A female patient with intra operative pulmonary edema and bilateral spontaneous pneumothorax
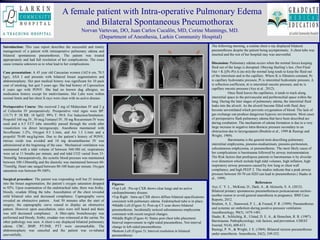
- 1. Figures: •Top Left : Pre-op CXR shows clear lungs and no active cardiopulmonary disease. •Top Right : Intra-op CXR shows diffuse bilateral opacifications consistent with pulmonary edema. Endotracheal tube is in place. •Middle Left (Figure 3): Post-op CT scan shows bilateral pneumothorax. Incidentally noticed subcutaneous emphysema consistent with recent surgical changes. •Middle Right (Figure 4): Status post chest tube placement. Interval improvement in right-sided pneumothrax. Not interval change in left-sided pneumothorax. •Bottom Left (Figure 5): Interval resolution in bilateral pneumothorax Introduction: This case report describes the successful and timely management of a patient with intraoperative pulmonary edema and bilateral spontaneous pneumothorax. The patient was treated appropriately and had full resolution of her complications. The exact cause remains unknown as to what lead to her complications. Case presentation: A 45 year old Caucasian women (162.6 cm, 70.5 kgs), ASA I and presents with bilateral breast augmentation and abdominoplasty. Her past medical history was significant for 10 pack year of smoking, but quit 5 years ago. She had history of Liposuction 6 years ago with PONV. She had no known dug allergies, no medication history except for multivitamins. Her Labs were within normal limits and her chest X-rays were clear with no active disease. Perioperative Course: She received 2 mg of Midazolam IV and 2 g of Cefazolin IV preoperatively. Preoperative vital signs were BP: 131/71 P: 58 RR: 18 SpO2: 99% T: 99.0. For Induction/Intubation: Propofol 160 mg IV, 50 mcg Fentanyl IV, 50 mg Rocuronium IV were used and a 6.5 ETT tube smoothly passed through the cords after visualiztion via direct laryngoscopy. Anesthesia maintained with Sevoflurane 1-2%, Oxygen 0.5 L/min, and Air 1.5 L/min and a propofol 70-80 mcg/kg/min. Due to the patient’s history of PONV, nitrous oxide was avoided and 10 mg dexamethasone IV was administered at the beginning of the case. Mechanical ventilation was maintained with a tidal volume of between 560-580 ml, respirations were set at 11 breaths per minute, and end tidal CO2 varied from 33- 36mmHg. Intraoperatively, the systolic blood pressure was maintained between 100-130mmHg and the diastolic was maintained between 60- 75mmHg. Heart rate ranged between 80-100 beats per minute. Oxygen saturation was between 99-100%. Surgical procedure: The patient was responding well but 25 minutes into the breast augmentation, the patient’s oxygen saturation dropped to 92%. Upon examination of the endotracheal tube, there was frothy, bloody, exudate filling the tube. Auscultation of the chest revealed mild bilateral rales and decreased compliance. Capnography curve revealed an obstructive pattern. And 50 minutes after the start of surgery, the capnography curve ceased to display an obstructive pattern. However upon auscultation, rales were still heard and there was still decreased compliance. A fiber-optic bronchoscopy was performed and bloody, frothy, exudate was witnessed at the carina. No other pathology was seen. A chest x-ray displayed bilateral pulmonary edema. CBC, BMP, PT/INR, PTT were unremarkable. The abdominoplasty was canceled and the patient was ex-tubated uneventfully. The following morning, a routine chest x-ray displayed bilateral pneumothorax despite the patient being asymptomatic. A chest tube was inserted and the rest of her hospital stay was uneventful. Discussion: Pulmonary edema occurs when the normal forces keeping fluid out of the lungs is disrupted. Obeying Starling’s law, (Net Fluid Out = Κ [(Pc-Pi)-Δ (πc-πi)) the normal lung tends to keep the fluid out of the interstium and in the capillary. Where K is filtration constant, Pc is capillary hydrostatic pressure, Pi is interstitial hydrostatic pressure, Δ is reflection coefficient, πi is interstitial oncotic pressure, and πc is capillary oncotic pressure (Aye et al., 2012). Once fluid leaves the capillaries, it tends to track along interstitial space to the perivascular and peribronchial space within the lung. During the later stages of pulmonary edema, the interstitial fluid leaks into the alveoli. As the alveoli become filled with fluid, they become unventilated which prevents oxygenation of blood. The lack of gas exchange can produce dangerous hypoxic environments. Most cases of perioperative flash pulmonary edema that have been described are during extubation. The mechanism of edema formation is due to a very large increase in negative intra-thoracic pressure secondary to an obstruction due to laryngospasm (Ibrahim et al., 1999 & Rastogi and Wright, 1969). Barotrauma is the general term describing pulmonary interstitial emphysema, pneumo-mediastinum, pneumo-peritoneum, subcutaneous emphysema, or pneumothorax. The most likely cause of her complications is barotrauma followed by airway instrumentation. The Risk factors that predispose patients to barotraumas is by alveolar over distention which include high tidal volumes, high inflation, high inspiratory airway pressures caused by low lung or chest wall compliance, and high PEEP 2. The studies indicate that a peak airway pressure between 50-70 cm H2O can lead to pneumothorax.( Haake et al., 1999) References Aye, C. Y. L., McKean, D., Dark, A., & Akinsola, S. A. (2012). Bilateral primary spontaneous pneumothoraces postcaesarean section– another reason to avoid general anaesthesia in pregnancy. BMJ Case Reports, 2012. Ibrahim, A. E., Stanwood, P. L., & Freund, P. R. (1999). Pneumothorax and systemic air embolism during positive-pressure ventilation. Anesthesiology, 90(5), 1479-1481. Haake, R., Schlichtig, R., Ulstad, D. E. A., & Henschen, R. R. (1987). Barotrauma. Pathophysiology, risk factors, and prevention. CHEST Journal, 91(4), 608-613. Rastogi, P. N., & Wright, J. E. (1969). Bilateral tension pneumothorax under anaesthesia. Anaesthesia, 24(2), 249-252. A female patient with Intra-operative Pulmonary Edema and Bilateral Spontaneous Pneumothorax Norvan Vartevan, DO, Juan Carlos Cucalõn, MD, Corine Munnings, MD. (Department of Anesthesia, Larkin Community Hospital)
