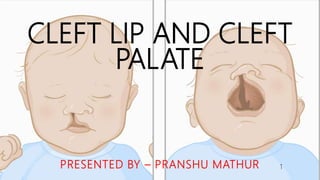
Cleft Lip and Cleft Palate
- 1. CLEFT LIP AND CLEFT PALATE PRESENTED BY – PRANSHU MATHUR 1
- 2. CONTENTS • Introduction • Embryology • Classification • Epidemiology • Etiology • Problems associated with cleft • Diagnosis • Management 2
- 3. INTRODUCTION •Cleft lip and palate is the most common developmental anomaly of the craniofacial region, and they have been depicted throughout in the past civilizations. •Records suggest that hare lip was reported as far back as 1000 AD . 3
- 4. • Cleft lip and cleft palate, also known as orofacial cleft, is a group of conditions that includes cleft lip, cleft palate, and both together. • A cleft lip contains an opening in the upper lip that may extend into the nose. The opening may be on one side, both sides, or in the middle. • A cleft palate occurs when the roof of the mouth contains an opening into the nose. • These disorders results in feeding problems, speech problems, hearing problems, and frequent ear infections. Less than half the time the condition is associated with other disorders. 4
- 5. EMBRYOLOGY 5
- 6. DEVELOPMENT OF FACE • After formation of head fold, the developing brain and the pericardium form two bulgings on the ventral aspect of the embryo. • The bulgings are separated by the STOMATODAEUM. • The floor of the stomatodaeum is formed by the buccopharyngeal membrane, which separates it from the foregut. 6
- 7. • Soon, the mesoderm covering the developing forebrain proliferates and forms a downward projection that overlaps the upper part of stomatodaeum – FRONTONASAL PROCESS. • Frontonasal Process forms by early 4th week 7
- 8. • The face is derived from the following structures that lie around the stomatodaeum – Frontonasal process – 1st pharyngeal (mandibular) arch of each side – forms the lateral wall of the stomatodaeum. 8
- 9. • The mandibular arch gives off a bud from its dorsal end – MAXILLARY PROCESS. (Early 4th week) • It grows ventro – medially cranial to the main part of the arch – MANDIBULAR PROCESS. (Early 4th week) 9
- 10. • The ectoderm overlying the frontonasal process shows bilateral localized thickenings (a little above the stomatodaeum) – NASAL PLACODES. (Late 4th week.) 10
- 11. • Nasal Placodes soon shrink to form NASAL PITS (external nares). • The edges of each pit are raised above the surface : a. the medial raised edge – MEDIAL NASAL PROCESS. b. the lateral edge – LATERAL NASAL PROCESS. • Nasal Processes form by Early 5th week. 11
- 12. DEVELOPMENT OF LOWER LIP • The mandibular processes of both the sides grow towards each other. • They now form the lower border of the stomatodaeum. • Fused mandibular process give rise to the lower lip and lower jaw. (Early 5th week) 12
- 13. DEVELOPMENT OF UPPER LIP • Each maxillary process now grows medially and fuses, first with the lateral nasal process and then with the medial nasal process. (Late 5th week) • The lateral and medial nasal processes also fuse with each other. Thus the nasal pits are cut off from the stomatodaeum. 13
- 14. • The maxillary processes undergoes considerable growth. • At the same time, the frontonasal process becomes much narrower from side to side, with the result that two external nares comes closer together. • Finally the upper lip is formed by the contribution from – a. Lateral part by the right and the left maxillary processes. b. Median part of the lip (called the Philtrum) by the narrowing of the frontonasal process. • Philtrum and upper lip are completed by Early 7th week. 14
- 15. DEVELOPMENT OF PALATE • The palate starts to form during the fifth and sixth week. It is derived from the following structures – a) 2 medial nasal processes (MNP) b) 2 maxillary processes • The primary palate forms first. • During the 5th week of IU like, the MNPs on both the sides extend backwards in the oral cavity for a short distance and fuse in the midline to give rise to the primary palate. 15
- 16. • During the 7th week, two palatal processes evolve as outgrowth from maxillary processes, one on each side, and develop downward on either side of the developing tongue. 16
- 17. • Later, with the expansion and growth of stomatodaeum, the tongue descends downwards allowing the vertically developing palatal shelves to elevate and approach each other in the midline. 17
- 18. 18
- 19. • If there is any disturbance in the fusion of the lateral and medial nasal processes with the maxillary process, there will a CLEFT LIP formation. • If cleft of lip extends deep into primary palate, it results in cleft of alveolus too. • Whereas, if the 2 palatal shelves do not fuse, there is a CLEFT PALATE formation. • Occasionally, cleft of lip and alveolus may have bands of soft tissue bridging across the two sides called simonnarts band. 19
- 20. CLASSIFICATION OF CLEFT LIP AND PALATE 20
- 21. MORIAN’S CLASSIFICATION (1886) • Morian is credited with the first attempt to classify craniofacial anomalies. • He described three types of facial clefts – • Type I (oronasal cleft) – described a maxillary cleft located between the central and the lateral incisors. • Type II (oroocular cleft) – described a maxillary cleft located between the incisor and the canine teeth. • Type III (oroocular cleft) – described a maxillary cleft located behind the canine teeth 21
- 22. DAVIS AND RITCHIE CLASSIFICATION (1922) • Davis and Ritchie’s classification was based on a proper conception of congenital cleft of the lip and palate. • This classification was divided into 3 groups – • Group I. Pre-alveolar cleft. (Lip cleft; alveolar process normal.) • 1. Unilateral. Right. Left. Complete. Incomplete. • 2. Bilateral. Right : Complete ; incomplete. Left : Complete ; incomplete. • 3. Median (rare). Complete. Incomplete. Cleft of the palate may be associated with this group. 22
- 23. • Group II. Postalveolar (process) cleft. (Palate cleft; alveolar process normal.) 1. Soft palate. (The uvula only, or the entire soft palate, may be cleft.) 2. Hard palate. (May be notch only, or cleft may extend to the anterior palatine foramen, in addition to the soft palate.) Cleft of the lip may be associated with this group. • Group III. Alveolar (process) cleft. (Cleft follows incisor sutures.) 1. Unilateral. Right: Complete; incomplete. Left: Complete; incomplete. 2. Bilateral. Right : Complete ; incomplete. Left : Complete; incomplete. 3. Median (rare). Complete. Incomplete. Clefts of the lip and palate are usually associated in this group. 23
- 24. VEAU’S CLASSIFICATION (1931) Victor Veau in 1931 put forth a classification of cleft lip and palate which was divided into four types as shown - 24
- 25. CLASSIFICATION BY FOGH ANDERSON (1942) • Fogh Anderson gave a very similar classification based on embryological development , which is as follows: Group 1 – clefts of the lip- unilateral or bilateral; Group 2 – clefts of the lip and cleft palate (single or double); Group 3 – clefts of the lip and palate upto the incisive foramina 25
- 26. KERNAHAN AND STARK CLASSIFICATION (1958) 26
- 27. 27
- 28. 28
- 29. AMERICAN ASSOCIATION OF CLEFT PALATE AND REHABILITATION (1962) • Harkins and associates (1962), presented a classification of facial clefts: 1. Cleft of Primary Palate (cleft of lip and embryologic primary palate) A. Cleft Lip (cheiloschisis) 1) Unilateral: right, left (a) Extent: one-third, two-thirds, complete 2) Bilateral: (a) Extent: one-third, two-thirds, complete 3) Median (a) Extent: one-third, two-thirds, complete 4) Prolabium: small, medium, large 5) Congenital scar: right, left, median (a) Extent: onethird, two-thirds, complete 29
- 30. 30
- 31. B. Cleft of Alveolar Process (alveoloschisis) 1) Unilateral: right, left (a) Extent: one-third, two-thirds, complete 2) Bilateral: (a) Extent: one-third, two-thirds, complete 3) Median (a) Extent: one-third, two-thirds, complete 4) Submucous: right, left, median 5) Absent incisor tooth 31
- 32. 2. Cleft of Palate (cleft of the embryologic secondary palate) A. Soft Palate (staphyloschisis or veloschisis) 1) Posteroanterior: one-third, two-thirds, complete 2) Width - maximum (mm) 3) Palatal shortness: none, slight, moderate, marked 4) Submucous cleft (a) Extent: one-third, two-thirds, complete 32
- 33. B. Hard Palate (uranoschisis) 1) Posteroanterior (a) Extent: one-third, two-thirds, complete 2) Width - maximum (mm) 3) Vomer attachment: right, left, absent 4) Submucous cleft (a) Extent: one-third, two-thirds, complete C. hard and soft palate (uranostaphyloschisis) 33
- 34. 3. Mandibular Process Clefts A. Lip (a) Extent: one-third, two-thirds, complete B. Mandible (a) Extent: one-third, two-thirds, complete C. Lip Pits: Congenital lip sinuses 4. Naso-ocular: Extending from the narial region toward the medial canthal region. 5. Oro-ocular: Extending from the angle of the mouth toward the palpebral fissure. A. Oro-medial canthus – from angle of mouth to medial angle of palpebral fissure. B. Oro-lateral canthus – from angle of mouth to lateral angle of palpebral fissure. May extend to temporal region. 6. Oro-aural: Extending from the angle of the mouth toward the auricle. 34
- 35. PFEIFER CLASSIFICATION (1964) • At the ‘2nd International Symposia on Cleft Lip and Palate’ in Hamburg in 1964 Pfeifer introduced a visual symbol to index a cleft malformation. • It is a pentagon that consists of a vertical block of three pairs of rectangles representing lip, alveolus, and hard palate standing on top of a triangle representing the soft palate. 35
- 36. DAHL’S CLASSIFICATION (1970) • Dahl divided the clefts in four groups: • Cleft Lip (CL), • Cleft palate (CP), • Unilateral CLP • Bilateral CLP 36
- 37. KERNAHAN STRIPPED ‘Y’ CLASSIFICATION (1971) • In 1971, Kernahan further modified Pfeifer’s classification into a striped Y symbolic classification. He has represented the most severe and extensive form of cleft lip with cleft palate deformity as a ‘Y’. • Each individual can be diagrammatically represented by stippling appropriate areas of clefting. In submucous cleft of palate the appropriate section is cross hatched. Simonart's band can be represented by cross hatching the anterior portion of the limb of the Y. • By assigning numbers to the striped Y segments, classification and retrieval of information can be achieved with ease. 37
- 38. Limitations of Kernahan’s Classification – 1. The degree of cleft is ambiguous 2. Premaxillary protrusion and alveolar arch collapse cannot be depicted. 3. The palate is not divided into its hard and soft portions for differential description in partial and complete clefts. 4. Function is not illustrated along with structure, so there is no indication of velopharyngeal incompetence. 5. The diagram lacks labelling for patient name, date and stage in the course of the treatment. 6. Inadequate detail for recording cleft lips, especially asymmetric deformities in bilateral cleft lip; 7. Inadequate detail for assessment of palatal deformities associated with speech results and rates of fistula formation 8. Potentially misread data that was hard to analyze by computer. 38
- 39. MODIFICATIONS OF KERNAHAN STRIPED ‘Y’ CLASSIFICATION 1. Elsahy Modification of Stripped ‘Y’ classification (1973) • Triangle 1, 5 – Nasal Cavity • Square 2, 6 – Upper Lip • Square 3, 7 – Alveolus • Square 4, 8 – Hard palate anterior to incisive foramen • Square 9, 10 – Hard Palate • Square 11 – Soft palate • Circle 12 – Posterior Pharynx • Circle 13 - Premaxilla 39
- 40. It has the following advantages over the original Striped Y. 1. It gives information about the degree of cleft lip. 2. It indicates the presence or absence of collapse of the alveolar arch. 3. It describes the state of the hard and soft palate as a separate identity. 4. It describes the position of the palatal segments in complete cleft palate. 5. It indicates the presence or absence of velopharyngeal closure, thus giving some idea of the patient's speech. 6. It indicates the absence or presence of a protruding premaxilla and the degree of the protrusion. 7. It facilitates comparison between different patients and different stages in the same patient (preoperative and postoperative). 40
- 41. 2. Milliard’s modification of Stripped ‘Y’ Classification (1977) • Millard endorsed Elsahy’s revision of Kernahan’s striped Y classification. • He further modified it by adding inverted triangles atop the upright triangular segments 1 and 5 to stand for the right and left aspects of the nasal arch respectively. • In his symbolic representation horizontal lines in these nose segments, of density proportionate to the degree of nasal deformity, can be used to mark it. • Horizontal lines can also be employed to show submucosal clefts. 41
- 42. 3. Friedman’s Modification of Stripped ‘Y’ Classification (1991) • Friedman proposed the modification which combines the graphic and striped schemes of Elsahy and Millard; further it incorporates various cleft microforms and assigns severity scores to the anatomic and functional deformities. • Instead of shading the blocks in the diagram to indicate the severity of the deformity a number is placed in each diagrammatic segment to represent. 42
- 43. 4. Smith’s Modification of Stripped ‘Y’ Classification (1998) • Smith modified the Kernahan Y classification further, in an attempt to make up for the shortcomings. The description of the cleft deformities became more detailed. • Incomplete cleft lip was denoted as letters ‘‘a’’ to ‘‘d’’ for minor defects to lips. • A similarly detailed description also was used to describe a secondary palatal deformity by subdividing it into three segments: palatine process of the maxillary bone, the palatine process of the palatine bone, and the soft palate. • The letter ‘‘a’’ denotes a sub-mucous cleft. • The Smith’s modification is more comprehensive than the Kernahan Y classification. 43
- 44. SPINA’S CLASSIFICATION Spina in 1974 proposed a modification of classification presented by the nomenclature committee of the American Cleft Palate association. The reference point for the proposed classification is the incisive foramen. Group I: Pre-incisive foramen clefts (clefts lying anterior to the incisive foramen), Clefts of the lip with or without an alveolar cleft: A. Unilateral B. Bilateral C. Median Group II: Trans-incisive foramen clefts (clefts of the lip, alveolus, and palate). A. Unilateral. B. Bilateral. Group III: Post-incisive foramen clefts Group IV: Rare Facial clefts 44
- 45. BALAKRISHNAN’S CLASSIFICATION • The original Indian classification and brief notation was published by Dr. (Prof) C. Balakrishnan in 1975 at Nagpur. • Using these groups and brief notations, he described 12 types of possible cleft deformities. • The Indian classification has anatomical and embryological basis. 45
- 46. 46
- 47. TESSIER’S CLASSIFICATION • In 1976, Tessier proposed a classification of craniofacial clefts that has been widely accepted. • Based on his personal experience, which included clinical, radiologic, and surgical observations of 336 patients, Tessier devised an ordered numbering system to identify the consistent anatomic pathways of soft tissue and skeletal clefts. • The appealing simplicity of the Tessier system has both improved communication between observers of craniofacial clefts and provided a better appreciation of the reconstructive surgery required to restore normality. 47
- 48. 48
- 49. 49
- 50. LAHSHAL CLASSIFICATION • A completely new recording-system for the diagnosis of cleft lip and palate malformations is the LAHSHAL system that Kriens introduced in Bremen in 1985. • He projects the first letter of the English terms for Lip, Alveolus, Hard, and Soft Palate in one line. • LAHSHAL is a palindrome representing the anatomic structures, proceeding from the patient's right side toward left side. 50
- 51. • In the LAHSHAL system, each column of the acronym is filled by a letter or symbol that confirms involvement of that part of the anatomy as well as the severity of the clefting: A capital letter means that anatomic feature was completely clefted; a lowercase letter means incomplete clefting; an asterisk (*) means minimal clefting (e.g., lesser-form cleft lip, notched alveolus, submucous cleft palate); and a period (.) or dot (•) means that anatomic feature is normally developed. 51
- 52. RPL SYSTEM • Using the Kernahan concept with modification Schwartz in 1993 developed a three-digit numerical system RPL system to record the location and number of anatomic components involved in cleft deformities. • The right limb of the Kernahan Y classification (1, 2, and 3) is represented by the first digit of this recording system (R). The base of the Y (7, 8, and 9) is represented by the second digit (P), and the left limb (4, 5, and 6) is identified by the third digit (L). Each digit is represented by the numerals 1 to 3, consistent with the anatomic components involved in an anteroposterior direction. • Any of the 63 cleft possibilities in the Kernahan classification can be represented by three digits only, allowing immediate identification and computerized data analysis. However, the RPL system is too simple to describe the incomplete and asymmetry of cleft deformities. 52
- 53. KOCH’S CLASSIFICATION • Koch and Koch in 1995 proposed a new extended classification, LAHSN of cleft deformities. In addition to the lip, alveolus, hard palate, soft palate, they also considered the Vomer and the micro forms in three dimensions. • The anatomical regions-lip, alveolus, hard and soft palate, and nose (LAHSN) can be affected single, or they can be affected in all combinations with each other. • The severity of all single and combined malformations of LAHSN depends on its extent in sagittal, transverse and vertical directions, and it depends on whether they are submucous or open forms. 53
- 54. The transverse direction In transverse direction the cleft malformation is very easy to localise and to record: left, or right sided, or a bilateral malformation of the lip, alveolus, hard palate and nose, and the medially located cleft malformation of the soft palate. The vertical direction In the vertical direction the two levels of the malformation- nose and vomer on the one hand, lip, alveolus, hard and soft palate on the other hand have to be considered. 54
- 55. The sagittal direction The sagittal extent (microform, subtotal or total) of the malformation of lip, alveolus, hard and soft palate is defined by adding the degree to the symbol representing the affected region (without regard to the shape). The classification is as follows: bilateral total cleft of LAHS L3 A3 H3 S3 H3 A3 L3 right total LAHS L3 A3 H3 S3 - left total cleft of lip -L3 bilateral total cleft of lip and alveolus L3 A3 A3 L3 bilateral total cleft of hard and soft palate -H3 S3 H3- Uvula bifida -Sl- 55
- 56. NEWER CLASSIFICATION • M.R. Ortiz-Posadas, L. Vega-Alvarado, J. Maya- Behar (2001), proposed a new method, which allows for a complete description of primary and secondary cleft palates, incorporating elements that are related to the palate, lip, and nose that will also reflect the complexity of this problem. • They developed a mathematical expression to characterize clefts of the primary palate, including the magnitude of palatal segment separation and the added complexity of bilateral clefts, yielding a numerical score that reflects overall complexity of the cleft. • Clefts of the secondary palate are also considered in a separate score. Using this method, it is possible to incorporate elements that are not considered in other approaches and to describe all possible clefts that may exist. 56
- 57. 57
- 58. 58
- 59. LAPAL CLASSIFICATION • The LAPAL system (2007) consists of only five Arabic numerals that describe accurate anatomic components and the extent of any cleft. It was proposed by Qiang Liu and his associates. • Numerals are ordered from the right side to the left side, corresponding to what one sees when facing a patient. • One numeral is used for the palate posterior to the incisive foramen for the following reasons: 1. Clefts in the posterior hard palate and soft palate are almost in the midline; 2. A bilateral cleft palate is not attached to the nasal septum; and 3. The soft palate has no relationship to the Vomer, although a unilateral cleft palate is fused with the nasal septum on one side. 59
- 60. The extent of cleft deformities (i.e., intact to complete cleft) is represented by Arabic numerals 0 to 4 in order to provide more detailed information, even though some minor clefts such as a minor degree of cleft alveolus, do not have a great bearing on management. 60
- 61. LIMA CLOCK DIAGRAM • Percy Rossell-Perry gave the Lima clock diagram in 2009, is the design of a new diagram for cleft lip and palate, based on the degree of severity of the four basic cleft components: nose, lip, primary palate, and secondary palate. • The clock diagram, is a circle divided into four areas, one for each cleft component. • Each area is subdivided into three segments, which represent the three degrees of severity- mild, moderate, and severe. 61
- 62. • He assigns the clock numbers (1 to 12) to each degree of severity of the four components as follows: • a) Right superior quadrant (nasal deformity). Degrees: Mild (1), Moderate (2), Severe (3). • b) Right inferior quadrant (medial segment lip and Prolabium deformity).Degrees: Mild (4), Moderate (5), Severe (6). • c) Left inferior quadrant (primary palate). Degrees: Mild (7), Moderate (8), Severe (9). • d) Left superior quadrant (secondary palate).Degrees: Mild (10), Moderate (11), Severe (12). 62
- 63. EPIDEMIOLOGY 63
- 64. PREVALENCE • The overall prevalence of Oro-Facial Cleft (OFC) is estimated to be approximately 1 in 700 live births, accounting for nearly one half of all craniofacial anomalies • The prevalence of OFCs varies from 1/500 to 1/2500 births depending on the geographic origin, racial and ethnic backgrounds, and socioeconomic status • Asians have the highest risk (14 : 10,000 births) followed by whites (10 : 10,000 births) and African Americans (4 : 10,000 births) • As reported by the World Health Organization (WHO), the prevalence at birth of OFC varies worldwide, ranging 3.4–22.9 per 10,000 births for CL/P, and 1.3–25.3 per 10,000 births for CPO. 64
- 65. • Prevalence has been found to vary based on ancestry, with the highest incidence rates observed amongst Asian populations (0.82–4.04 per 1000 live births), intermediate rates amongst Caucasians (0.9–2.69 per 1000 live births), and the lowest rates amongst African populations (0.18–1.67 per 1000 live births). • Overall incidence of cleft lip and palate is approximately 1 in 600 to 800 live births (1.42 in 1000) and isolated cleft palate occurs approximately in 1 in 2000 live births. Thus, the typical distribution of cleft types are: 1. Cleft lip alone – 15% 2. Cleft lip and palate – 45% 3. Isolated cleft palate – 40% 65
- 66. GENDER RATIO • Prevalence of OFC additionally varies according to gender and cleft pattern. Male predominance has been consistently identified in CLP, with a male/female sex ratio of 1.81. • For CP, the opposite has been shown, with a reported sex ratio of 0.93; however, this may be due in part to sampling bias, as one Danish study could not find a significant predominance of females in individuals with CP after combining both surgically treated and non-surgically treated cases 66
- 67. LATERALITY • OFC may be unilateral or bilateral. According to the International Perinatal Database of Typical Orofacial Clefts (IPDTOC) working group, the proportion of bilateral cases is 10.3% for cleft lip without palate (CL) and 30.2% for cleft lip with palate (CLP). • Amongst unilateral cases, 36.9% of CL and 41.1% of CLP occur on the right side, suggesting that unilateral cases of CL/P occur more frequently on the 67
- 68. 68
- 69. FACTORS INFLUENCING INCIDENCE • Sex – more common in males than females. • Race – American Indians and Afghans show higher incidence • Birth Weight – babies with isolated cleft palate have lower birth weight than those with isolated cleft lip • Parental Age – increasing incidence has been reported with increasing parental age (particularly mothers) • Birth Rank – incidence is more in first born child • Social Status – malnutrition increases the chances of cleft lip and cleft palate 69
- 70. ETIOLOGY 70
- 71. Various aetiologies of cleft lip and palate are – • Heredity (Genetic predisposition) • Nutritional disturbances during development • Physiologic, Emotional & Traumatic stresses during development • Defective vascular supply to the affected area • Mechanical disturbances (Tongue size may interfere) • Effect of certain drugs (Aminopterin, Cortison, Thalidomide, Anti-cancer drugs, etc) • Effect of alcohol • Radiation • Infection • Lack of inherent developmental force • Maternal smoking • Syndrome associated with cleft lip and palate 71
- 72. Heredity • Transmitted through a male as sex linked recessive gene. • Predisposition for cleft lip is 40% while only 18-20% for cleft palate. • Much evidence supports the view that genetic factors are associated with orofacial clefting • In twins with cleft lip-palate, concordance is far greater for monozygotic twins (40%) than dizygotic twins (4.2%) 72
- 73. Chromosomal rearrangements • Orofacial clefting is seen as part of the phenotype in a wide variety of rearrangements of many chromosomes, including trisomies, duplications, deletions, microdeletions, or cryptic rearrangements (Brewer et al., 1998, 1999). • Rearrangements that can include a CL/P are deletions of 4p (Wolf- Hirschorn syndrome), 4q or 5p (cri du chat syndrome); duplications of 3p, 10p, and 11p; and trisomy 13 or 18 (and trisomy 9 mosaic). • CP is seen with deletions of 4q and 7p; duplications of 3p, 7p, 7q, 8q, 9q, 10p, 11p, 14q, 17q, 19q; and trisomy 9 or 13. 73
- 74. • The role of microdeletions and other cryptic rearrangements in orofacial cleft etiology has recently been recognized. • Microdeletions of 22q11.2 are now known to be the common etiology for at least three clinically classified syndromes—DiGeorge syndrome, velocardiofacial syndrome, and conotruncal anomaly face syndrome— with an incidence of about 1 in 4000 , and cleft palate is seen in as many as 80% of cases, although this estimate is likely to be biased by the ascertainment of cases through cleft palate centers. • A microdeletion in this region has also been noted in 7 of 23 patients with velopharyngeal insufficiency (Zori et al., 1998). 74
- 75. Environment 75
- 76. Syndromes associated with clefts Following syndromes have been associated with clefts – 1. Autosomal dominant a. Van der Woude Syndrome b. EEC (Ectrodactyly, Ectodermal Dysplasia, Cleft) 2. Autosomal Recessive a. Meckel Syndrome b. Orofacial digital syndrome type II c. Roberts Syndrome 3. X – linked a. Orofacial digital syndrome type I b. Isolated cleft palate with ankyloglossia 4. Chromosomal a. Trisomy 13 b. Trisomy 18 5. Non Mendelian a. Pierre Robin Syndrome b. Clefting with congenital heart disease 76
- 77. Multifactorial Etiology • Recent studies show that etiology of cleft lip and palate cannot be attributed solely to either genetic or environmental factors. • It seems to involve more than one factor. • They argue that unless a person is genetically susceptible, the environment factors may not by themselves cause clefts. • Chances increases if more than one family member if affected • More the severity, greater the chances of recurrence in sibling • Higher risk if affected individual is of less affected sex • Risk decreases in remotely related individuals • Consanguinity increases the rate because of sharing of genes 77
- 79. DENTAL PROBLEMS • Tooth agenesis, hypodontia (most common), microdontia • Supernumerary teeth (2nd most common) • Enamel hypoplasia (CI) • Posterior & anterior crossbites • Ectopic eruption, transposition • Taurodontism, dilacerations • Congenitally missing teeth( mostly upper lateral incisors) at the site of cleft • Presence of supernumerary, neonatal and natal teeth • Peg shaped teeth • Ectopically erupted tooth • Fused teeth 79
- 80. SKELETAL PROBLEMS • Maxillary deficiency • Mandibular prognathism • Class III malocclusion • Concave profile • Constricted maxilla • Skeletal deep bite • Protruded premaxilla 80
- 81. ESTHETIC PROBLEMS • Facial disfigurement • Orofacial structures can be malformed and congenitally missing • Deformities of nose can also occur 81
- 82. HEARING AND SPEECH PROBLEMS • Children with cleft often have associated speech and language disorder. • Assessment of speech therapist is required as early as 9 months of age • Patient with delayed development of speech may have receptive language problems that arise because of the collection of fluid in middle ear. • Hearing loss may also occur due to ossicular malformation. • Speech problems are more severe if surgery is delayed • Usually an operated cleft palate patient present short palate, decreased mobility of soft palate due to scarring and presence of oronasal fistula, all which contribute to velopharyngeal insufficiency 82
- 83. FEEDING PROBLEMS • Oronasal fistulas • Draining of oral fluids in nasal cavity and vice versa • Bottle, cup and spoon, tube feeding • Nasal regurgitation • Infant held at 30-450 angle to aid swallowing 83
- 84. PSYCHOLOGICAL PROBLEMS • Disfigurement of face causes psychological stress to the family. • Psychological stress in the child due to their abnormal facial appearance and they have to put up with staring, curiosity, pity, etc. • Child may perform bad in academics due to hearing and speech problems. 84
- 85. DIAGNOSIS 85
- 86. • Cleft lip and/or palate may be diagnosed by prenatal ultrasound, which has become more common because refinements of this diagnostic tool provide images by which congenital and developmental anomalies may be detected more clearly. • The ability to make the diagnosis in utero gives the parents the opportunity to be prepared for the birth of their infant with a facial anomaly and to understand the surgical procedures available for repair of the facial cleft. • If the diagnosis of a cranio facial anomaly has not been identified prenatally, parents may experience an overwhelming disappointment and sense of guilt when the obstetrician or neonatologist informs them of their baby’s birth defect. 86
- 87. Prenatal Diagnosis • Ultrasonography is a non-invasive diagnostic tool now widely used as a routine component of prenatal care. • Ultrasonography serves to confirm foetal viability, determine gestational age, establish the number of foetuses and their growth, check placental location, and examine foetal anatomy to detect any malformations. 87
- 88. Ultrasound Technique • Robinson reported that the detection rate for foetal cleft lip is improved greatly when transabdominal sonography is performed at or after 20 weeks of gestation. • Transvaginal sonography, although not routinely used, has been reported to allow earlier visualization of the face and better image resolution, yielding high specificity and sensitivity of prenatal cleft lip detection • Babcock and McGahan described a systematic approach that allows for fast and thorough sonographic evaluation of the midface structures. 88
- 89. • Starting with the coronal plane, the soft tissues of the foetal nares and upper lip are examined for continuity. • Once a cleft is detected in the coronal view, anatomic assessment continues in the axial plane, evaluating the superficial skin margin of the upper lip, the underlying orbicularis oris muscle, and tooth-bearing alveolar ridge 89
- 90. • Colour Doppler ultra sonography has been used to visualize abnormal flow of amniotic fluid from the mouth to the nasal cavity, a finding that may suggest the presence of a palatal cleft. 90
- 91. Limitations Various factors may limit the sensitivity of diagnosing an orofacial cleft during ultrasound screening – • unfavorable position of the fetus • hand or umbilical cord overlying the face • maternal obesity • presence of a multiple gestation • oligohydramnios (reduced amniotic fluid) • parity (number of pregnancies) • prior abdominal surgery • the presence of additional fetal abnormalities) 91
- 92. Three-dimensional Ultrasonography • Three-dimensional ultrasound imaging is a new technology that presents views of the foetal face with greater clarity than the conventional two- dimensional imaging described previously. • Advantages include • Viewing of the face in a standard anatomic orientation • Manipulation of planer views without concern for foetal movement • Identification of exact location of planer images relative to the surface facial image • Easy interpretation of lifelike rendered 3D images by a nontrained observer. 92
- 93. Advantages of Prenatal Cleft Diagnosis 1. Psychological preparation of parents and caregivers to allow for realistic expectations at the time of delivery 2. Education of parents on the management of the cleft: presurgical neonatal orthopedics, plastic surgery for lip and palate closure, and alveolar bone grafting 3. Preparation for neonatal care and feeding 4. Opportunity to investigate for other structural or chromosomal abnormalities 5. Possibility for foetal surgery 93
- 94. Disadvantages of Prenatal Cleft Diagnosis 1. Parents and professionals report an emotional disturbance and high maternal anxiety after prenatal diagnosis of cleft lip/palate is disclosed. 2. As the sensitivity of ultrasound screening in the detection of facial clefts increases, the potential exists for an increased number of families choosing to terminate the pregnancy even in the absence of other malformations. 3. Factors such as perceived burden, expectation of recurrence, religious and cultural beliefs, professional advice, and gestational age at diagnosis are considered influential in the family’s decision to terminate pregnancy 94
- 95. MANAGEMENT OF CLEFT LIP & PALATE 95
- 96. 96 MULTIDISCIPLINARY TEAM FOR CLEFT MANAGEMENT
- 97. Primary team or Core team • The CLEFT SURGEON undertakes the primary and the secondary repair. • The SPEECH THERAPIST monitors speech from 9 months onwards and institutes measures for normal development of speech. • The AUDIOLOGIST quantifies and locates the cause of hearing problem. • The ORTHODONTIST monitors the dental development, occlusion, skeletal problems and institutes interceptive therapy, dentofacial orthopaedics and prepares for secondary alveolar bone grafts. • Orthodontist’s expertise in cephalometry and craniofacial growth uniquely qualifies him/her to monitor craniofacial growth, dental development and treatment results. • The ORAL & MAXILLOFACIAL SURGEON assists in secondary bone grafting and orthognathic surgery if required. • The PLASTIC SURGEON corrects nose deformity, secondary deformities of lip and scar revision. 97
- 98. Supplemental Specialists • A SPECIALIST CLEFT NURSE who can monitor the neonates during the early days after birth and give feeding advice. • CLINICAL GENETICIST to resolve the genetic basis of the cleft and advice on recurrence risk. • PEDIATRIC DENTIST/PEDODONTIST to maintain and monitor dental health and oral hygiene. • ENT SURGEON/AUDIOLOGIST to take care of recurrent ear infections, insert grommets and hearing tests. 98
- 99. TREATMENT SEQUENCE TREATMENT TREATMENT TIMING PROCEDUE Pre – Surgical Orthopaedics 1 – 4 weeks Repositioning of palatal segments facilitates lip repair Lip Closure 8 – 12 weeks May be preceded by preliminary lip adhesion as an alternative to presurgical orthopaedics Palate Closure 18 – 24 weeks Closing only the soft palate initially an alternative, but one stage closure of the hard and soft palate is the usual procedure Speech Therapy 6 – 11 years Articulation errors often develop as child tries to compensate for cleft Early Orthodontics 7 – 8 years Usually incisor alignment and maxillary transverse expansion 99
- 100. Alveolar grafting 6 – 10 years Needed before permanent canines erupt; timing determined by stage and sequence of dental development. Comprehensive Orthodontics 11 – 14 years Class III elastics often vey helpful Pharyngeal flap surgery 9 – 19 years Only if required to overcome nasal air leakage during speech sometimes needed after loss of lymphoid tissue in the nasopharynx at adolescence or following maxillary advancement Orthodontic Surgery 17 – 19 years Maxillary advancement, perhaps combined with mandibular setback; not done until growth completed except in rare instances of severe psychological impact; needed infrequently Fixed Prosthodontics 17 – 19 years Replacement of missing lateral incisors; comprehensive treatment only after growth completed 100
- 101. 101
- 102. Feeding appliance • Feeding in a normal child involves two mechanisms – suckling and swallowing. • In cleft patients, due to abnormal musculature attachment, there is an inability to create negative intraoral pressure and hence the suckling mechanism is disturbed while swallowing is normal. • The feeding appliance or the obturator is intended to block the continuity of the oral cavity with the nasal cavity. • It facilitates feeding and reduces the time span required for feeding, prevents nasal regurgitation, and incidence of choking. • It also prevents abnormal positioning of the tongue in the cleft palate and therefore prevents widening of the cleft, assists in speech development, provides maxillary cross arch stability and prevents arch collapse after surgical closure of the lip. 102
- 103. 103
- 104. Presurgical Orthopaedics • It was pioneered and introduced by McNeil in 1950s. • He advocated that the neonatal maxillary orthopaedic could modify and control the postnatal development of maxilla by stimulating the growth of soft tissues overlying the hard palate. • The original philosophy of McNeil was to reduce the displacement of the alveolar segments and create a butt joint between the alveolar segments in the cleft region. • The idea was to create a normal arch form by actively moulding the alveolar segments using a series of plates. 104
- 105. Latham Appliance • Georgiade and Latham in 1975 introduced a pin- retained active appliance to retract the premaxilla and expand the posterior segments simultaneously. • The appliance mechanically manipulates the maxillary segments into close proximation. Along with lip adhesion, the gingivoperioplasty provides stabilisation of maxillary segments and reconstruction of nasal floor. • Advantage – include a fixed appliance which provides quick results in 2.5-3 weeks. • Disadvantage – this requires an additional surgery for its placement removal under general anesthesia. 105 a a aa b b
- 106. Presurgical Nasoalveolar Moulding (PNAM) • Conventional approaches and appliances for presurgical orthopaedics in cleft children focussed on correcting the alveolar cleft. • In 1993, Grayson et al described a technique to correct alveolus, lip and nose simultaneously. • The PNAM appliance is a palatal plate that is constructed on an infant’s maxillary cast. The device consists of an acrylic bulb (nasal stent) attached with a rigid wire. • The bulb/stent is left in the nasal dome and moulds the shape of the nostril and soft tissue of the cleft region. • Typically, PNAM is initiated within the 1st week after birth and needs to be modified and activated on a weekly basis. 106
- 107. • Alveolar moulding is done via active moulding and passive growth guidance. • Active moulding is done by over build-up of the soft acrylic on the labial flange and at the same time removal of the hard acrylic on the lingual side allowing the movement of the larger segment into the desired space and reverse is done for lateral or smaller segments. • Passive growth guidance of the alveolar segment growth on the medial aspect along the labial flange so that alveolus grows inside the cleft space and fills it. • The appliance is used for 4-6 months and alveolar moulding is finished before primary closure of lip. • Nonsurgical columella lengthening is done by a tape adhered to the prolabium and stretching downwards to engage the retention arm with elastics. The vertical pull provides a counter stretch to the upward force applied to the nasal tip of the nasal stent and helps to lengthen the columella and small prolabium. 107
- 108. Advantages of PNAM 1.Ability to guide the alveolar segments to a more normal position prior to surgery. 2.Reduction of the cleft gap facilitates the primary gingivoperiosteal closure of the cleft defect, because there is a greater probability that a complete osseous bridge formation will happen when cleft width is reduced. 3.The combined action of the nasoalveolar moulding plate and non surgical lip approximation with surgical taping results in a predictable correction of the nasal, alveolar and soft tissue deformities. 4.As a result under surgical repair the lip and nose heals under minimal tension with no or minimal scar formation. 108
- 109. Disadvantages of PNAM 1. irritation of oral mucosa or gingival tissue 2. Ulceration of intraoral tissues 3. The intranasal lining of the nasal tip can become inflamed 4. Skin irritation due to tape usage 5. Parent compliance is required 6. PNAM plate may get dislodged and obstruct the airway 109
- 110. CLEFT LIP REPAIR • The repair or the management of the cleft lips is known as CHEILOPLASTY. • The goal of this surgery is to address the functional and cosmetic deformity of cleft lip. • In order to achieve such goal, the repair should include the creation of an intact and appropriately sized upper lip to compensate for the loss of philtral height on the cleft side, repair of the underlying muscular structure for normal oral competence and function, and primary repair of nasal deformity. 110
- 111. Timing of surgery • Most surgeons repair the cleft lip taking into account the “Milliard’s Rule of 10”. 1. Age should be more than 10 weeks 2. Weight over 10 lbs, 3. Haemoglobin 10 g/dL 4. White blood cell count < 10,000/mm3 111
- 112. Various methods of Cleft Lip Repair • There are many techniques for the cleft lip repair. Some of them are- Milliard’s rotational advancement technique (1952) Tennison’s Stencil Method (1955) Skoog’s Method of Cleft lip repair (1958) Rendall’s Method (1959) Mulliken’s Method (1985) Mohler’s Technique (1987) Noordhoff’s Technique (1995) Afroze incision for Chelioplasty (2009) 112
- 113. Miiliard’s Rotational Advancement Technique (1952) 113
- 114. Tennison’s Stencil Method of Lip Repair (1955) 114
- 115. Skoog’s Method of Lip Repair (1958) 115
- 116. Rendall’s method of Lip Repair (1959) 116
- 118. 118
- 121. Afroze incision for cheiloplasty (2009) 121
- 122. CLEFT PALATE REPAIR • The surgical procedure to carry out the closure of the defect in the palate is known as PALATOPLASTY. • There is controversy related to the optimal timing of cleft palate repair, with varying recommendations, depending on which outcome is being considered. • Goals of palatoplasty include the separation of the nasal cavity from the oral cavity, creation of a competent velopharyngeal valve for both speech and swallowing, and preservation of midface growth. • For optimal speech development, recommendations for palatoplasty are as early as 3 to 6 months but at least before 12 months, when language acquisition begins 122
- 123. Various methods of Cleft Palate Repair There are many techniques for the cleft palate repair. Some of them are- von Langenbeck’s bipedicle flap technique Veau-Wardill-Kilner Pushback technique Bardach’s two-flap technique Furlow Double opposing Z-Plasty Two-stage palatoplasty Intravelar Veloplasty 123
- 124. von Langenback Bipedicle Flap Technique (1861) 124
- 125. Veau – Wardill – Kilner Pushback Palatoplasty 125
- 127. Furlow double opposing Z - plasty 127
- 128. Two – stage Palatoplasty • It is a well established fact that unrepaired cleft patients have better maxillary relationship and development. • Early palatal surgical intervention causes maxillary hypoplasia. Because of this reason many surgeons used to perform palate repair in two stages. • The soft palate was repaired early and later the hard palate was repaired. • At the time of introduction of this protocol the soft palate was repaired along with the lip at around four to six months of age and the hard palate was repaired at the age of 10-12 years. This was later reduced to four to five years. This delay significantly reduced the cleft width in the hard palate region and was easy to close without the need for extensive dissection. This reduced the maxillary hypoplasia significantly. However, the speech result was compromised. Hence this technique fell into disrepute. 128
- 129. Intravelar veloplasty • In 1968, Braithwaite first described the dissection of the Levator Palati from the posterior border of the hard palate, nasal and oral mucosa and posterior repositioning. • He described independent suturing of the muscle with that of the opposite side for the reconstruction of the Levator sling. • Since then intravelar veloplasty has evolved considerably and many surgeons have modified the surgical details to achieve better anatomical muscle sling reconstruction. 129
- 130. 130
- 131. Complications of Cleft palate repair Immediate complications • Haemorrhage • Respiratory obstruction • Hanging Palate • Dehiscence of the repair • Oronasal fistula formation Late complications • Bifid uvula • Velopharyngeal Incompetence • Abnormal speech • Maxillary hypoplasia • Dental malpositioning and malalignment • Otitis media 131 Common complications of any palate surgery are as follows:
- 132. Role of Orthodontist in Cleft Lip & Palate patients 132
- 133. Orthodontic – Orthopaedic treatment in deciduous dentition Problems in deciduous dentition: • Delay in eruption in vicinity of cleft • Malformed or congenitally missing lateral incisor • Anterior or posterior buccal crossbite • Functional shift • Turvey (1982) believe that orthodontic treatment in the deciduous dentition, although possible, is contraindicated • Rygh and Tindlund (1988) – Growth modification at this stage has been proposed. They recommend utilization of a quad-helix appliance soldered to bands on the primary second molar teeth and canines to expand the upper arch 133
- 134. Procedures carried out during this phase: • Adjustment of intraoral obturator to accommodate the erupting deciduous teeth. • To maintain a check on eruption pattern and timing. • Oral hygiene instructions. • Restoration of decayed teeth. • Orthodontic treatment is not normally recommended for primary dentition as it may damage permanent dentition follicles. • However , in patients with moderately underdeveloped maxilla and no class III hereditary defect reverse headgear treatment should be advocated at age of 4 – 7 years. 134
- 135. • Parents should understand the value of tooth brushing. • Parents may be nervous to brush in region of cleft especially following primary lip and palate surgery. • They should be shown in detail about how to brush. • A low fluoride children toothpaste containing no more than 600 ppm fluoride is recommended for children under 6 years. • Twice brushing daily is recommended. • In addition, twice yearly professional application of topical fluoride varnish is useful. 135
- 136. Orthodontic treatment during Mixed Dentition • The decision to intervene orthodontically during the mixed dentition stage of development depends on a careful assessment of the problems present and the potential risks and benefits. • Such treatment is not offered routinely to all cleft palate patients but it has been more common since the advent of the alveolar bone grafting procedure. 136
- 137. • Patient evaluation includes an appraisal of the soft tissue condition (ie, presence or absence of oronasal communication) the skeletal aspects of malocclusion in all three planes of space dental problems, o missing/malformed teeth, o malposed/rotated incisors, o anterior and/or posterior crossbites. • Timing of treatment is closely related to the age that the secondary alveolar grafting procedure is performed. 137
- 138. Procedures carried out in mixed dentition phase – • A tentative decision on extraction of supernumerary teeth and overretained teeth • Correction of crossbites (use of various expander appliances) • Maintain space for proper eruption of teeth • Expand collapsed segment to improve surgical excess to graft site. • Correction of jaw relationship (Face mask therapy) 138
- 139. Prior to Alveolar Bone Grafting – • As previously mentioned, individuals with CLP typically present with transverse maxillary deficiency and posterior crossbites. • The primary objective of orthodontic treatment during this mixed dentition phase is to prepare the maxillary segments for receiving the ABG, thus maxillary expansion is typically required. • Different type of appliances can be used to achieve this goal and the type of appliance used is directly dependent on the maxillary arch form, clinical presentation of the crossbite and on the orthodontist’s preference and personal experience. 139
- 140. Maxillary Expansion Devices – • Telescopic maxillary expander • Fan shaped maxillary expander • Butterfly maxillary expander • Spring jet for slow expansion • Banded / bonded rapid palatal expansion • Modified hyrax appliance • Quad helix 140
- 141. 141
- 142. 142
- 143. 143
- 144. 144
- 145. 145
- 146. 146
- 147. Bone Grafting • von Eiselsberg (1901) and Lexer (1908) were the first to use autogenous bone to graft the cleft maxilla by a free bone or pedicled soft tissue and bone of the little finger. • Drachter (1914) was the first to report the closure of a cleft with tibial bone and periosteum. Primary Bone Grafting • Primary and early secondary bone grafting were practised mainly in the 1950s and 1960s by a whole generation of cleft surgeons. • The indication for primary bone grafting was- elimination of bone deficiency, stabilization of the pre-maxilla, creation of new bone matrix for eruption of teeth in the cleft area and augmentation of the alar base. • There were also expectations of normalization or even stimulation of maxillary growth. 147
- 148. Secondary Bone Grafting • Secondary bone grafting, meaning bone grafting in the mixed dentition, became an established procedure after abandoning primary bone grafting. • The pre-requisites were precise timing, operating technique, and sufficiently vascularized soft tissue. The advantages of primary bone grafting allowing tooth eruption through the grafted bone could also be maintained. • Furthermore, secondary bone grafting can stabilize the dental maxillary arch, improving the conditions for prosthodontic treatment such as crowns, bridges and implants. • It will also facilitate eruption of teeth increasing the amount of bony tissue on the alveolar crest allowing orthodontic treatment. • Bony support to teeth neighbouring the cleft is a pre-requisite for orthodontic closure of the teeth in the cleft region. • Secondary bone grafting can also be used to augment the alar base of the nose to achieve symmetry with the non-cleft side, thereby improving facial appearance. 148
- 149. Face Mask Therapy • Used in maxillary deficient cleft patients • Orthopaedic forces are used in maxillary protraction • Orthopaedic forces are 350-500 gm per side over 10-12 hrs/day for an average of 12-15 months • Can be done before bone grafting in mild midfacial deficiency 149
- 150. Permanent Dentition Treatment • When the patient reaches the final stage in the development of his/her dentition, a thorough evaluation including complete orthodontic records is required. • Orthodontic appliances may still be present from the previous treatment phase or orthodontic retainers may be in place. • The outcome of this comprehensive evaluation should indicate whether the patient requires comprehensive orthodontics alone or orthodontics in conjunction with orthognathic surgery. • Although the percentage of cleft palate patients requiring orthognathic surgery is higher than that of the general population, the percentage per se is smaller than anticipated. 150
- 151. Skeletal Problems • In general, a patient with an oral cleft may show a wide spectrum of orthodontic problems with the cleft palate-related anomalies superimposed on them. • It is common that the maxilla exhibits deficiency in all three dimensions, i.e., anteroposteriorly, transversely, and vertically. Dental Problems 1. Absence of teeth adjacent to the cleft, most often the permanent lateral incisors 2. High incidence of missing teeth in other regions, especially missing bicuspids 3. Malformed teeth 4. Supernumerary teeth 5. Ectopically positioned teeth 6. Lack of osseous support for some teeth compromising the possibility to move these teeth to desired positions 7. Accentuated curve of Spee in the maxilla, the mandible, or both 8. Collapsed arch form 9. Poor oral hygiene, caries, periodontal disease. 151
- 152. Treatment by Orthodontics Alone • In the absence of severe skeletal discrepancy and major esthetic concerns, orthodontic treatment alone may be sufficient. Goals of such treatment include: • Tooth alignment • Establishment of a continuous maxillary arch with favorable arch form • Correction of anterior and/or posterior crossbites • Stability of occlusion in the presence of dental compensations • Favourable dentofacial esthetics • Missing teeth 152
- 153. Treatment by Orthodontics combined with Orthognathic Surgery • Severe skeletal discrepancy, oronasal fistulas, speech deformity • Maxillary surgery – multiple segment Le Fort I osteotomy with down grafting • Presurgical orthodontic treatment – 12 months • AP discrepancy – more than 8mm – bijaw surgery needs to be planned 153
- 154. 154 Surgeries for correction of UCLP • Standard Le Fort I osteotomy • Modified Le Fort I osteotomy (two segments) Surgeries for correction of BCLP • Standard Le Fort I osteotomy • Modified Le Fort I osteotomy (two segments) • Modified Le Fort I osteotomy (three segments)
- 155. Complications of Surgery • Airway Problems • Speech Impediment • Infection • Oronasal Fistula • Nerve Damage 155
- 156. Distraction osteogenesis • Ross (1987) showed that about 25% of patients with unilateral cleft lip and palate develop maxillary hypoplasia that does not respond to orthodontic treatment alone. • The hypoplastic maxilla is usually advanced later by Le Fort I osteotomy, with or without bone grafting, to re-establish facial balance and occlusion. • However, the maxilla in these patients is often difficult to mobilize because of scarring from previous operations. In spite of improvements in surgical fixation, cleft patients have a greater tendency to relapse than do noncleft patients with maxillary hypoplasia that may adversely affect final surgical results. • Distraction osteogenesis is an effective method used for bone regeneration. 156
- 157. Distraction Osteogenesis is a procedure that moves two segments of bone slowly in such a way that new bone fills the gap. • In this procedure, a surgeon makes an osteotomy cuts in the bone and attaches a device known as distractor to both sides of osteotomy. • The distractor is gradually adjusted over a period of days or week to stretch the osteotomy so that new tissue fills in it. 157
- 158. External Distractors Advantages – • Direction of force is well controlled Disadvantages – • Cranial surgery is performed • Esthetics are compromised 158
- 159. Internal Distractors Advantages – • Esthetic • Psychological Relief Disadvantages – • Difficult to control the direction of force 159
- 160. CONCLUSION 160
- 161. • The key to successful rehabilitation of cleft lip and palate include flexibility and a interdisciplinary approach. • Patient should be treated with sympathy and concern. • Parents should not panic with the condition, rather should provide special attention to such child . • There is no perfect method of treating a cleft patient; patient and his individual treatment needs must be taken into account. • Treatment begins soon after birth and continues till adulthood requiring a team approach. • Decision should be made along with other team members who all are responsible for well being of the patient from infancy to adulthood. 161
- 162. REFERNCES 162
- 163. 1. Contemporary Orthodontics – Proffitt, 5th edition 2. Orthodontics – Current Principles and Techniques – Graber, Vanarsdall, 5th edition 3. Orthodontics – Diagnosis and management of Malocclusion and Dentofacial Deformities – O. P. Kharbanda, 3rd edition 4. Cleft lip and palate – diagnosis and management – Berkowitz 5. Milliard D. A Radical rotation of single hairlip. Am J Surg. 1958:95; 318-22. 6. Skoog T. A Design for the Repair of Unilateral Cleft Lips. Am J Surg. 1958:95; 223-6. 7. Tennison CW. The repair of the unilateral cleft lip by stencil method. Annual meeting of American society of Plastic and Reconstructive Surgery 8. Reddy GS. Afroze Incision for Functional Cheiloseptoplasty. J Craniof Surg 2009;20(2): 1733-6. 163
- 164. 9. Mulliken JB et al. Principles and Technique of Bilateral Complete Cleft Lip Repair. Plast Reconst Surg 1985;75(4):477-86. 10. Mohler LR. Unilateral cleft Lip Repair. J Plast Reconst Surg 1987;80(4):511-6. 11. Noordhoff MS et al. The Surgical Technique For The Complete Unilateral Cleft Lip-nasal Deformity. Op Tech Plast Reconstr Surg1995;2(3):167-174. 12. Randall P. A Triangular Flap operation for the primary repair of unilateral clefts of lip. Plast Reconst Surg 1959;23(4):331-47. 13. Marcus JR et al. Principles of Cleft Lip Repair: Conventions, Commonalities, and Controversies. Plast. Reconstr. Surg. 2017;139(3):764e-80e. 14. Agrawal K. Cleft palate repair and variations. Indian J Plast Surg 2009;42(Suppl 1):S102-9. 15. Shkoukani MA et al. Cleft palate: A Clinical Review. Bir Def Res 2014;102:333–42. 164
- 165. 16. Allam E et al. Cleft Lip and Palate: Etiology, Epidemiology, Preventive and Intervention Strategies. ANAT Physiol 2014;4(3). 17. Georgiade NG, Latham RA. Maxillary Arch alignment in the bilateral cleft lip and palate infant, using the pinned coaxial screw appliance. Plast. Reconstr. Surg. 1975;56(1):52-60. 18. Lilja J. Alveolar bone grafting. Indian J Plast Surg 2009;42(Suppl 1):S110-5. 19. Vlachos CC. Orthodontic treatment for cleft palate patient. Semin Orthod1996;2(3):197-204. 20. Rachmeil A. Treatment of Maxillary Cleft Palate: Distraction Osteogenesis Versus Orthognathic Surgery—Part One: Maxillary Distraction. J Oral Maxillofac Surg 2007;65:753-757. 21. Posnick JC. Orthognathic Surgery for the Cleft Lip and Palate Patient. Semin Orthod 1996;2:205-214. 22. Shaw WC. Orthodontic Treatment of Malocclusion Associated with Repaired Complete Clefts of the Lip and Palate. Brit J Orthod 1979;6:73-83. 165
- 166. 166THANK YOU FOR YOUR PATIENT HEARING