Gingiva (Macroscopic features)
- 1. GINGIVA - (MACROSCOPIC FEATURES) - N.PREM KUMAR 1st year PG (PERIODONTICS)
- 2. CONTENTS : Introduction. Definition. Development of gingival tissues. Clinical features of gingiva. Pristine gingiva. Parts of gingiva. Colour. Contour. Surface texture. Size and shape. Position. Bleeding on probing. Age changes in gingiva. Implications. Conclusion.
- 3. INTRODUCTION : The Periodontium (peri = around , odontos = tooth) comprises of, Gingiva Periodontal ligament Cementum Alveolar bone
- 4. Function - To attach the teeth to the bone tissue of the jaws. Oral mucosa consists of following 3 zones : Masticatory mucosa (Gingiva and covering of hard palate) Specialized mucosa (Dorsum of tongue) Mucous membrane (Lining the remainder of the oral cavity)
- 5. DEFINITION : “The gingiva is the part of the oral mucosa that covers the alveolar processes of the jaws and surrounds the neck of the teeth”. “The gingiva is that part of the masticatory mucosa which covers the alveolar processes and surrounds the cervical portion of the teeth”.
- 6. DEVELOPMENT OF THE PERIODONTIUM NEURAL CREST DEVELOPMENT: By about 8 days of embryonic development, two distinct types of cells are produced, Ectoderm and Endoderm which forms a Bilaminar disc. By the 3rd week Mesoderm forms between these two layers. The ectoderm thickens and forms a raised margin to form Neural fold and ultimately to Neural tube by the next few weeks. From the neural crest, the neural crest cells develop.
- 9. By the 28th and 40th days of gestation Stomatodeum (primitive oral cavity) is formed. The epithelium of the stomatodeum contains the Superficial layer of flattened cells and Basal layer of columnar cells. The Neural crest cells migrate into 1st branchial arch, where they form a band of ectomesenchyme beneath the epithelium of the stomatodeum. Now the epithelium releases certain factors which initiate epithelial ectomesenchyme interactions. Now the ectomesenchyme takes the dominant role in the further development.
- 11. During 6th week of embryogenesis tooth development begins with the thickening of oral epithelium lining Stomatodeum to form Dental lamina. Once Dental lamina is formed, a series of process are initiated.(Bud stage, Cap stage and Bell stage with root development). During cap stage, condensation of ectomesenchyme cells in relation to epithelium forms, Dental papilla - (which gives raise to dentin and pulp) Dental follicle - (periodontal supporting tissues)
- 12. DEVELOPMENT OF GINGIVAL TISSUES : The Gingival tissues are composed of a, 1. Superficial epithelium - (Ectodermal origin) 2. Connective tissue - (Mesodermal origin)
- 13. The epithelium of gingival tissues consists of ; 1) Non-keratinised junctional epithelium - (From enamel organ) 2) Non – keratinised sulcular epithelium - (From oral mucosa) 3) Keratinised gingival epithelium - (From oral mucosa)
- 14. The gingival connective tissue is largely a fibrous connective tissue. Both epithelial and connective tissue attach to tooth via separate mechanisms. Epithelial tissues – interface with tooth by attachment called Junctional Epithelium which is located at (or) coronal to CEJ. Connective tissues attach to the root surface at or below the CEJ via fibres insertion into the cementum of the root surface.
- 16. The epithelial covering of the completely formed enamel has few layers of cells. These cells are called Reduced enamel epithelium. They originate from ameloblasts and cells of stratum intermedium of the enamel organ). It also includes remnants of stellate reticulum and outer enamel epithelium.
- 17. • These cells will eventually give rise to Junctional epithelium. • As the erupting tooth approaches the overlying epithelium, the cells of the REE proliferate and causing the epithelial covering of the enamel to thicken. • Proliferation of the cells begins at the cusp tips of the tooth and slowly progresses to the cervix of the tooth.
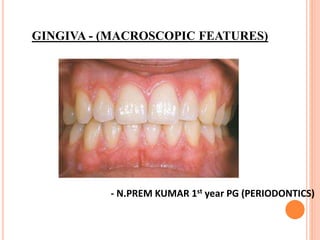
- 18. CLINICAL FEATURES OF THE GINGIVA : The healthy gingiva is coral pink (SALMON) and fully covers the root surface and supporting alveolar bone. It is characterised by an outer layer of stratified squamous epithelium and underlying connective tissue layer called lamina propria.(LINDHE et al) The gingiva obtains its final shape and texture in conjunction with eruption of the teeth. In the coronal direction it terminates in free gingival margin and covers the tooth to a level just coronal to the cementoenamel junction.
- 19. On the palatal aspect, the mucogingival line is absent as the gingiva here is continuous with the keratinised , non-mobile palatal mucosa. It may be pigmented, which is based on the ethnic origin of the people.
- 20. Pristine gingiva: A state of super health where normal gingiva is free from accumulation of inflammatory cells. Without any bacteria (0% bacteria) . It is seen only in infants. Goal of treatment is to achieve pristine gingiva but impossible.
- 21. Experimental gingivitis : Loe et al in 1965 demonstrated in students with clinically healthy gingiva : Clinical symptoms of gingivitis is developed in 2- 3 weeks if dental plaque was allowed to accumulate freely. But after adequate tooth cleaning, the gingival inflammation subsided within a week. The thickness of gingival plaque gradually increased within 3 weeks of time period. For first few days: Gram positive cocci Rods, representing the indegenous microflora of tooth surface.
- 22. After 4-5 days : Filamentous organisms. Gram negative cocci as well as rods. Non attaching spirochaetes were also developed in the sulcus. While the collection of micoorganisms in the biofilm increased continously.
- 23. PARTS OF THE GINGIVA: (SCHLUGER..ET AL,1990) The gingival tissues are anatomically subdivided into, 1. Marginal gingiva or Free gingiva. 2. Interdental gingiva. 3. Attached gingiva
- 24. MARGINAL GINGIVA : The marginal or unattached gingiva is the terminal edge or the border of the gingiva The free gingiva is coral pink, has a dull surface and firm consistency. (Lang) In about 50% of the cases, it is demarcated from the adjacent gingiva by a shallow linear depression called free gingival groove.
- 25. • The most apical point of the marginal gingiva scallop is called the gingival zenith. Its apicocoronal and Mesiodistal dimensions vary between (0.06 and 0.96mm).
- 26. The marginal gingiva is usually 1- 1.5mm wide and the inner wall forms the soft tissue wall of the gingival sulcus. It means when a probe is placed at the gingival margin in a healthy mouth, it can be inserted upto 3mm into the sulcus formed between the tooth and the mucosa, since soft tissue is movable.(kenhub) After complete tooth eruption, the free gingival margin is located on the enamel surface approximately (1.5-2mm) coronal to CEJ. (Lang)
- 27. GINGIVAL SULCUS : The gingival sulcus is the shallow crevice or space around the tooth bounded by the surface of the tooth on one side and the epithelium lining the free margin of the gingiva on the other side. It is V-shaped and barely permits the periodontal probe. Under normal conditions, the depth of the gingival sulcus is 0mm. In clinically healthy gingiva, a sulcus of some depth(Histological depth) can be found, it is around 1.8mm with variations from 0 to 6mm.(Also called Biologic depth) (Orban B et al, 1924)
- 29. Probing depth is the clinical evaluation used to determine the depth of the sulcus involves the introduction of metallic instrument called (periodontal probe) The so called probing depth of clinically normal gingiva sulcus in humans is 2-3mm. The probing depth usually depends upon 3 factors, Probe diameter. Probing force. Level of inflammation. It is not necessary that probing depth and biologic depth must be equal.
- 30. The sulcus has a depth of 3mm where food particles and bacteria can enter. This results in bacterial overgrowth and periodontitis.(ICOI) When gingiva is healthy, the pH of gingival sulcus is (6.9) The ecosystem of gingival sulcus is more anaerobic and the site is filled with Gingival crevicular fluid(GCF). GCF will be increased by 47% when gingivitis is present and to 30% when periodontitis is present. This is because GCF provides for cellular defense and humoral factors to combat against the microbial insult.(Marsh P)
- 32. Deepening of the gingival sulcus leads to periodontal pocket formation. Sulcus is the primary plaque forming domain and is the portal entry for periodontic pathogenic bacteria (i.e) porphyromonas gingivalis, aggregatibacter actinomycetumcomitans. (KvArun) Incase of periodontal pocket it is (7.4 – 7.8) (Van DykeTE, Dommisch H..et al,2018)
- 33. PATHOLOGY: Sulcus depth is chronically in excess of 3mm : The accumulated microbes will penetrate and ultimately destroy the delicate soft tissue and periodontal attachment fibers.(Chapple, Mealy BL..et al,2018)
- 34. Also result in recession, destruction of periodontium, tooth mobility and tooth loss.(Lang NP, Bartold PM..et al 2018) The depth of gingival sulcus is directly proportional to the severity of periodontitis.
- 35. ATTACHED GINGIVA : Orban(1948) was the first to describe attached gingiva. The attached gingiva is continuous with the marginal gingiva. • The dense connective tissue fibers of the attached gingiva ensure its firm attachment to the bone and “toughness”.
- 36. The attached gingiva is thus firmly entrenched between two movable structures, 1. The marginal gingiva – Coronally. 2. Alveolar mucosa – Apically. It is demarcated from the alveolar mucosa by mucogingival junction
- 37. BOUNDARIES: Facial aspect - Extend to relatively loose and movable alveolar mucosa. Lingual aspect – terminates at the junction of lingual alveolar mucosa, which is continuous with mucous membrane lining the floor of the mouth. (LOE H..et al,1996) Palatal aspect – blends imperceptibily with firm and resilient palatal mucosa.
- 38. WIDTH OFATTACHED GINGIVA : It refers to the apico-coronal dimension. (i.e) the distance between the mucogingival junction and the projection on the external surface of the bottom of the gingival sulcus. Average thickness of attached gingiva is 1.25mm. The width varies in different area of the mouth : Greater in the incisor region : 3.5mm to 4.5mm in maxilla anterior. 3.3mm to 3.9mm in mandibular anterior. Narrower in the posterior region : 1.9mm in maxillary posterior. 1.8mm in mandibular posterior.
- 39. The width is often least in the premolar region due to the presence of accessory frenae in those areas. With the progression from primary to permanent dentition the width of attached gingiva is decreased.
- 40. The width increases around 4 years of age and in Supraerupted teeth due to passive eruption.(Ainamo J) The mucogingival line remains stationary throughout life that separates not only the attached gingiva from the alveolar mucosa, but also the alveolar process from the basal bone.(Talari A)
- 41. BIOLOGIC WIDTH : GARGIULO ET AL,1961 The dimension of epithelial attachment , which is attached to the portion of the tooth coronal to the crest of the alveolar bone. In 1977, Ingber et al. described "Biologic Width" and credited D.Walter Cohen for first coining the term. A sulcus depth (0.69 mm) an epithelial attachment (0.97 mm) and a Connective tissue attachment of (1.07 mm). So, Biologic width is commonly stated to be 2.04 mm, which represents the sum of the epithelial and connective tissue measurements. Essential for preservation of periodontal health and removal of irritation that might damage the periodontium (prosthetic restorations).
- 43. THE SIGNS OF BIOLOGIC WIDTH VIOLATION ARE: Chronic progressive gingival inflammation around the restoration. Bleeding on probing. Localized gingival hyperplasia with minimal bone loss. Gingival recession. Pocket formation. Clinical attachment loss and alveolar bone loss. Gingival hyperplasia is most frequently found in altered passive eruption and subgingivally placed restoration margins.
- 44. MEASUREMENT OF WIDTH OF ATTACHED GINGIVA : Methods to determine mucogingival junction : Visual method. Functional method. Visual methods after histochemical staining. Assessed as a borderline between movable and immovable tissue. Tissue mobility is assessed by running a horizontally positioned probe from the vestibule towards the gingival margin using light force.
- 45. Assessed visually after staining the mucogingival junction with ( Schiller’s potassium iodide solution ): (KI) solution do not stain the keratinized epithelium;(i.e) marginal gingiva, attached gingiva and interdental papilla. But stains the Alveolar mucosa because, it differs from keratinized gingiva histochemically 1. Glycogen content 2. Acid phosphatase and nonspecific esterase content 3. Increased amount of elastic fiber content within the corium resulting in an iodo-positive reaction.
- 46. The attached gingiva, which is keratinized, has no glycogen in the most superficial layer and gives an iodo-negative reaction. Thus the solution stains only the Alveolar mucosa and clearly demarcates the mucogingival junction. The total width of gingiva is measured that is from gingival margin to mucogingival line. [ Stained total gingival width - pocket depth gives = Width of attached gingiva ]
- 47. INADEQUATE WIDTH: (ERICSSON I , LINDHE J..ET AL) Inadequate width of gingiva may facilitate subgingival plaque formation because of improper pocket closure resulting from the movability of the marginal tissue. PULL OF GINGIVAL MARGIN : Insufficient attached gingiva (causing recession and bone loss) Abnormal frenal attachment. Deep pockets that reach the level of mucogingival junction. Vigorous brushing in people with naturally thin tissue.
- 49. (Miyasato et al) concluded that there is no relationship between inflammation and amount of attached gingiva whether or not plaque is present. (De tray and Berimoulin) adequacy of attached gingiva cannot be determined by measurement of its width alone.
- 50. INTERDENTAL GINGIVA : The interdental gingiva occupies the gingival embrasure which is the interproximal space beneath the area of the tooth contact. It can be “pyramidal” or it can have a “col” shape. It presents a valley like depression that connects the facial and lingual papilla. The shape of gingiva in a given interdental space depends upon the presence or absence of contact point between adjacent teeth.
- 51. The lateral borders and tips of interdental papillae are formed by the marginal gingiva of the adjoining teeth. The interwining portion consists of attached gingiva. Incase of diastema, the gingiva is tightly bound to the underlying interdental bone to form a smooth, rounded surface without interdental papillae.
- 52. Anterior – Pyramidal form. Molar – Flatter in buccolingual direction. Premolar – Since these teeth have approximal contact surfaces rather than contact points so, col shape is established in these regions.(Lang Lindhe)
- 53. INTERDENTAL RECESSION : (KIA REZAVANDI,..ET AL2016) In the esthetic zone, the loss of interdental papilla height can be unsighty. The two most frequenty qouted factors influencing the papilla height are the 1) Types of Gingival biotype. 2) Position of contact point.
- 54. GINGIVAL BIOTYPE : (OCHSENBEIN C, ROSS S, SEIBERT JL, LINDHE J,ET AL ) Oshsenbein and Ross in their pioneer study indicated that there were two main types. 1) Scalloped and thin 2) Flat and thick.
- 55. So the gingival biotype means, the thickness of the gingiva in the facio-palatal dimension. Later the term “periodontal biotype” was introduced by Seibert and Lindhe. But the “periodontal biotype” not only includes thickness of gingiva but also contour, alveolar bone thickness, amount of keratinised gingiva present and crown shape. Gingival biotype may differ from tooth to tooth in a person and may also differ with age, gender and dental arch location.
- 56. Based on consensus published on 06 November 2019 by (David M. Kim , Seyed Hossein Bassir ,Thomas T. Nguyen) The 2017 World Workshop on the Classification of Periodontal and Peri‐Implant Disease and Conditions has recommended adoption of the term “periodontal phenotype” by the periodontal community.
- 57. THIN AND SCALLOPED TYPE : Have delicate and thin periodontium. Highly scalloped gingival tissue. Small incisal contact areas. Triangular crowns. Thin and translucent appearance. Tissue is friable with minimal zone of attached gingiva. Soft tissue is highly accentuated. Thin or minimal bone over the labial roots. Surgical exposure cause highly incidence of fenestration and dehiscence. Prevalance of thin biotype is 43 percent.
- 58. THICK AND FLAT TYPE : Thick and heavy periodontium. Wide zones of keratinized gingiva. Flat gingival contour, thick flat osseous gingival contour. Broad apical contact areas in teeth and square anatomic crown. Tissue is dense with wide zone of attached gingiva. The underlying bony architecture is thick. Surgical exposure demonstrate thick underlying osseous forms. Prevalence – 56 percent.
- 59. CLASSIFICATION Authors Classification 1) Ochsenbein and Ross(1969) Scalloped and thin Flat and thick 2) Seibert and Lindhe(1989) (Thick) ≥ 2mm (Thin) < 1.5mm 3) Becker et al(1997) Flat: 2.1mm Scalloped : 2.8 mm Pronounced scalloped : 4.1 mm 4) Kan et al(2010) Thick > 1mm Thin ≤ 1mm 5) Claffey and Shanley(1986) Thick ≥ 2mm Thin < 1.5mm 6) Egreja et al(2012) Thick >1mm Thin < 1mm
- 60. Both type respond differently to clinical and surgical insults. In the event of inflammation or any insults , soft tissue in thick biotype respond more of fibrotic changes and pocket formation. In thin, more inflammatory and recession of gingiva. Patients with thin type are more vulnerable to connective tissue loss and epithelial damage. Thus they need special treatment and oral hygiene instructions.
- 61. METHODS OF MEASUREMENT : 1) Direct measurement : Accurate measurement however inavasive technique using topical anaesthetic gel , endodontic reamer and caliper. It is measured from center of gingival margin and mucogingival junction in perpendicular direction.
- 62. 2) Visual examination - Very low accuracy and variation. Clinically evaluated based upon the general appearances of gingiva : 1) Thick – dense and fibrotic. 2) Thin – delicate, friable almost translucent
- 63. OTHER METHODS INCLUDE: Probe transparency Ultrasonic device CBCT. TRAN
- 64. SIGNS OF HEALTHY INTERDENTAL PAPILLA : 1. Healthy pigmentation 2. Firm attachment. 3. Triangular shape. 4. Pain and blood free. A distance of upto 5mm between the contact point and the interdental bone crest is considered as full interdental papilla height.(Tarnow et al)
- 65. In more recent study, the critical measurement for a complete papilla is 6mm from the tooth bone crest and 8.5mm from the implant bone crest to contact point. (Palmer et al) When distance is : 1. 5mm – 98 % papilla was present. 2. 6mm – 56 %. papilla was present. 3. 7mm – 27 %. papilla was present.
- 66. LOSS OF INTERDENTAL PAPILLA : (RES J, 2013) Plaque associated lesions. Traumatic oral hygiene procedures. Abnormal tooth shape. Improper contours of restoration. Spacing Loss of teeth.
- 67. Classification of loss: (Norland and Tarnow,et al 1998) Class 1 : Tip lies between the interdental contact point and the coronal extent of CEJ. Class 2 : Tip lies at or the apical to CEJ, but coronal to the apical extent of facial CEJ. Class 3 : the tip lies at the level with or apical to the facial CEJ.
- 68. RECONSTRUCTION OF LOST PAPILLA : Non surgical techniques Treatment : Traumatic procedures must be initially discontinued and successively modified. Re-epithelialization of the traumatic lesion can restore papilla.
- 69. Restorative : Abnormal tooth shape cause missing papilla. So appropriate restorative technique is indicated. By restoration, the contact point may be lengthened and located more apically; embrasure is reduced. Orthodontic : The aim is to reduce the diastema and create contact point. Coronal movement of tooth through orthodontic appliance cause alterations, changes in bone level, soft tissue contour, creating new papillae.(Ingber)
- 70. Surgical techniques : 1. Papilla – recontouring. 2. Papilla – preservation. 3. Papilla – reconstruction. Han and Takei ‘Semilunar Coronally Advanced Flap’. Azzi et al Envelope flap technique. Takei et al. in 1985 introduced conventional papilla preservation technique. Cortellini et al. (1995) introduced a new modification of conventional papilla preservation flap. Bianchi and Basseti in 2009 introduced a technique known as Whale’s tail technique.
- 72. CORRELATION OF CLINICAL AND MICROSCOPIC FEATURES. Colour : Normal gingiva is coral pink in color. There are four factors that determine the colour of the gingiva, they are, 1. Vascular supply. 2. Thickness of the epithelium. 3. Degree of keratinization. 4. Physiologic pigmentation.
- 73. Vascularity determines the basic colour of the gingiva which undergoes modification depending on, 1. Degree of keratinization. 2. Presence of pigments. Physiologic pigmentation (Melanin) : Melanin is a non hemoglobin – derived brown pigment with following characters ; 1. Responsible for the pigmentation of the skin, the gingiva and remaining oral mucous membrane. 2. Absent or severely diminished in albinos. 3. Pigmentation is higher in oral cavity of black individuals. 4. Ascorbic acid down regulates the pigmentation in gingival tissues.
- 74. The distribution of pigmentation in black individuals is, 1. Gingiva- 60 %. 2. Hard palate- 61% 3. Mucous membrane – 22% 4. Tongue – 15%
- 75. Appearance : Occurs as a diffuse, deep purplish discoloration or as irregularly shaped brown and light brown patches. It may appear in the gingiva as early as 3hours after birth. Oral repigmentation : Clinical reappearance of melanin pigment after a period of clinical de-pigmentation of the oral mucosa. Result of chemical, thermal, surgical, pharmacologic or idiopathic factors.
- 76. Colour in diseased conditions : 1. Chronic inflammation – appears reddish pink/ bluish in colour. 2. Acute inflammation – appears bright red in colour. o These changes are due to increased blood flow, increased permeability of capillaries and increased collection of defense cells and tissue fluid.
- 77. DISEASE COLOUR CHANGES Chronic gingivitis Reddish pink / bluish Acute gingivitis Bright red ANUG/ HIV Shiny slate gray Herpetic gingivostomatitis Dull whitish gray Smoking / trauma White Mild inflammation Pale red
- 80. ORAL PIGMENTATION INDEX – DUMMET ET AL (1964) SCORE CLINCIAL ASPECT 0 Pink gingiva (No clinical pigmentation) 1 Mild light brown colour (Mild clinical pigmentation) 2 Medium brown or mixed pink and brown colour (Moderate clinical pigmentation) 3 Deep brown or bluish black colour (Heavy clinical pigmentation)
- 81. CONDITIONS : Diseases that increase melanin pigmentation include the following : 1) Addison disease : (Adrenal dysfuntion) - produces isolated patches of discoloration that vary from bluish black to brown colour. 2) Peutz – jeghers syndrome : - produces intestinal polyposis and melanin pigmentation in oral mucosa and lips. 3) Albright syndrome or Polyostotic fibrous dysplasia 4)Neurofibromatosis or Von reck – linghausen disease They both produce oral pigmentation.
- 82. Addison disease Albright syndrome Peutz – jeghers syndrome Neurofibromatosis
- 83. Kaposi’s sarcoma Cushing syndrome Malignant melanoma Blue nevus
- 84. Endocrinopathic pigmentation: 1) Addison disease. 2) Cushings syndrome. Vascular lesion : 1) Kaposi’s sarcoma : -Oral mucosa is red , blue, and purple . -Hard palate is most favourable sight. Brown melanotic lesions: 1) Nevo cellular lesion. 2) Blue nevus. 3) Malignant melanoma.
- 85. CONTOUR : Normal gingiva has an arcuate contour with a scalloped outline and a knife edge margin. The contour or shape of the gingiva varies considerably and depends on the , shape of the teeth. Their alignment in the arch. The location and the dimensions of the facial and lingual embrasures.
- 86. 1. It follows a scalloped outline on the facial and lingual surfaces. 2. It forms a straight line along teeth with relatively flat surfaces. In canine and labial teeth : They have pronounced mesiodistal convexity. In these teeth, the normal arcuate contour is located farther apically.
- 87. In lingual teeth : The gingiva is horizontal and thickened. In addition, the gingiva biotype varies significantly.
- 88. In health : 1. Marginal gingiva – Scalloped and knife edged. 2. Interdental papilla – (Anterior) : Pyramidal shape. (Posterior) : Col shaped
- 89. In Diseased conditions : :Chronic gingivitis : - Marginal gingiva becomes Rounded and Bulbous. - Interdental papilla becomes Flat and Blunt. ANUG : Punched out crater like depression at the end crest of interdental papilla extending to marginal gingiva Stillman’s cleft : Exaggerated scalloping apostrophe shaped intendations extending from and into the gingival margin for varying distance on the facial surface. McCall’s festoon ; Life saver like enlargement of marginal gingiva. Chronic Desquamative gingivitis : Irregular denuded appearance.
- 90. ANUG Chronic Desquamative gingivitis Chronic gingivitis
- 91. SURFACE TEXTURE The gingiva presents a textured surface similar to that of an orange peel appearance and is referred to as Stippled. It varies among different individual and different areas of mouth.(LOE H..et al,1996). Stippling is viewed by drying the gingiva. This occurs as a result of the epithelial retepegs in growth in connective tissue.
- 92. The papillary layers of connective tissue extends into the epithelium and this feature is known as stippled appearance. 1. Marginal gingiva is not stippled. 2. Attached gingiva is stippled. 3. Central portion of Interdental papillae is stippled, but margins are smooth.
- 93. Differences : i. Stippling is less prominent on lingual surfaces. ii. Stippling varies with age. It is absent during infancy, appears in some children at about 5 years of age. iii. Increases in adulthood and disappears in old age. Microscopic feature : Microscopically, stippling is produced by alternated rounded protuberances and depressions in the gingival surface. The elevated and depressed layers are covered by stratified squamous epithelium.
- 94. Functions : It is a form of adaptive specialization or reinforcement for function to withstand mechanical stresses. On a study , gingival stippling was found to be a normal characteristic in 56 percent of 3 to 10 year old children, without significant difference in arch , gender or age.( J Clin Pediatr Dent, 2003)
- 95. Loss of stippling : It is common sign of gingival disease. It is reversible in nature. It has been observed in a study where , thick gingiva has coarse and diffuse stippling, whereas thin gingiva has fine and scanty stippling.
- 96. STUDY AUTHORS : Thushara Mohanan, Vanadana KL,..et al 2020 The study was about evaluation of gingiva, where 180 sites were examined in 15 patients aged 17-25 years. Result : Out of 50, (27.7 percent) sites had coarse dense stippling 13.3 percent sites had thin gingiva(1mm) 14.44 had thick gingiva (1mm)
- 97. SIZE Size of the gingiva corresponds with the sum total of the bulk of cellular and intercellular elements and their vascular supply. The size of gingiva is increased in some conditions that are called Gingival enlargement. Size : 0-2mm for Marginal gingiva. 0-9mm for Attached gingiva. Disease : Inflammatory – increased in cells and decrease in fibers. Non inflammatory – decrease in cells and increase in fibers.
- 99. SHAPE Shape of gingiva depends upon, 1. Contour of proximal tooth surface. 2. Location and shape of gingival embrasures. Hence in , Anterior region – Pyramidal shape. Posterior region – More flat in buccolingual direction.
- 100. Anterior Tooth Posterior Tooth Proximal surface of crowns are flat faciolingually. Proximal surface flare away from area of contact Interdental bone is thin mesiodistally. Mesiodistal diameter of the interdental gingiva is broad. Interdental gingiva is narrow mesiodistally. The height of the interdental gingiva varies with the location of the proximal contact.
- 101. CONSISTENCY : The gingiva is firm and resilient and with the exception of the movable free margin, tightly bound to the underlying bone. The collagenous property of lamina propria and its contiguity with the mucoperiosteum of the alveolar bone determine the firmness of the attached gingiva. The gingival fibers contribute to the firmness of the gingival margin and also cellular and fluid content of the tissue.
- 103. In Diseased condition: Gingiva is soft and spongy increased fluid (edema) red, smooth, shiny bleeds easily. Flabby due to connective tissue loss. Chronic gingivitis : (Inflitration by fluids and cells)- Soggy puffiness. Acute gingivitis : Vesicle formation. Fibrotic condition : - Firm leathery. Diffuse puffiness. Sloughing. Exudative :Marked softness and friability.
- 104. POSITION : The position of the gingiva is the level at which the gingival margin is attached to the tooth. The position of the gingiva is usually 1.5- 2mm above the cementoenamel junction. Factors responsible for position : Position of tooth in the arch. Root bone angle. Mesiodistal curvature of tooth surface. Formation of position : When the tooth erupts into the oral cavity the margin and the sulcus are at the tip of the crown.
- 105. As the eruption progresses, they are seen closer to the root. During this eruption process, the juntional epithelium, undergo extensive alterations and remodeling. Thus maintaining the shallow physiologic depth of the sulcus. Without this remodeling, an abnormal anatomic relationship between the gingiva and tooth would result. In disease : Gingival recession : Due to tooth brush trauma caused by abnormal or faulty methods. Pseudopockets : Due to gingival inflammation, high frenum attachment, tooth malposition and friction from soft tissue.
- 106. Tooth brush trauma Gingival inflammation High frenal attachment
- 107. BLEEDING ON PROBING : During probing for examination of sulcular depth, bleeding occurs, this is due to intact sulcular epithelium and normal capillaries. Whereas in chronic gingivitis, bleeding on probing is present due to dilation and engorgement of capillaries and thinning. Similarly in ANUG and systemic diseases, chronic recurrent bleeding in seen and spontaneous or slight bleeding is seen. Ulceration of sulcular epithelium may also cause bleeding on probing.
- 108. AGE CHANGES IN GINGIVA The gradual changes taking place in the dental tissues after the teeth are fully formed is known as age changes. Comfort (1956) defined aging as a biological process that causes increased susceptibility to disease. Gottlieb & Orban – Believed that with age, gingival recession and alveolar bone resorption occur and termed it as Senile Atrophy.
- 109. People aged 65-74 are young elderly. People aged 75-84 are old or mid old. People above 85 years are oldest-old. Gingival epithelium changes : Thinning and decrease in keratinization of the gingival epithelium have been reported with age. This results increase in epithelial permeability to bacterial antigens, a decreased resistance to functional trauma or both. If so, such changes may influence long term periodontal outcomes. Flattening of rete pegs and altered cell density.
- 110. Junctional epithelium : Migration of junctional epithelium from to more apical position on the root surface with accompanying gingival recession. The width of attached gingiva increases with age. The migration of junctional epithelium to the root surface could be caused by (passive eruption) as a result of tooth surface loss from attrition.
- 112. TOOTH PERIODONTIUM RELATIONSHIP: The reduction in bone height that occurs with aging. Bone loss results in an increase in crown to root ratio. Wear of teeth also occurs on the proximal surfaces accompanied by mesial migration of teeth. Proximal wear reduces the Anteroposterior length of dental arch by 0.5cm in age of 40.
- 113. Progressive alteration - Maxillary-Mandibular overjet in the molar area. Proximal wear – Edge to edge bite Anteriorly. Increased role for Porphyromonas gingivalis and decreased role for Aggregatibacter actinomycetemcomitans.
- 114. EFFECTS OF AGING ON THE PROGRESSION OF PERIODONDAL DISEASES In a classic experimental gingivitis study, subjects were rendered plaque and inflammation free through frequent professional cleaning. Later the subjects are stopped from oral hygiene measures for periods of 3 weeks to allow gingivitis to develop. A comparison of gingivitis between young and older individuals demonstrated a greater inflammatory response in older age. Findings included a greater size of infiltrated connective tissue, increased gingival crevicular fluid flow and increased gingival index.
- 115. IMPLICATIONS DEFENSIVE FUNCTIONS OF ATTACHED GINGIVA It prevents deflection of marginal gingiva thus aids in plaque maintenance. By preventing this deflection, it also helps avoid food entrapment between tooth and gingival sulcus. The dense collagenous structure of the attached gingiva also aids in slowing down the inflammatory spread from the marginal gingiva.
- 116. Attached gingiva aids in : Increase resistance to external injury and contribute in stabilization of gingival margin. Acts against frictional forces. Dissipating physiological forces.
- 117. CLINICAL SIGNIFICANCE OF ATTACHED GINGIVA AROUND IMPLANTS : (METTEST RM, LANGER B..ET AL) I. Prevent spread of inflammation. II. Prevent recession of marginal tissue. III. Provides tight collar around implants. IV. Enable patients to maintain good oral hygiene.
- 118. ROLE OF CONTOUR IN GINGIVAL HEALTH (SYDNEY S .WAGMAN) Total clinical crown contour is related to gingival health. The subgingival convexity of a tooth or a restoration should extend facially or lingually no more than one half of the thickness of the gingiva. This protects the gingival crevice and promotes a knifelike free margin, important plaque control.
- 119. REFERENCES : Newman and Carranza’s clinical periodontology(13th edition). Clinical periodontology and implant dentistry by Jan Lindhe, Niklaus P.Lang(6th edition). Molecular biology of periodontium (KV Arun). Biology of periodontal connective tissues (P.Mark Bartold.PhD and A.Sampath Narayanan. PhD) Shirmohammadi A, Faramarzie M, Lafzi A. A clinical evaluation of anatomic features of gingiva in dental students in Tabriz, Iran. Journal of dental research, dental clinics, dental prospects. 2008;2(3):90. Singh S, Vandana KL. Assessment of width of attached gingiva in primary, mixed, and permanent dentition: Part-2. SRM Journal of Research in Dental Sciences. 2017 Oct 1;8(4):157.
- 120. Shah R, Sowmya NK, Thomas R, Mehta DS. Periodontal biotype: Basics and clinical considerations. Journal of Interdisciplinary Dentistry. 2016 Jan 1;6(1):44. Vandana KL, Shivani S, Savitha B, Vivek HP. Assessment of gingival sulcus depth, width of attached gingiva, and gingival thickness in primary, mixed, and permanent dentition. Journal of Dental Research and Review. 2017 Apr 1;4(2):42. Shah R, Sowmya NK, Thomas R, Mehta DS. Periodontal biotype: Basics and clinical considerations. Journal of Interdisciplinary Dentistry. 2016 Jan 1;6(1):44. Ughabharathy R, Balu P, Muthu J, Saravanakumar R, Vineela K, Karthikeyan I. Clinical evaluation of increase in the width of attached gingiva using modified apically repositioned flap: A 9-month follow-up study. Contemporary clinical dentistry. 2018 Apr;9(2):200. Nadkarni MA, Chhour KL, Browne GV, Byun R, Nguyen KA, Chapple CC, Jacques NA, Hunter N. Age-dependent changes in Porphyromonas gingivalis and Prevotella species/phylotypes in healthy gingiva and inflamed/diseased sub- gingival sites. Clinical oral investigations. 2015 May 1;19(4):911-9.
- 121. Sharma A, Singal V. Connective tissue: A gold standard for reconstruction of black triangle. Journal of Current Research in Scientific Medicine. 2017 Jul 1;3(2):111. Bimstein E, Peretz B, Holan G. Prevalence of gingival stippling in children. Journal of Clinical Pediatric Dentistry. 2004 Jan 1;27(2):163-5. KS P. Prevalence of Gingival Stippling among 4-8 Years Old Children. Kan JY, Morimoto T, Rungcharassaeng K, Roe P, Smith DH. Gingival biotype assessment in the esthetic zone: visual versus direct measurement. International Journal of Periodontics & Restorative Dentistry. 2010 May 1;30(3). Jamwal D, Kanade K, Tanwar VS, Waghmare P, Landge N. Treatment of Interdental Papilla: A Review. Shirmohammadi A, Faramarzie M, Lafzi A. A clinical evaluation of anatomic features of gingiva in dental students in Tabriz, Iran. Journal of dental research, dental clinics, dental prospects. 2008;2(3):90.
- 122. THANK YOU !
