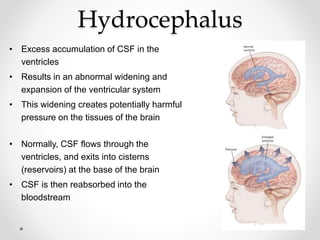
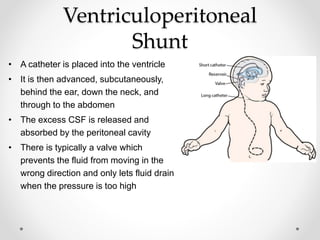
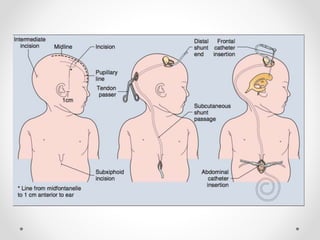
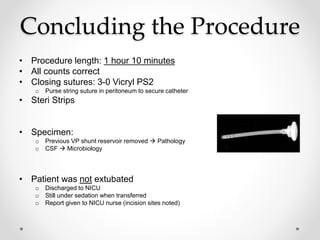
A baby girl born at 38 weeks was diagnosed with hydrocephalus after birth. She underwent a ventriculoperitoneal shunt placement surgery at 8 days old to drain excess cerebrospinal fluid from her brain ventricles into her abdomen. The surgery involved placing a catheter from her brain ventricle into her abdomen, with a valve to regulate fluid flow. Precautions were taken due to her young age, including maintaining her body temperature. She was placed under general anesthesia and monitored closely after the surgery for potential complications like infection.