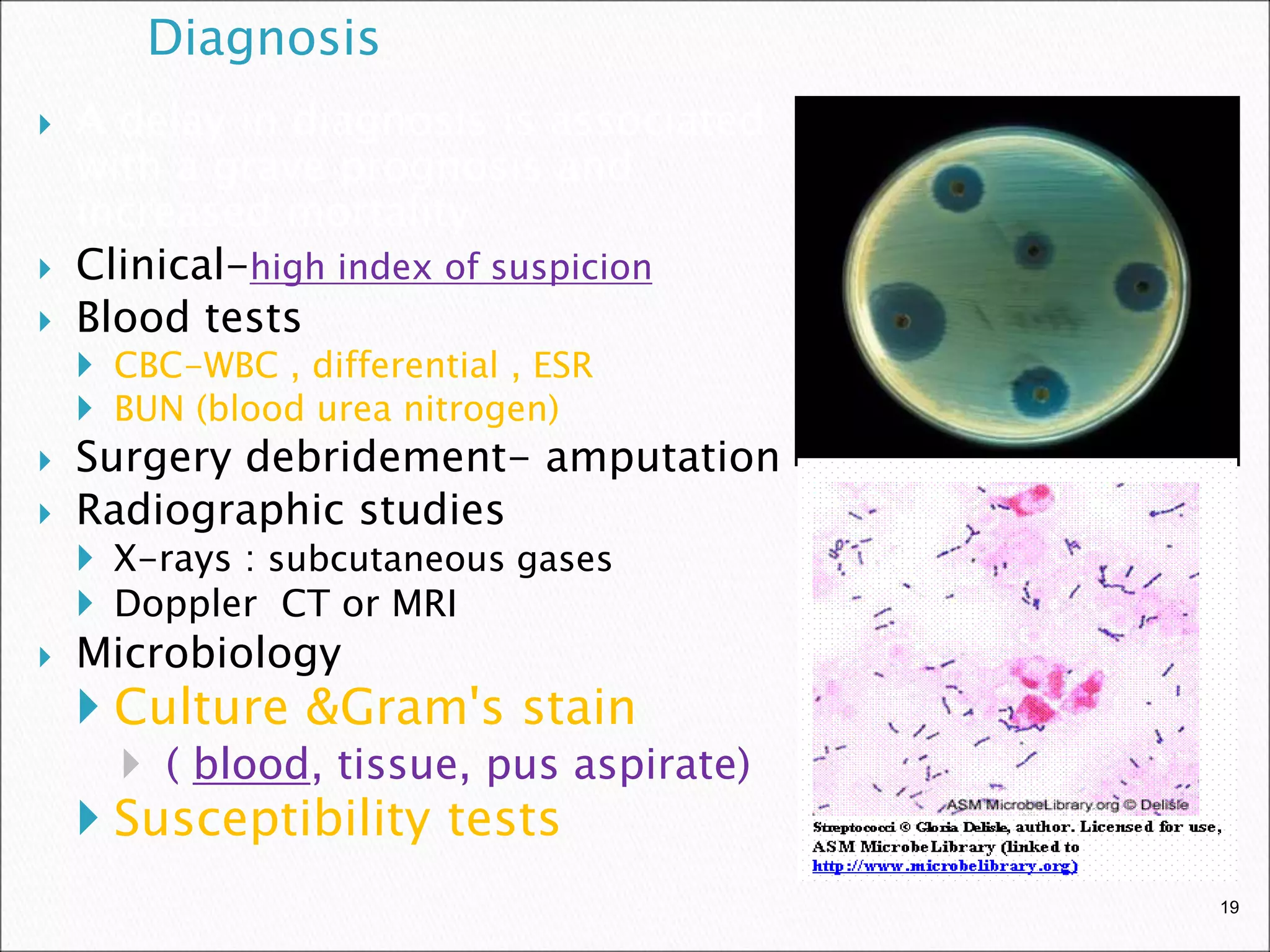
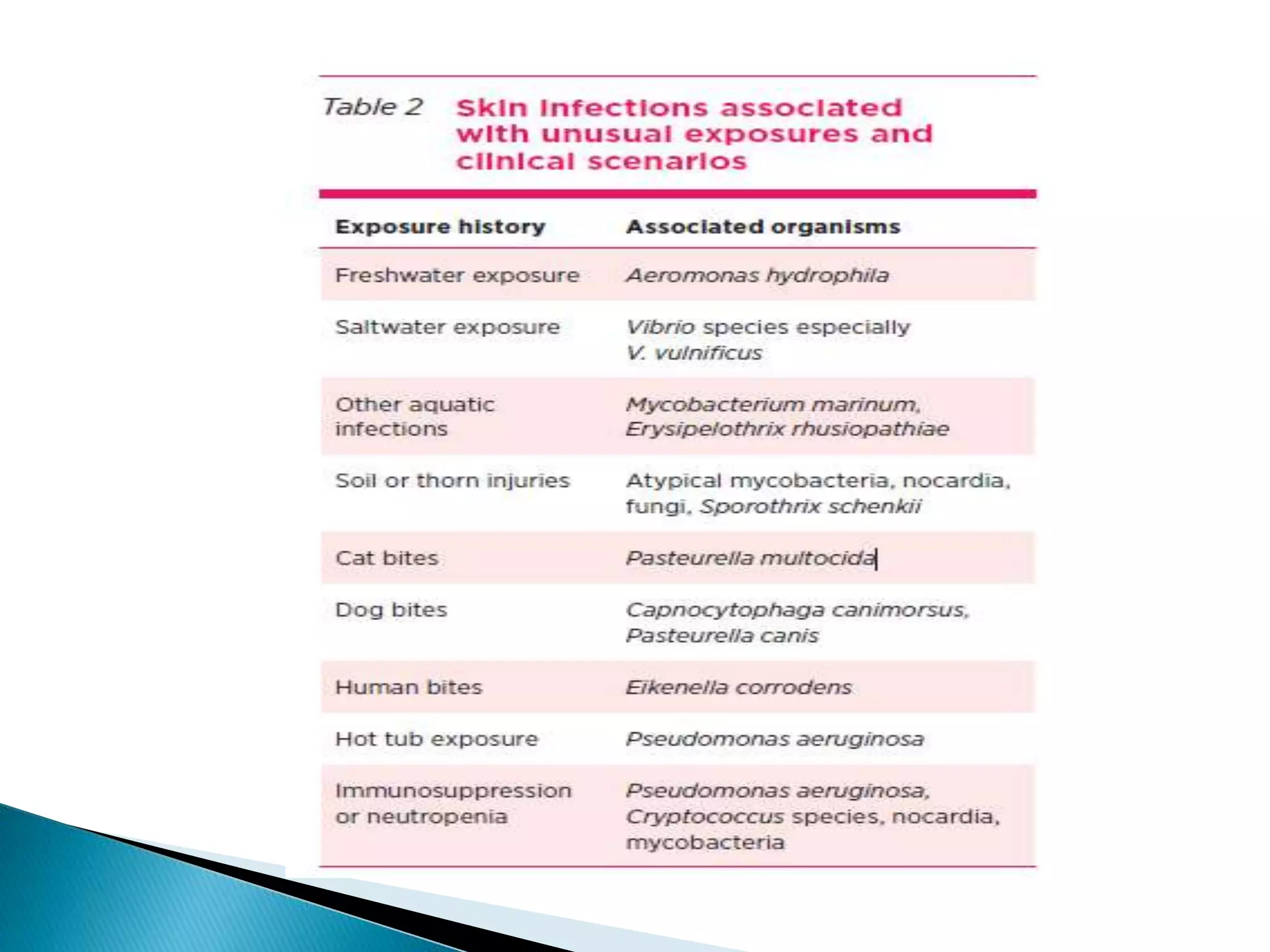
This document discusses various bacterial skin infections including erysipelas, impetigo, folliculitis, ecthyma, furuncles, carbuncles, cellulitis, necrotizing fasciitis, and pyomyositis. Erysipelas is a bacterial skin infection of the upper dermis caused by Streptococcus pyogenes. Impetigo is a superficial infection that presents as crusting or bullous lesions caused by Staphylococcus aureus or streptococcus. Folliculitis presents as pustules in hair-bearing skin and is usually caused by S. aureus. Cellulitis is a spreading skin infection of the deeper dermis and subcutaneous tissues caused by streptococci




































































































![ several underlying health conditions (such as
diabetes and kidney disease)
previous infections with methicillin-resistant
Staphylococcus aureus (MRSA)
intravenous [IV] catheters
recent hospitalizations
recent exposure to vancomycin and other
antimicrobial agents.](https://image.slidesharecdn.com/bacterialskinandsofttissueinfections-221025064116-4b5734b0/75/bacterial-skin-and-soft-tissue-infections-ppt-107-2048.jpg)

