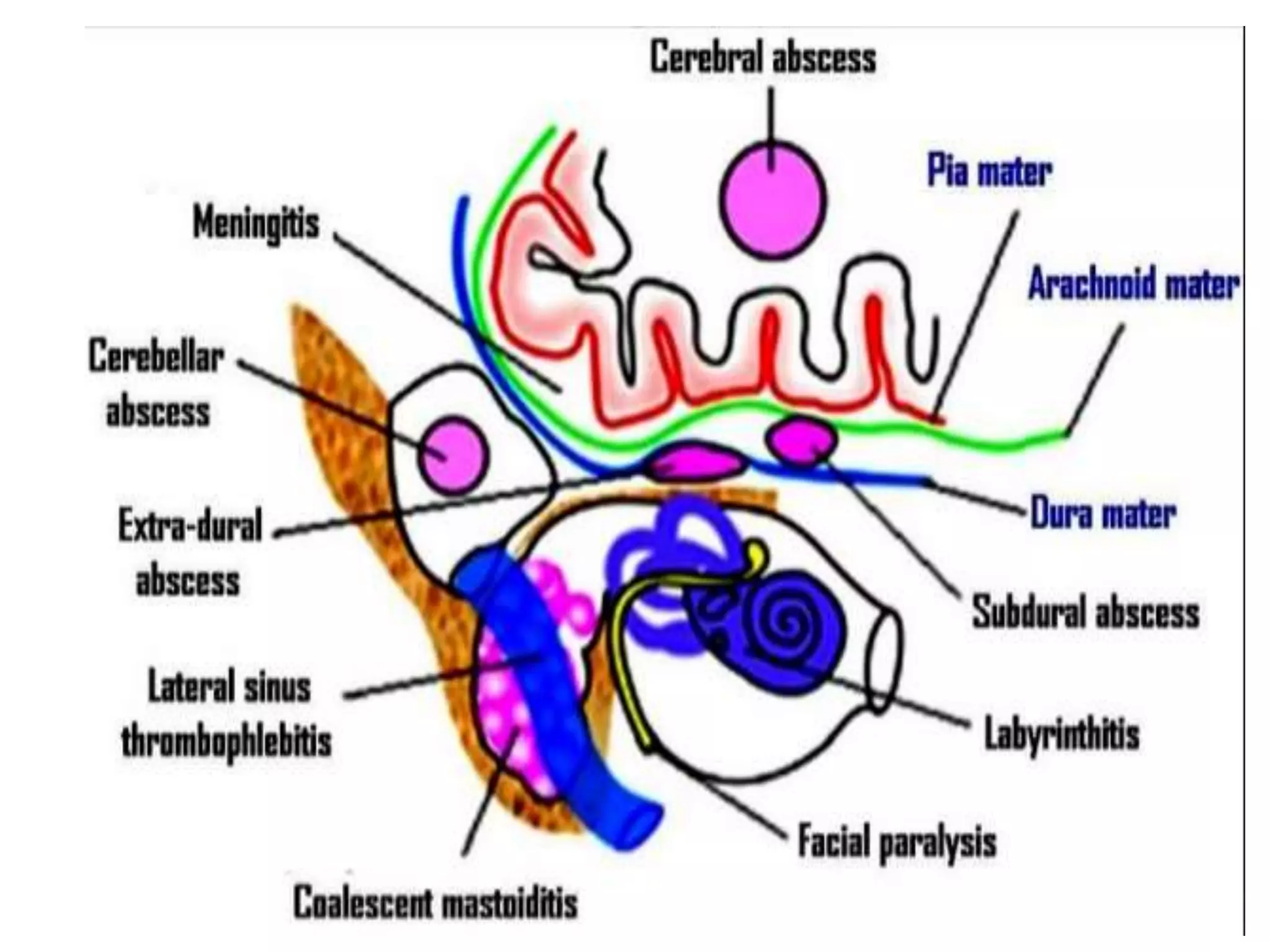
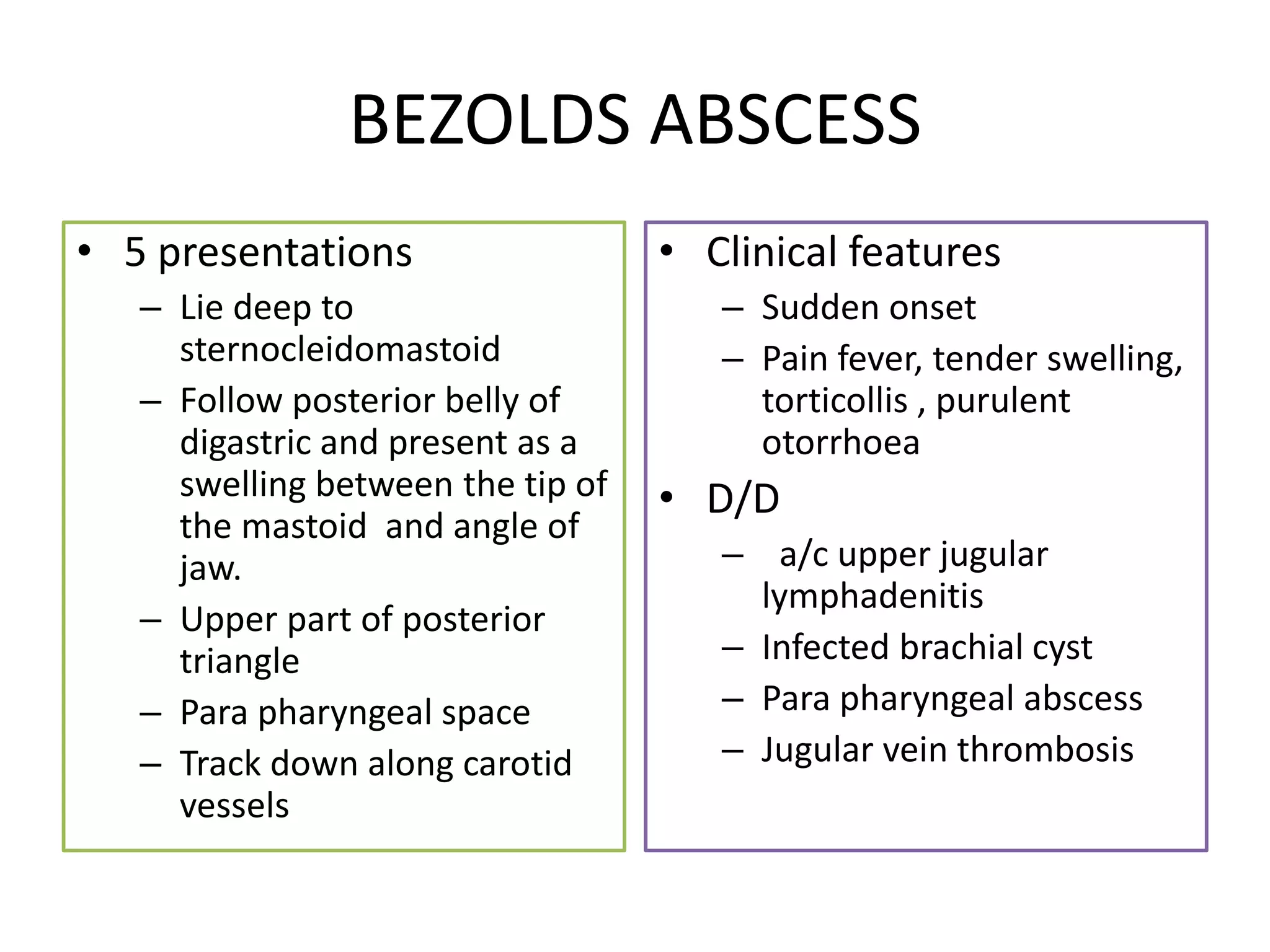
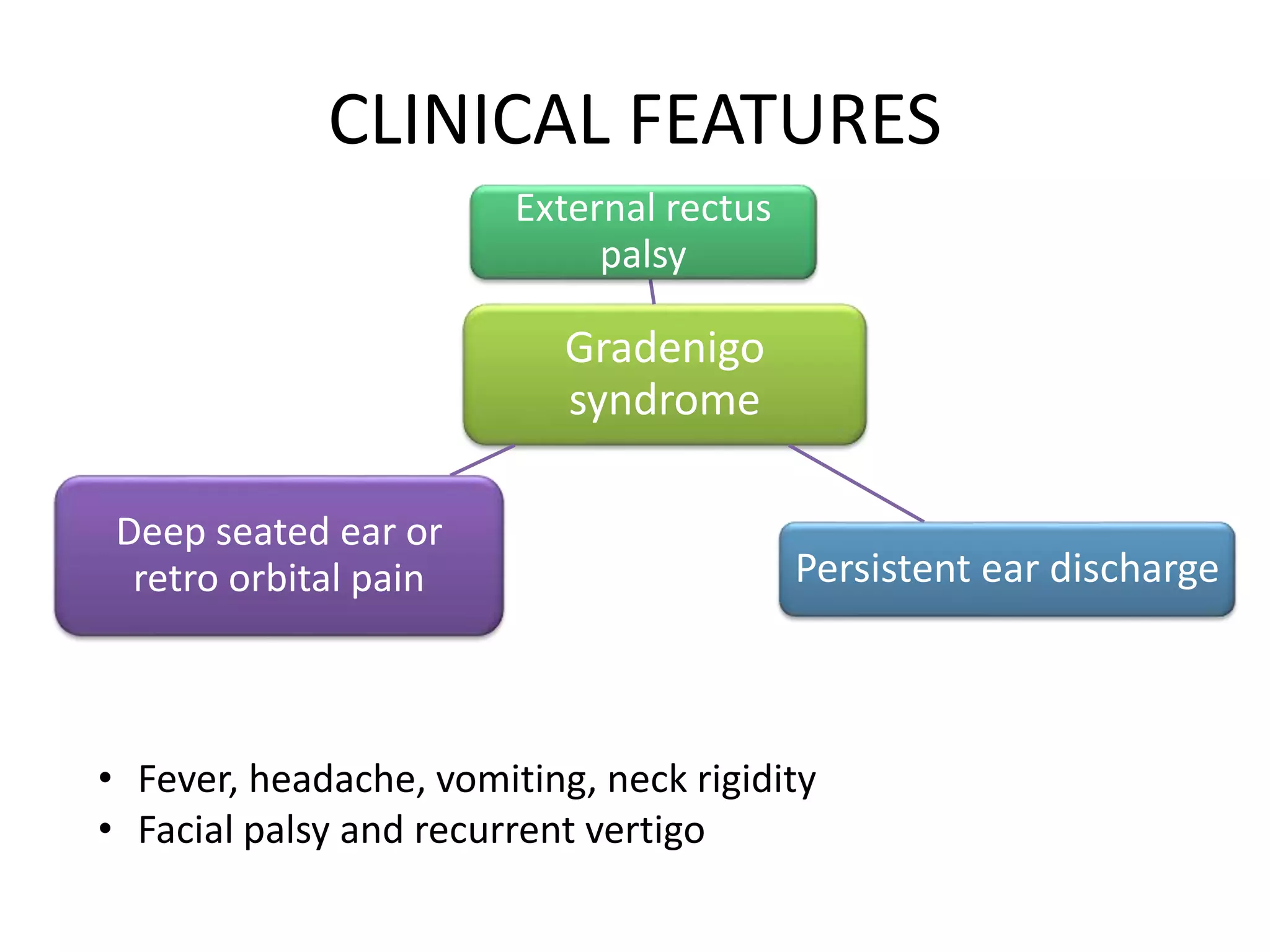
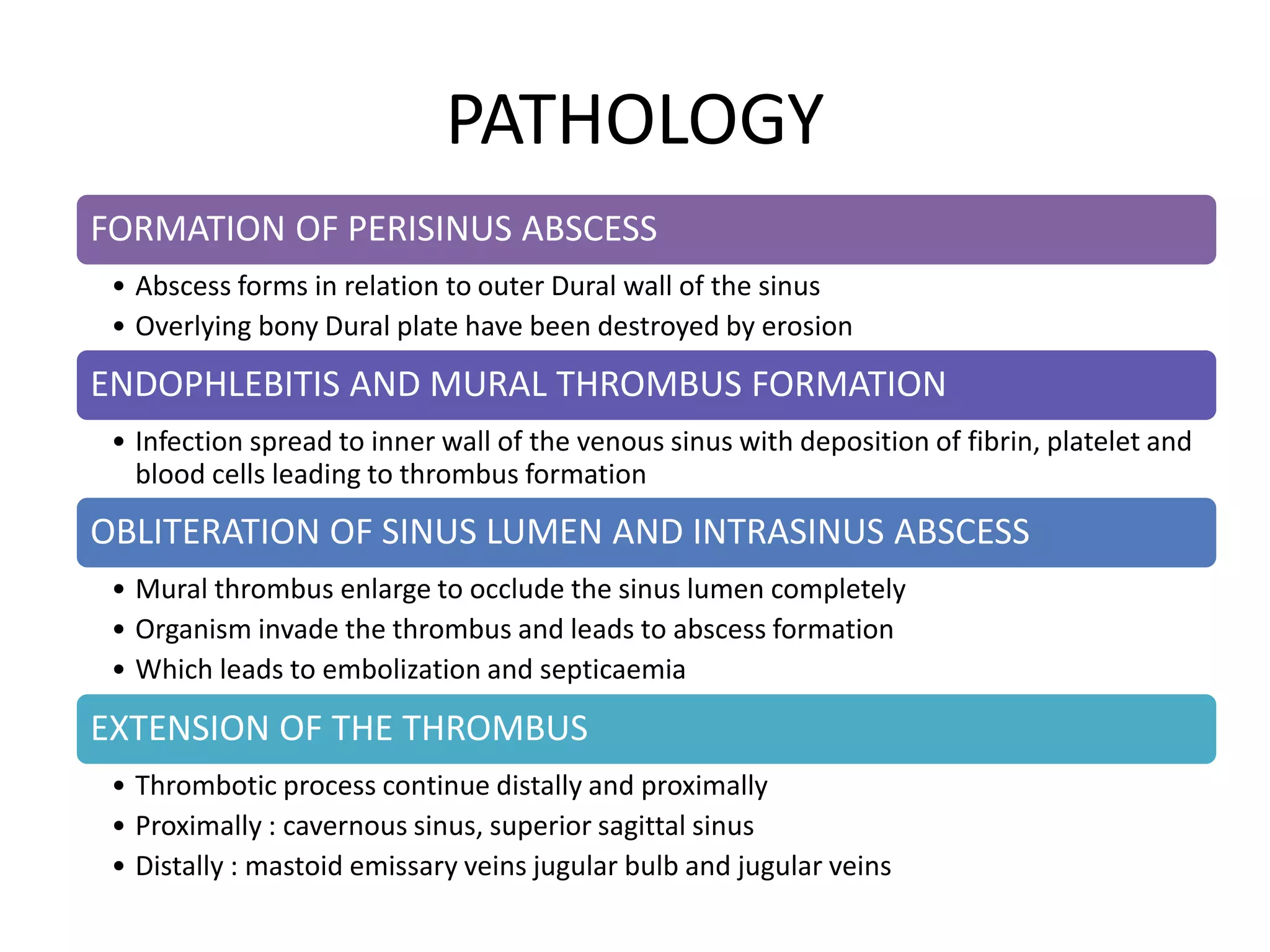
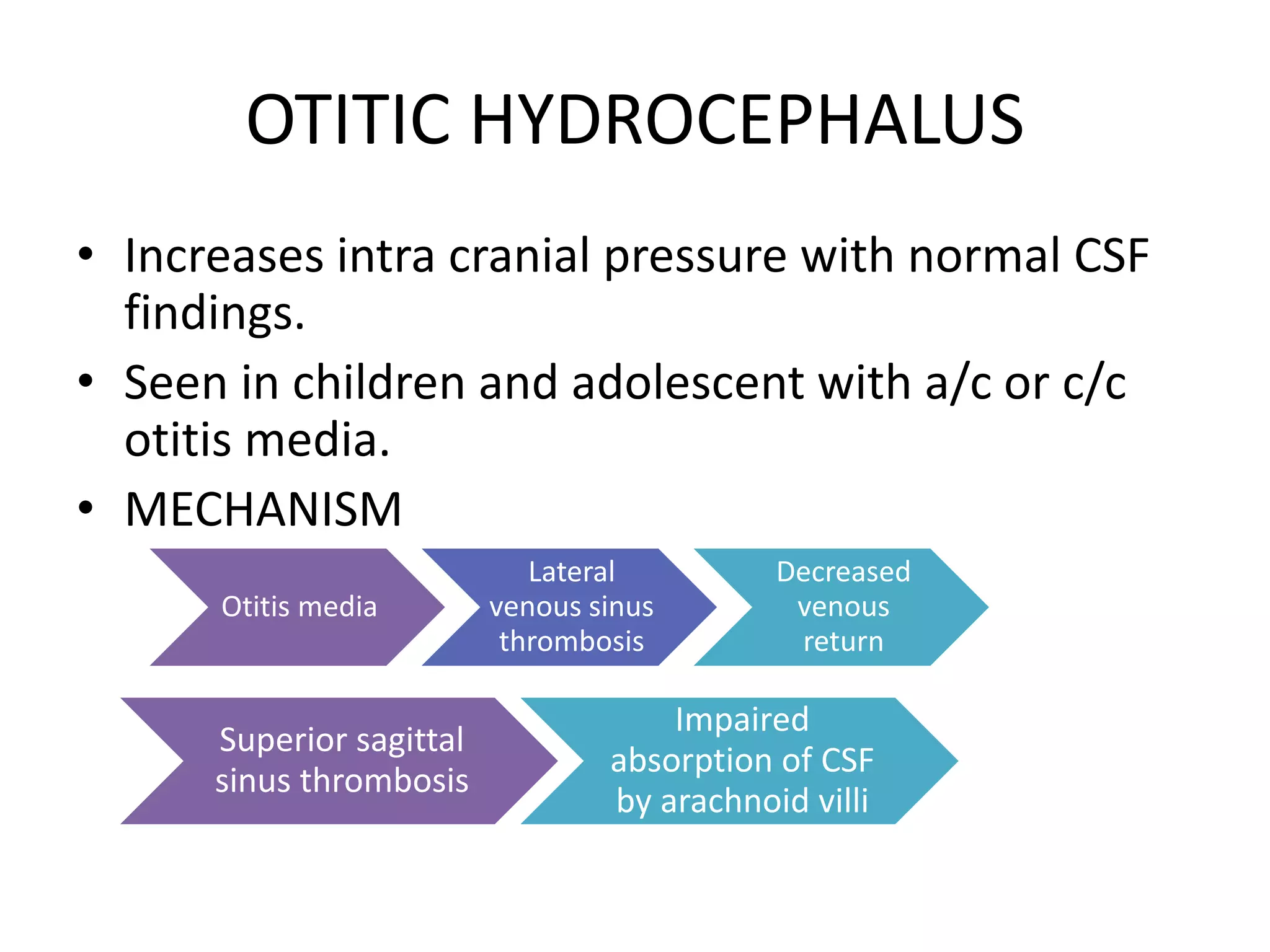
This document summarizes various complications that can arise from otitis media. It discusses both extracranial complications like mastoiditis, mastoid abscesses, and facial nerve palsy, as well as intracranial complications like labyrinthitis, meningitis, brain abscesses, and lateral sinus thrombophlebitis. It provides details on the pathology, clinical features, investigations, differential diagnosis, and management of each complication.