1. The document discusses digital smile design (DSD), which uses presentation software like PowerPoint to analyze facial and dental photos and simulate smile designs.
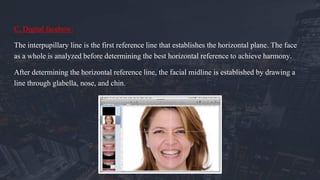
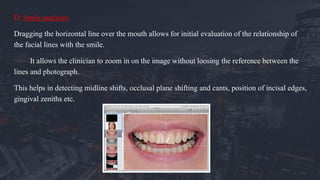
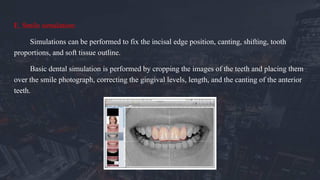
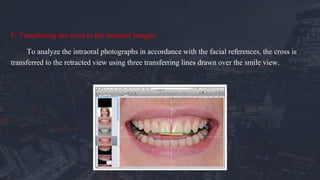
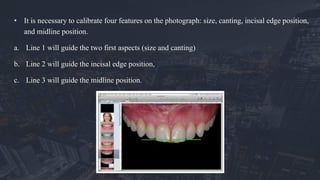
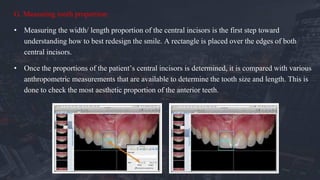
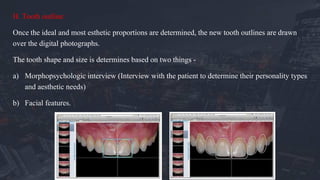
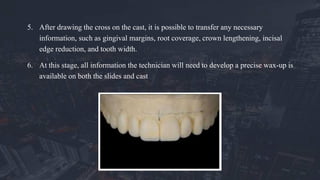
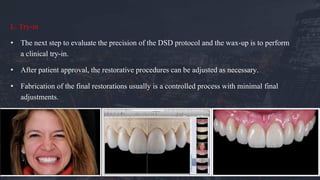
2. The DSD workflow involves taking photos, applying reference lines, analyzing proportions, and simulating tooth shapes. This information is transferred to diagnostic wax-ups and provisional restorations.
3. DSD provides benefits for esthetic diagnosis, communication between clinicians and technicians, feedback throughout treatment, and patient management by helping visualize treatment plans.