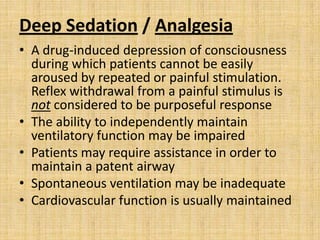
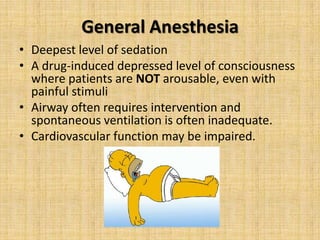
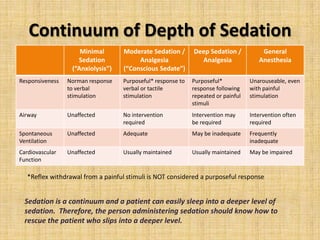
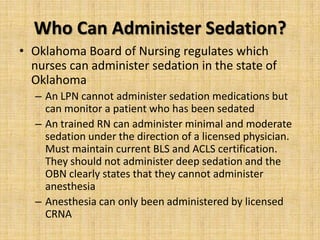
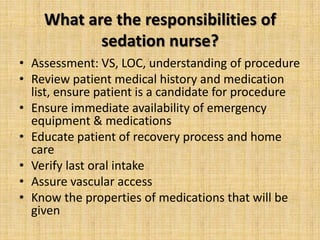
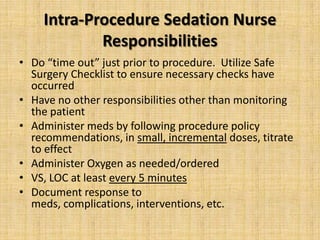
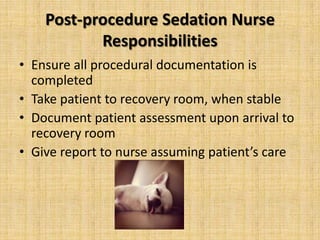
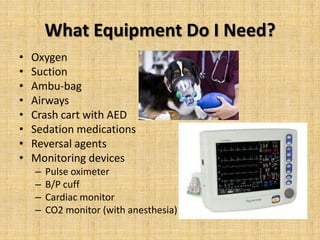
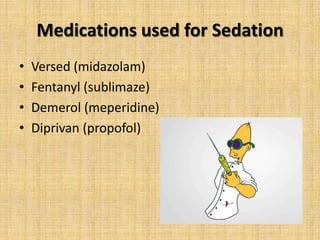
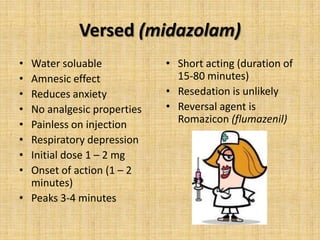
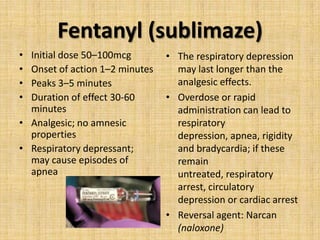
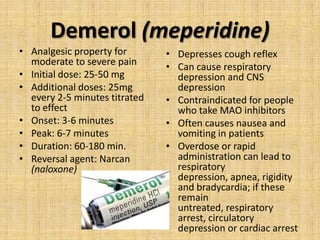
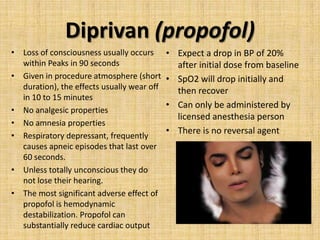
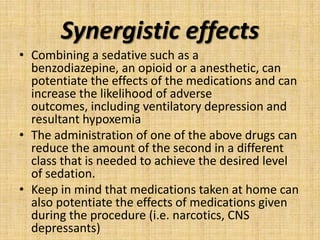
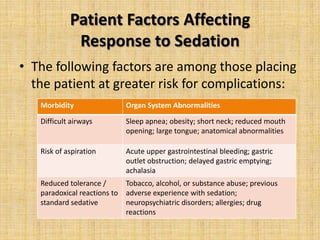
This document provides information about procedural sedation, including the different levels of sedation from minimal to general anesthesia. It discusses who is allowed to administer various levels of sedation according to Oklahoma regulations. The responsibilities of sedation nurses during the pre-procedure, intra-procedure, and post-procedure periods are outlined. Common sedation medications like Versed, Fentanyl, Demerol and Diprivan are described along with their properties, dosages and side effects. The synergistic effects of combining sedation medications are noted as increasing risks. Finally, patient factors that could increase sedation risks are listed.