1.5 to 1.9 for men and 2.1 to 3.2 for women). The risk of developing OA increases by about 10% with each additional kilogram of weight, and in obese persons without OA, weight loss of even 5 kg decreases the risk of future knee OA by one-half.
- 16. Recent data suggest that OA is associated with the metabolic syndrome, suggesting a possible common pathogenic mechanism involving metabolic abnormalities and systemic Inflammation. It is also likely that vascular disease may both initiate and hasten disease progression in OA. This could be due to venous occlusion, stasis or microembolic disease leading to episodic reduction in blood flow through small vessels within the subchondral bone. Subchondral ischaemia may subsequently reduce nutrient delivery and gas exchange to articular cartilage in addition to direct deleterious effects on the bone itself.
- 17. Occupation There is increased risk of OA for those who are in occupation requiring Prolong Standing Kneeling Squatting Lifting/Moving Heavy Objects ↓ →Miming Factory Work Car paintery Repetitive motion also contributes to hand OA with dominant hand usually affected Risk OA depends on type and intensity of physical activity
- 18. Sports Damage to articular cartilage due to sports greatly increase the risk of OA Meniscal damage (common in athlete) also increase the risk of knee OA 1.Because of loss of proper load bearing and shock absorption 2.Increase focal load on cartilage and subchondral bones Trauma AGE AT INJURY DOSE MATTER As older individuals who damage ligaments tends to develope OA more rapidly than young people with similar injury Trauma early in life →Increased risk of OA
- 19. Genetic Factors A number of recent studies discovered the presence of over 80 gene mutations involved in the pathogenesis of OA ,among which the most relevant one is a single nucleotide polymorphism. This one, called rs143383 and located in the 3' untranslated region (3'UTR) of the growth and differentiation factor 5 gene (GDF5), is responsible for the development, maintenance and repair of synovial joints Genes for Vitamin D receptors (VDR) and insulin-like growth factor 1(IGF-1) also seem to be involved in the patho-physiologic pathways of OA It also includes genes related to inflaamation,bone morphogenetic protiens, protease/ its inhibitors
- 21. Normal Articular Cartilage Articular Cartilage Possesses ↓ Viscoelastic Properties ↓Which provides 1. Lubrication With Motion 2. Shock absorbency during rapid movement 3. Load Support In Synovial joints Articular cartilage is found between synovial cavity on one side and narrow layer of calcified tissue overlying subchondral bone on onther side
- 22. Charactristics of Articular Cartilage 1.Cartilage is easily compressed lossing up to 40% of its original hight when load is applied ↓ Compression increase area of contact ↓ Disperse force more evenly to undelying bone,tendon, ligament, muscles 2.Cartilage is frictionless Togather with compresibility , this enables smooth movement in joint and distributes load across joint tissue to prevent damage and stabilize the joint
- 23. Structure of Cartilage Cartilage is having ↓ 1.Strength 2.Low co-efficiant of friction 3.Copressiblity These all is derived from its unique structure So,the cartilage is composed of complex, hydrophilic , Extra- cellular matrix It contains →75% to 85% Water 2% to 5% Chondrocytes (the only cell in cartilage) Collagen Protiens Proteoglycans Hyaluronic Acid Molecules
- 24. Two Major Structure of Cartilage Type II Collagen Tightly woven, triple helical structure which provides TENSILE STRENGTH to cartilage Aggrecans In which there is Proteoglycan linked with hyluronic acid, having negative charge. The strong electrostatic repulsion of proteoglycan gives cartilage the ability to withstand further compression
- 25. Normal Cartilage turn over ↓ Helps repair and restore cartilage ↓ Respond to usual demand of loading and physical activity In healthy adult cartilage chondrocyte metabolism is slow with dynamic balance between anabolic process Metabolism is premoted by 1. Groth factors - Bone morphogenetic protien 2 - Insulin like groth factor-1 - tranforming growth factor 2. Catabolism 3. Proteolysis Stimulated by MMPs, TNF-ᾲ, Interlukein-1, Other cytokines
- 26. Joint Protective Mechanisms 1.Muscle Bridging The Joints 2.Sensory receprtors in feedback loops to regulate muscle and tondon function 3. Supporting ligaments 4. Subchondral bones having shock absorbent properties Note Articular cartilge is avascular and aneural and chondrocytes are nourised by synovial fluid
- 29. OA Cartilage OA begins with damage to articular cartilage, which is due to 1. Trauma or other injury 2. Excess joint loading by obesity / other reason 3. Instability or injury of the joint that causes abnormal loading Devlopement of OA is due to 1. Local mechanical influence 2. Genetic factor 3. Inflammation 4. Chondrocyte function Which leads to loss of articular cartilage
- 30. When there is damage to articular cartilage ↓ Increase activity of chondrocytes to remove and repair the damage Depending on degree of damage the balance between breakdown and resynthesis of cartilage can be lost ↓ Which leads to increase breakdown of cartilage ↓ Ultimately, loss of cartilage Destruction of aggrecans by proteolytic enzyme is consider to play a key role
- 31. There is also involvement of collagen receptors named DDR-2 , located on chodrocyte cell surface In healthy cartilage ,DDR-2 is inactive ,which is masked by aggrecan from contact with collegen Damage to cartilage ↓ Triggers aggrecan destruction ↓ Exposure of DDR-2 to collagen ↓ Active DDR-2 increase activity of MMP-13 ↓ Which destroy collagen Collagen breakdown products further stimulate DDR-2,in which more collagen is destroyed
- 32. Huge research work has been done on genes involved in OA which shows that In OA , expression of hundreds of genes of cartilage tissue are affected which alters chondrocyte phenotype In addition to articular cartilage there is also role of subchondral bone in OA In OA , subchondral bone release vasoactive peptides and MMPs Neovascularization and subsequent increase in permeability of the adjacent cartilage occurs and contributes to further cartilage loss
- 33. Substantial loss of cartilage cause joint space narrowing and leads to painful and deformed joints The remaining catilage softens and devlopes fibrillation(Verticle cleft ) and there is splittting and further loss of cartilage and exposure of underlying bone As cartilage is destroyed and the adgecent subchondral bone undergoes pathologic changes, cartilage is eroded completely, leaving denuded subchondral bone which becomes dence , smooth and glistening A more brittle, stiffer bone results, with decreased weight-bearing ability and development of sclerosis and microfractures The joint capsule and synovium also show pathologic changes in OA.
- 34. Inflammation, noted clinically as synovitis, may result from release of inflammatory mediators from chondrocytes, such as prostaglandins Inflammation is localized to the affected joint, in contrast to that seen in rheumatoid or other inflammatory arthritides. The pain in OA is not due to distruction of cartilage but arise from the activation of nociceptive nerve ending within the joint by mechanical and chemical irritants
- 35. So,the slow progressive changes in OA consist of an increase in water content, loss of PG, and reduction of PG aggregates of cartilage. The cartilage is subsequently unable to repair itself. Alterations in metabolism of subchondral bone adjacent to articular cartilage appear necessary for continued cartilage destruction. Eventually, progressive loss of articular cartilage and increasing subchondral sclerosis lead to an abnormal and painful joint.
- 37. Age Usually elderly Gender Age <45 more common in men Age >45 more common in women Symptoms →Pain Deep, aching character Pain on motion Pain with motion early in disease Pain with rest late in disease → Stiffness in affected joints Resolves with motion, recurs with rest Usually <30 minutes’ duration Often related to weather → Limited joint motion May result in limitations activities of daily living Signs, history, and physical examination Monarticular or oligoarticular; asymmetrical involvement Hands Distal interphalangeal joints Heberden’s nodes Proximal interphalangeal joints Bouchard’s nodes First carpometacarpal joint Osteophytes give characteristic square appearance of the hand Knees Patellofemoral compartment involvement Pain related to climbing stairs Transient joint effusions Typically noninflammatory synovial fluid Clinical Represntation
- 38. Hips Pain during weight-bearing activities Stiffness, especially after inactivity Limited joint motion Spine L3 and L4 involvement is most common in the lumbar spine Signs and symptoms of nerve root compression Radicular pain Paresthesias Loss of reflexes Muscle weakness associated with the affected nerve root Feet Typically involves the first metatarsophalangeal joint Other sites, less commonly involved Shoulder, elbow, acromioclavicular, sternoclavicular, and temporomandibular joints Observation on joint examination Bony proliferation or occasional synovitis Local tenderness Muscle atrophy Limited motion with passive/active movement Deformity Radiologic evaluation Early mild OA Radiographic changes often absent Progression of OA Joint space narrowing Subchondral bone sclerosis Marginal osteophytes Late OA Abnormal alignment of joints Effusions Characteristics of synovial fluid High viscosity Mild leukocytosis Laboratory values ESR
- 39. Treatment Goals (1) to educate the patient, caregivers, and relatives; (2) to relieve pain and stiffness; (3) to maintain or improve joint mobility; (4) to limit functional impairment; and (5) to maintain or improve quality of life Treatment of OA Non-pharmacological Treatment 1.Diet 2.Physical And Occupational Therapy 3.Surgery Pharmacological Treatment 1.Analgesics Oral Topical 2.NSAIDs 3. Glucosamine &Chondroitin 4.Hyluronate Injection 5.Narcotic Analgesics 6.Disease Modifying Drugs
- 40. Diet Excess weight increases the biomechanical load on weight- bearing joints, and is the single best predictor of need for eventual joint replacement. Weight loss is associated with decreased symptoms and Disability Even 3-5 kg of weight loss can decrease the biomechanical force on a weight-bearing joint. Although dietary intervention for overweight OA patients is reasonable, weight loss usually requires a motivated patient and a structured weight-loss program. Diet with low fat (calories) and high fibre as well as balanced diet should be taken to decrease weight
- 41. Physical And Occupational Therapy Physical therapy—with heat or cold treatments and an exercise program Which helps to maintain and restore joint range of motion and reduce pain and muscle spasms. Warm baths or warm water soaks may decrease pain and stiffness. Exercise programs and quadriceps strengthening can improve physical functioning and can decrease disability, pain, and analgesic use by OA patients. The decision about whether to encourage walking should be made on an individual basis. With weak or deconditioned muscles,the load is transmitted excessively to the joints, so weight-bearing activities can exacerbate symptoms.
- 42. However, avoidance of activity by those with hip or knee OA leads to further deconditioning or weight gain. A program of patient education, muscle stretching and strengthening,and supervised walking can improve physical function and decrease pain in patients with knee OA.
- 43. Surgery Surgery can be recommended for OA patients with functional disability and/or severe pain that is unresponsive to conservative Patients with mild knee OA, an osteotomy may correct the misalignment of knee Knee arthroscopy or lavage have been recommended for short- term relief of pain, a recent study showed these two procedures to be equivalent to surgery Experimental but potentially restorative approaches involve Soft tissue grafts, Penetration of subchondral bone, Cell transplantation, and Use of growth factors
- 44. Pharmacological Therapy Things to be taken in concern 1.Adverse effect of the drug given for OA 2.As OA is usually seen in old age people with some other conditions they Pharmacological treatment should be done with so much causion 3.Always combine non pharmacological therapy with pharmacological one for more improvement
- 45. Analgesics Acetaminophen is used as first-line drug therapy for pain management in OA, due to its relative safety, efficacy, and lower cost compared to NSAIDs Pain relief with acetaminophen can be similar to that obtained with NSAIDs, although some patients will respond better to NSAIDs. Some studies have shown comparable efficacy for acetaminophen and NSAIDS, others have reported that patients experienced better pain control with NSAIDs than with acetaminophen, and that OA patients preferred NSAIDs to acetaminophen
- 46. Mechanism Of Action Acetaminophen is thought to work within the central nervous system to inhibit the synthesis of prostaglandins, agents that enhance pain sensations. Acetaminophen prevents prostaglandin synthesis by blocking the action of central cyclooxygenase. Kinetics Acetaminophen is well absorbed after oral administration (bioavailability is 60% to 98%), achieves peak concentrations within 1 to 2 hours, is inactivated in the liver by conjugation with sulfate or glucuronide, and its metabolites are renally excreted Efficacy Comparable relief of mild to moderate OA pain has been demonstrated for acetaminophen at 2.6 to 4 g/day
- 47. ADR Hepatotoxicity, and Possibly renal toxicity Drug – Drug Intrection Isoniazid can increase the risk of hepatotoxicity. Chronic ingestion of maximal doses of acetaminophen may intensify the anticoagulant effect in patients taking warfarin, Food decreases the maximum serum concentration of acetaminophen by approximately one-half.
- 48. Non Steroidal Anti - Iflammatory Drugs MOA Blockade of prostaglandin synthesis through inhibition of cyclooxygenase (bothCOX-1 andCOX-2 enzymes) is the principal mechanism by which NSAIDs relieve pain and inflammation
- 49. Kinetics High oral availability, high protein binding, and absorption as active drugs (except for sulindac and nabumetone, which require hepatic conversion for activity). The most important difference in NSAIDs is a serum half-life ranging from 1 hour for tolmetin to 50 hours for piroxicam, impacting the frequency of dosing and potentially, compliance with therapy. Elimination of NSAIDs largely depends on hepatic inactivation, with a small fraction of active drug being renally excreted. NSAIDs penetrate joint fluid, reaching about 60% of blood levels
- 50. ADR Minor complaints—nausea, dyspepsia, anorexia, abdominal pain, flatulence, and diarrhea To minimize these symptoms, NSAIDs should be taken with food or milk, except for enteric-coated products, which should not be taken with milk or antacids All NSAIDs have the potential to cause GI bleeding. Possible Mechanism For this Unionized NSAIDs enter gastric mucosal cells, release hydrogen ions, and are concentrated (“ion trapped”) within cells, with cell death or damage. Gastric mucosal injury can also result from NSAID inhibition of gastroprotective prostaglandins.
- 51. COX-2 inhibitors pose a decreased risk of GI toxicity compared to nonspecific NSAIDs, an especially important consideration when treating those at risk for clinically significant GI adverse effects. NSAIDs may cause kidney diseases, Acute renal insufficiency, Hyperkalemia, and Renal papillary necrosis Clinical features of these NSAID-induced renal syndromes Increased serum creatinine Increased blood urea nitrogen, Hyperkalemia, Elevated blood pressure, Peripheral edema, and Weight gain.
- 52. Mechanisms of NSAID injury include direct toxicity, and inhibition of local prostaglandins that promote vasodilation of renal blood vessels and preserve renal blood flow. COX-2 inhibitors also have potential for renal toxicity; COX-2 activity has been demonstrated in a variety of sites in the kidney and is upregulated in salt-depleted states Importantly,COX-2 inhibitors decrease urinary prostaglandins and cause sodium and potassium retention, as do nonspecific NSAIDs
- 54. Drug Intrection Lithium, Warfarin, Oral hypoglycemics, High-dose methotrexate, Antihypertensives, Angiotensin-converting enzyme inhibitors, β-blockers, and diuretics.
- 55. Topical Therapies Topical products can be used alone or in combination with oral analgesics or NSAIDs. Capsaicin, isolated from hot peppers, releases and ultimately depletes substance P from afferent nociceptive nerve fibers. Substance P has been implicated in the transmission of pain in arthritis, and capsaicin cream has been shown in four controlled studies to provide pain relief in OA when applied over affected joints To be effective, capsaicin must be used regularly, and it may take up to 2 weeks to work. It is well tolerated, except that some patients experience a temporary burning sensation at the site of application. Although use is recommended four times a day, a twice-daily application may enhancelong-term adherence and edequate effet
- 56. GLUCOSAMINE AND CHONDROITIN These substances stimulate proteoglycan synthesis from articular cartilage in vitro Chondroitin and glucosamine are superior to placebo in alleviating pain from knee or hip OA. In studies, chondroitin sulfate showed similar analgesic benefits to diclofenac A recent meta-analysis of glucosamine and chondroitin indicated that both agents had efficacy in reducing pain and improving mobility, and that glucosamine reduced joint space narrowing further more were associated with slower loss of cartilage than placebo, in knees affected by OA
- 57. CORTICOSTEROIDS Intra-articular glucocorticoid injections can provide excellent pain relief, particularly when a joint effusion is present Aspiration of the effusion and injection of glucocorticoid are carried out aseptically,and examination of the aspirate to exclude crystalline arthritis or infection is recommended. The therapy is generally limited to three or four injections per year because of the potential systemic effects of steroids, and because the need for more frequent injections indicates little response to the therapy. Systemic corticosteroid therapy is not recommended in OA, given the lack of proven benefit and the well-known adverse effects with long-term use.
- 58. HYALURONATE INJECTIONS Agents containing hyaluronic acid (HA) (sodium hyaluronate) are available for intra-articular injection for treatment of knee OA. High-molecular-weight HA is an important constituent of normal cartilage, with viscoelastic properties providing lubrication with motion and shock absorbency during rapid movements Endogenous HA also may have anti-inflammatory effects because the concentration and molecular size of synovial HA decrease in OA, administration of exogenous HA products has been studied, with the theory that this could reconstitute synovial fluid and reduce symptoms. Injections temporarily and modestly increase viscosity. HA products are injected once weekly for either 3 or 5 weeks.
- 59. Injections are well tolerated, although acute joint swelling and local skin reactions, including rash, ecchymoses, and pruritus have been reported. HA injections may be beneficial for patients unresponsive to other therapies. These agents are expensive because the treatment includes both drug costs and administration costs. As a result, HA injections are often used after less expensive therapies have demonstrated lack of efficacy
- 60. DISEASE-MODIFYING DRUGS Disease-modifying drugs are targeted not at pain relief but at preventing, retarding, or reversing damage to articular cartilage Most products have been tested in animal models, and limited human data are available. Thus far, OA is a disease whose symptoms can be alleviated, but whose progress is impossible to stop because of this, clinicians were very interested to learn that both chondroitin and glucosamine show disease-modifying potential in patients with OA Another approach is that of pharmacologic agents that could mimic TIMPs and thus potentially decrease cartilage destruction.
- 61. Heparinoid products that contain glycosaminoglycans, sodium pentosan polysulfate, and calcium pentosan polysulfate show promise in preliminary work limited largely to animal models and in vitro studies There is also recent interest in the potential of cyclooxygenase- inhibiting nitric oxide–donor compounds to relieve OA while sparing GI adverse effects.
- 62. NARCOTIC ANALGESICS Low-dose narcotic analgesics may be very useful in patients who experience no relief with acetaminophen, NSAIDs, intra-articular injections, or topical therapy. These agents are particularly useful in patients who cannot take NSAIDs due to renal failure, or for patients in whom all other treatment options have failed and who are at high surgical risk, precluding joint arthroplasty. Low-dose narcotics are the initial intervention, usually given in combination with acetaminophen. Sustained-release compounds usually offer better pain control throughout the day, and are used when simple narcotics are ineffective.
- 63. If pain is intolerable and limits activities of daily living, and the patient has sufficiently good cardiopulmonary health to undergo a major surgery, joint replacement may be preferable to continued reliance on narcotics.
- 64. Guided By Samir Rabadiya, Associate Profesor ,Department Of Pharmaceutical Sciences Acknowledgement Sachin Parmar,Associate Profesor ,Department Of Pharmaceutical Sciences Payal Bhalodia,Associate Profesor ,Department Of Pharmaceutical Sciences Rahul Solanki,BE
- 65. References Pharmacotherapy ,A Pathophysiological Approch Joseph T. DiPiro, PharmD, FCCP Professor and Executive Dean, South Carolina College of Pharmacy, University of South Carolina, Columbia, and Medical University of South Carolina, Charleston Robert L. Talbert, PharmD, FCCP, BCPS Professor, College of Pharmacy, University of Texas at Austin; Professor, Departments of Medicine and Pharmacology, University of Texas Health Science Center at San Antonio, Texas Gary C. Yee, PharmD, FCCP Professor and Chair, Department of Pharmacy Practice, College of Pharmacy, University of Nebraska Medical Center, Omaha, Nebraska Gary R. Matzke, PharmD, FCP, FCCP Professor, Department of Pharmacy and Therapeutics, School of Pharmacy, Renal-Electrolyte Division, School of Medicine, University of Pittsburgh, Pittsburgh, Pennsylvania Barbara G. Wells, PharmD, FASHP, FCCP, BCPP Dean and Professor, School of Pharmacy, The University of Mississippi, University, Mississippi L. Michael Posey, BS Pharm President, PENS Pharmacy Editorial and News Services, Athens, Georgia
- 66. Arthritis Research UK Obesity Action Coalition Anna Litwic, MD [Specialist Registrar in Rheumatology] Giuseppe Musumeci , Department of Biomedical and Biotechnological Sciences, Human Anatomy and Histology Section, School of Medicine, University of Catania, Via S. Sofia 87, 95123 Catania, Italy; F. Berenbaum yz Department of Rheumatology, AP-HP Saint-Antoine Hospital, 75012 Paris, France V Tandon
Editor's Notes
- , aspirin 650 mg four times daily, ibuprofen at 1200 or 2400 mg daily, and naproxen 750 mg/day
- Efficacy Choosing of cox inhibitior Valdecoxib new drug Cvs toxisity
