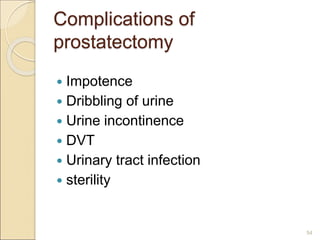
This document discusses benign prostate hypertrophy (BPH). It begins by reviewing the anatomy and physiology of the prostate gland. BPH is defined as a non-cancerous enlargement of the prostate gland caused by increased hormones like testosterone. Common signs include difficulty urinating. Diagnosis involves digital rectal exam, ultrasound, and blood tests like PSA. Treatment options include medications that block hormones or surgery to remove part of the prostate. Post-operative care focuses on risks like infection, bleeding, pain, and urinary problems.