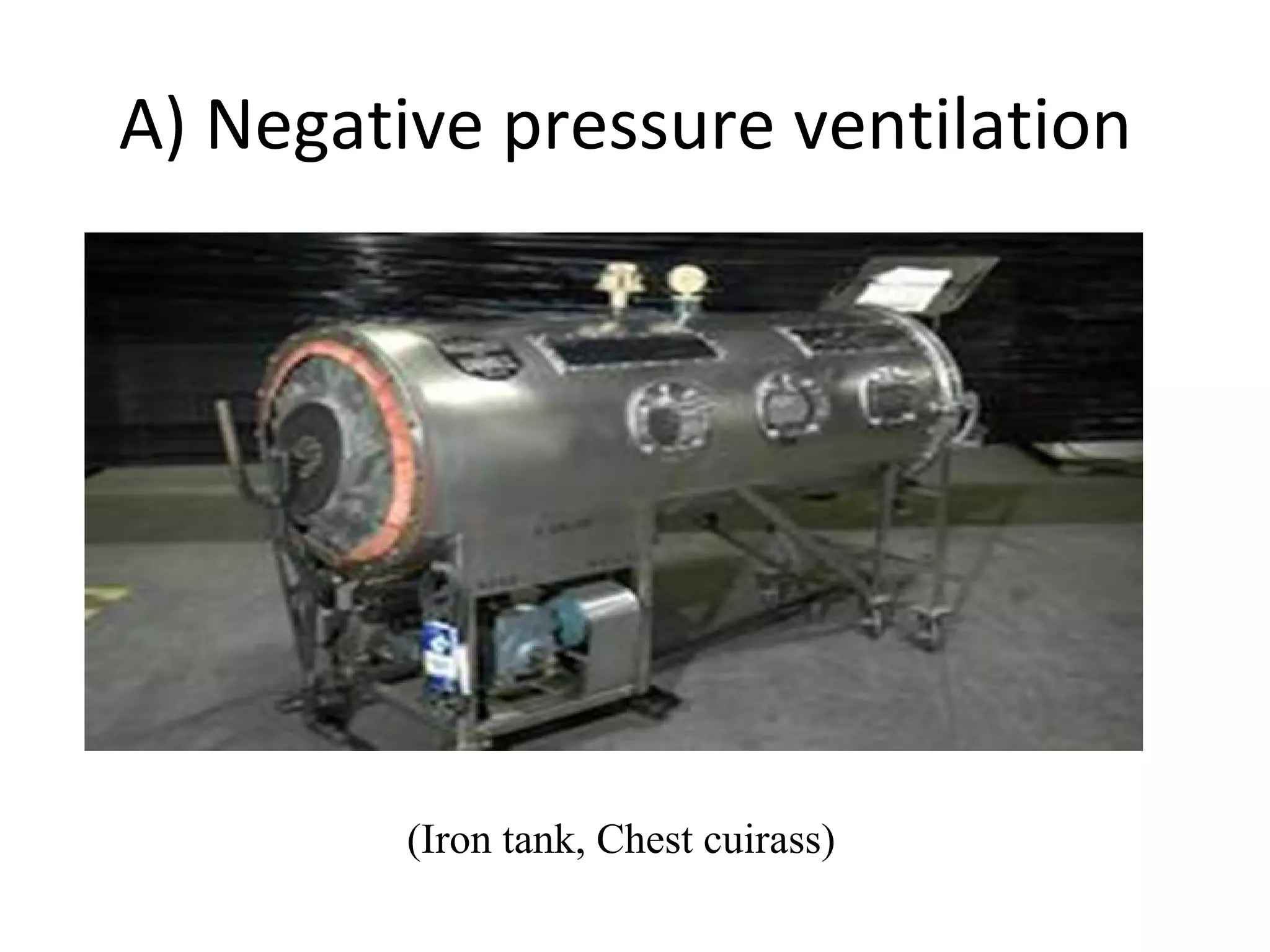
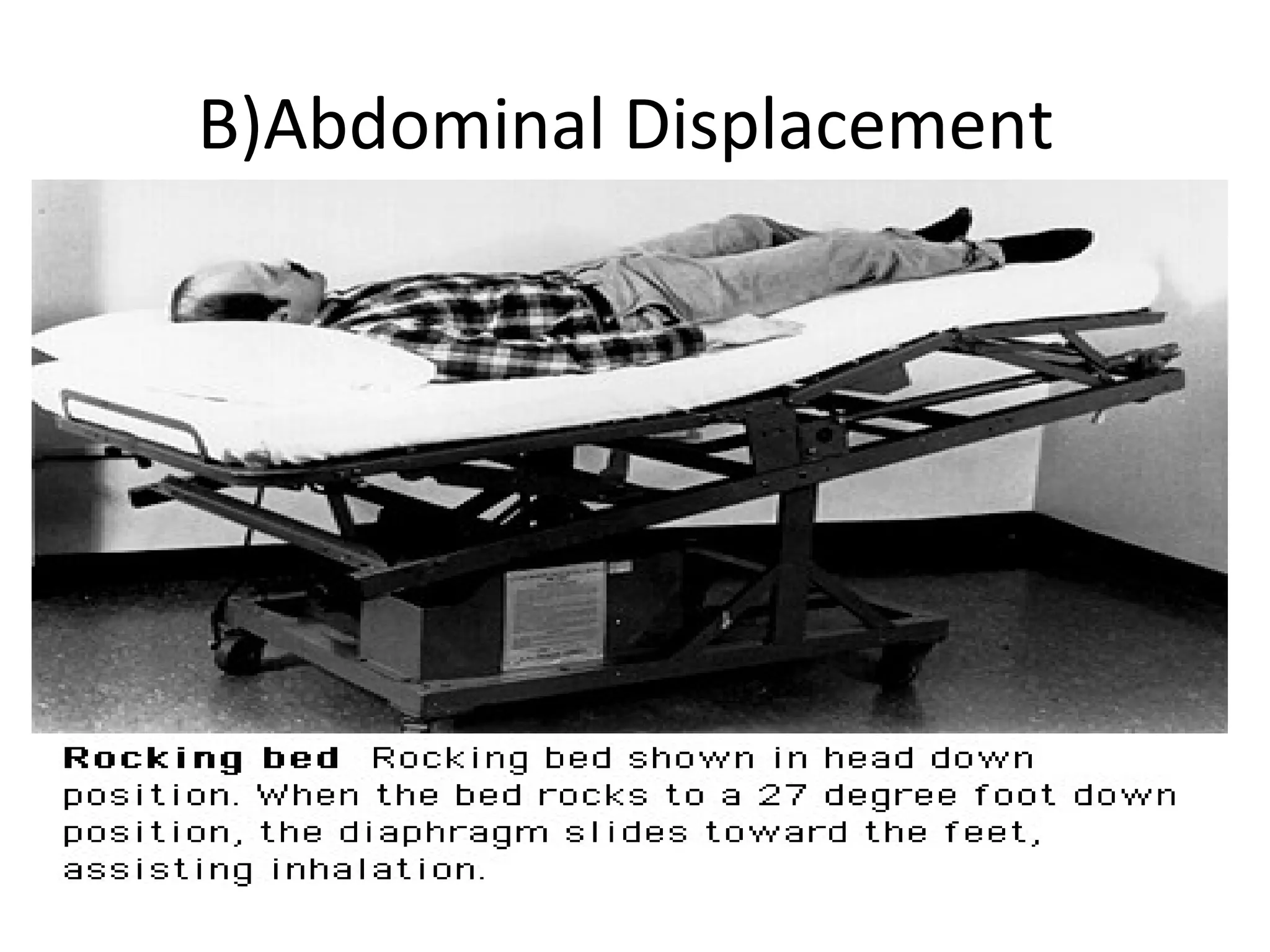
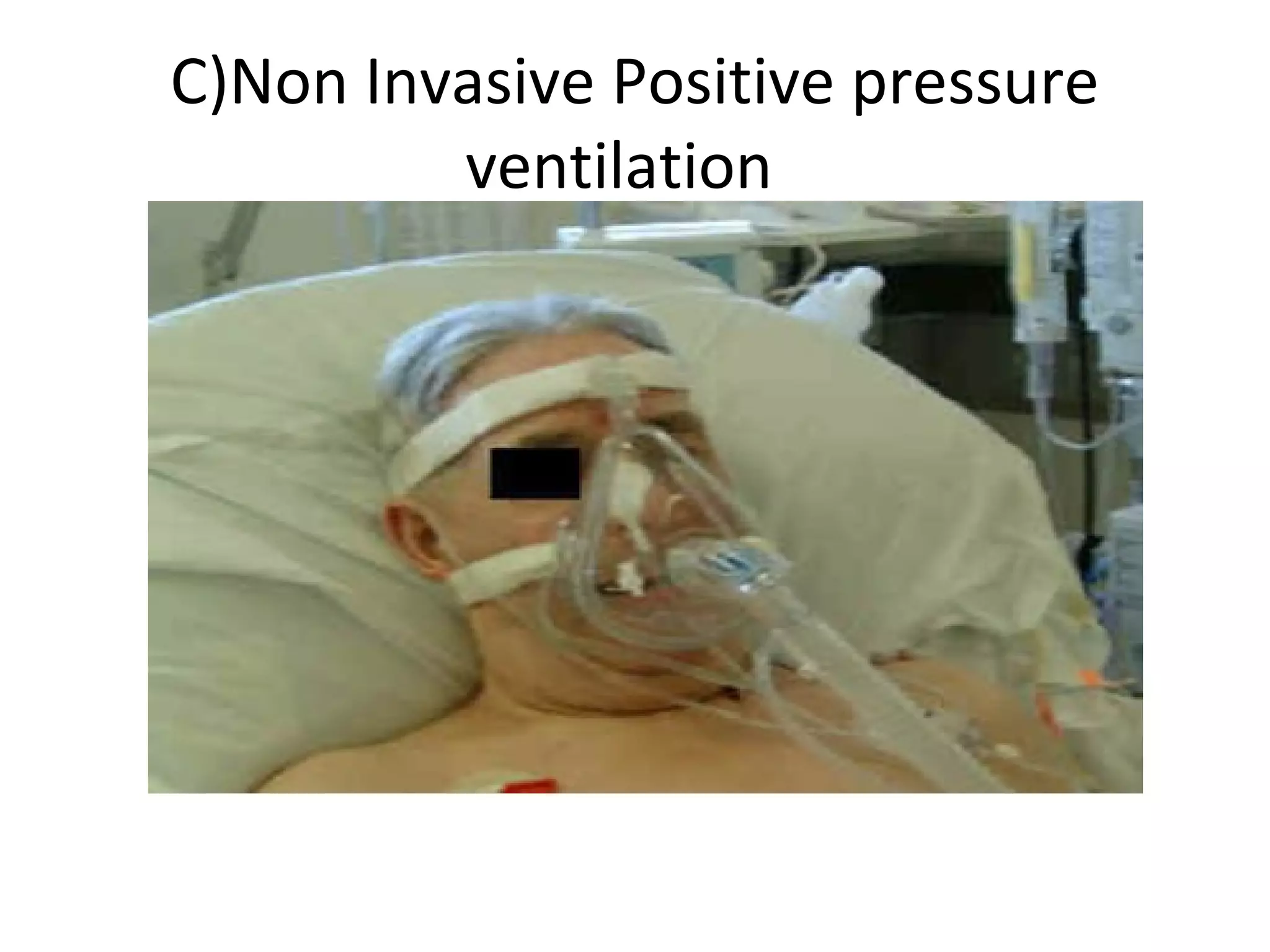
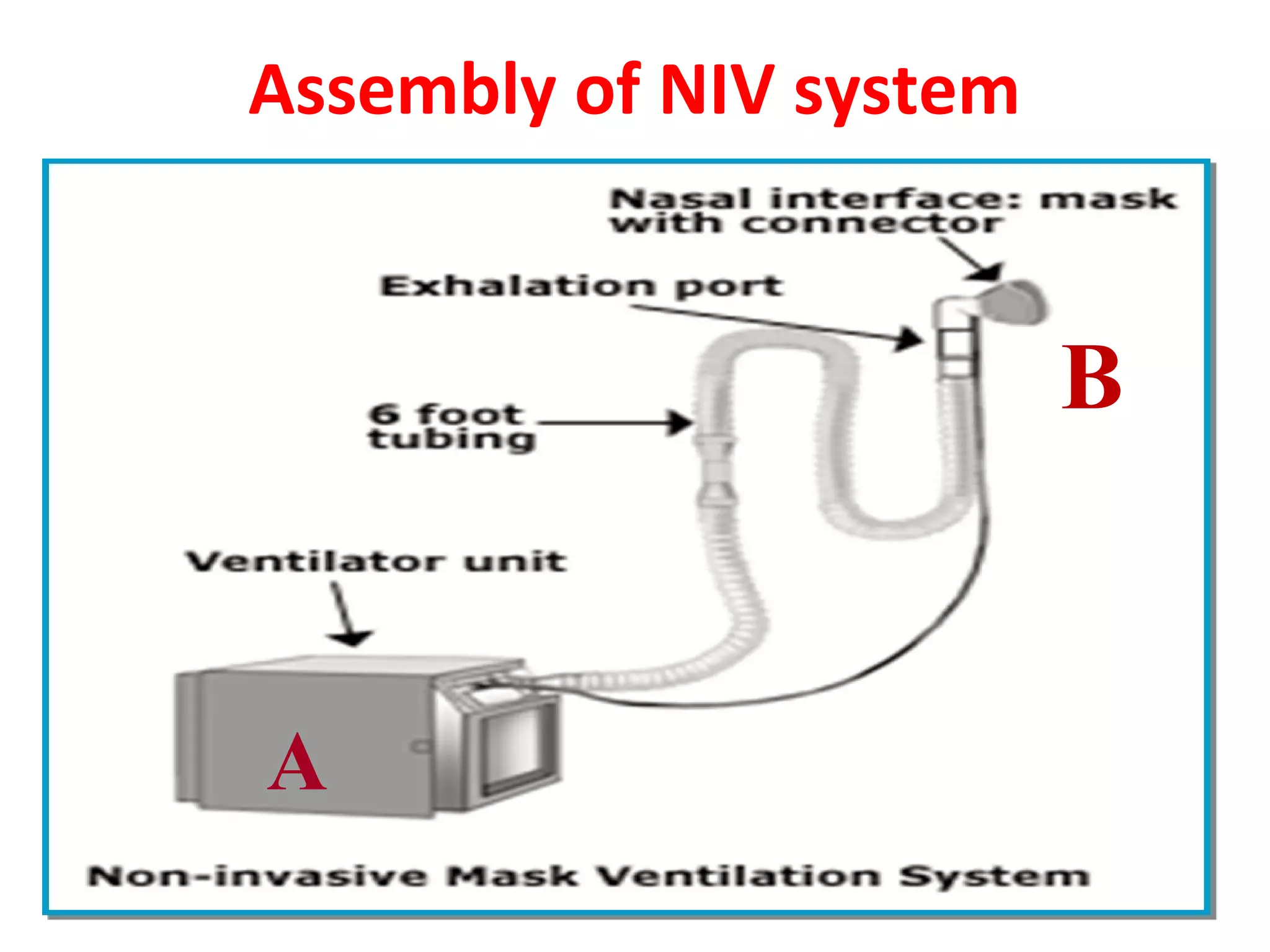
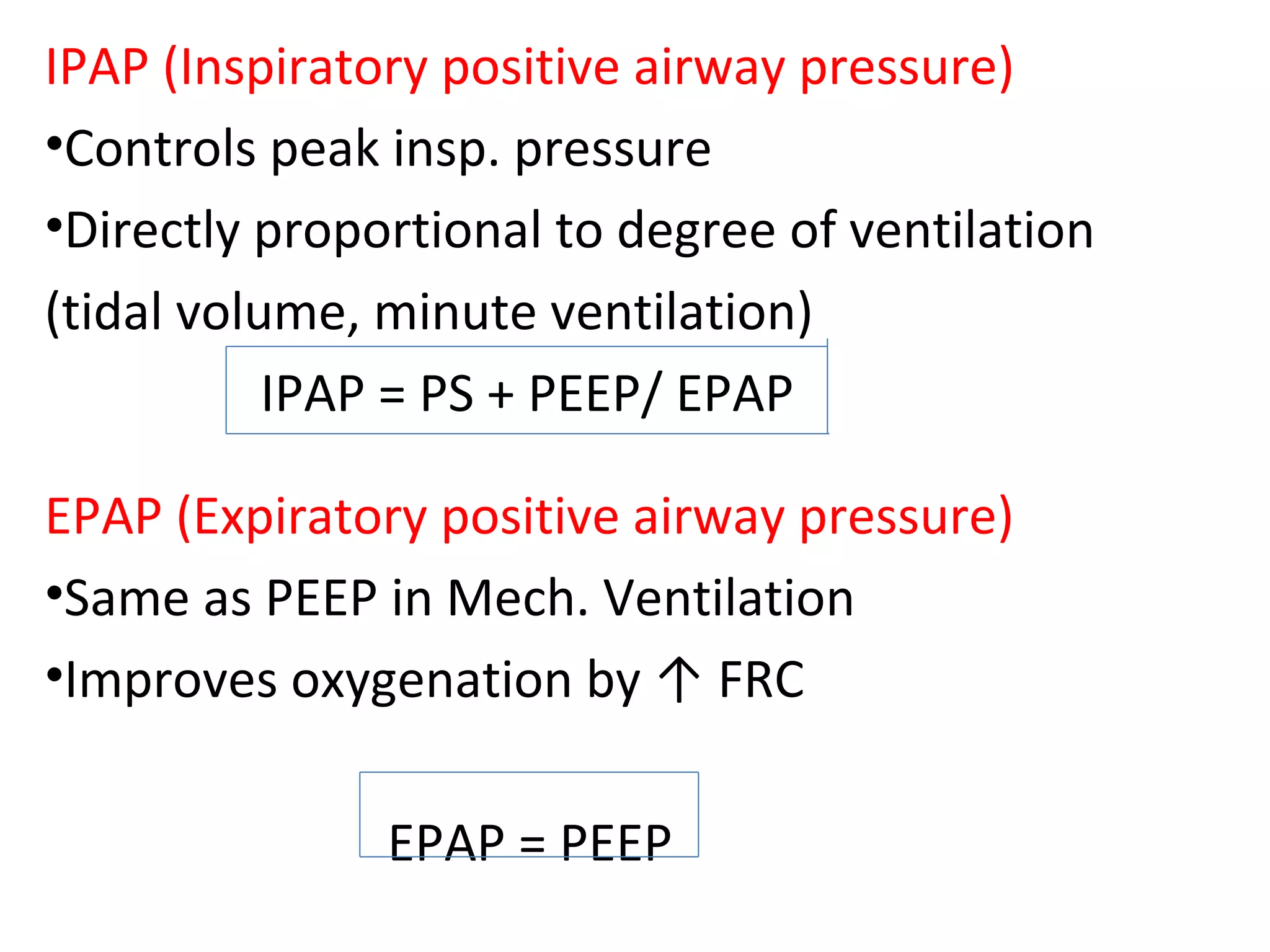
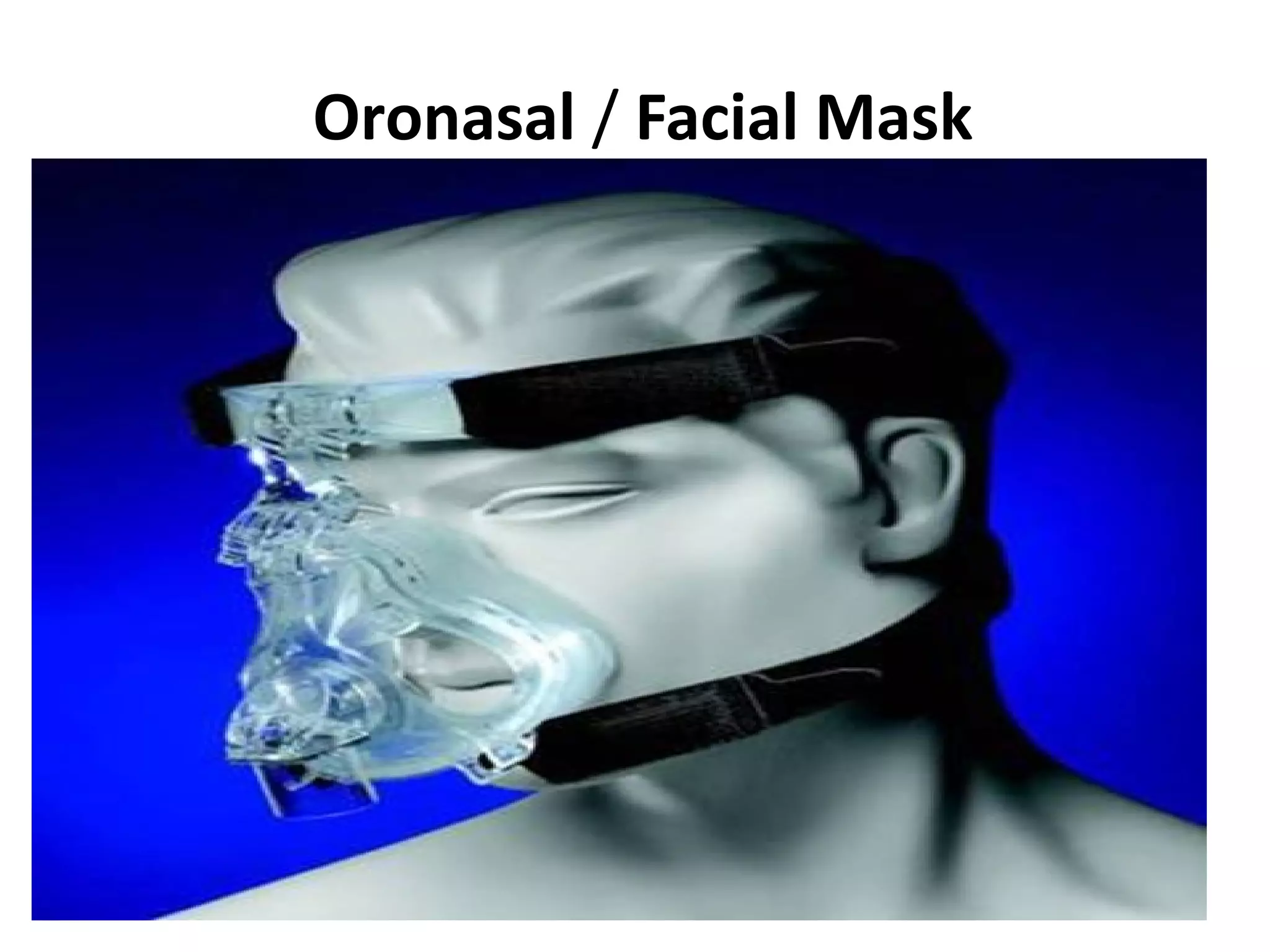
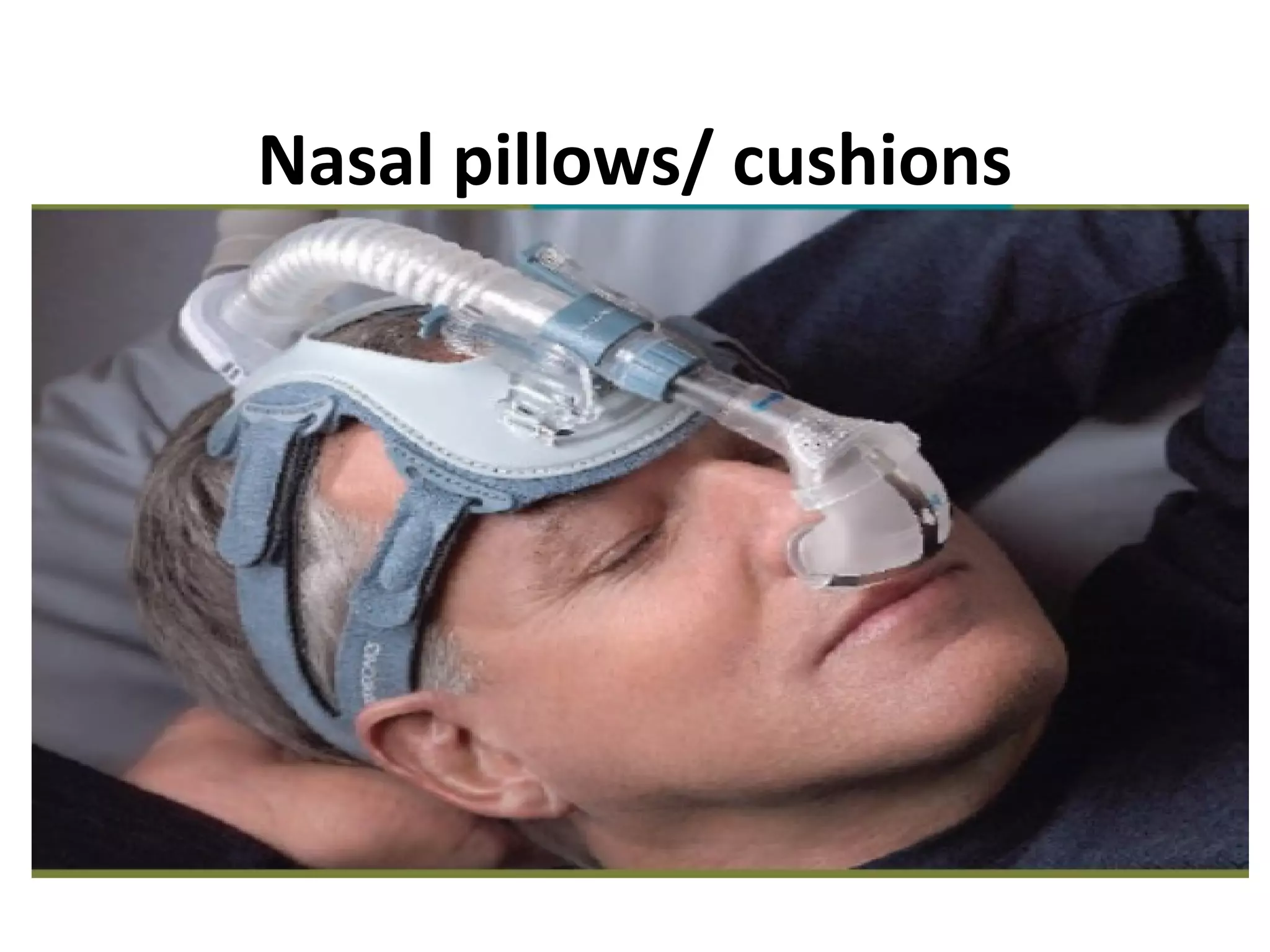
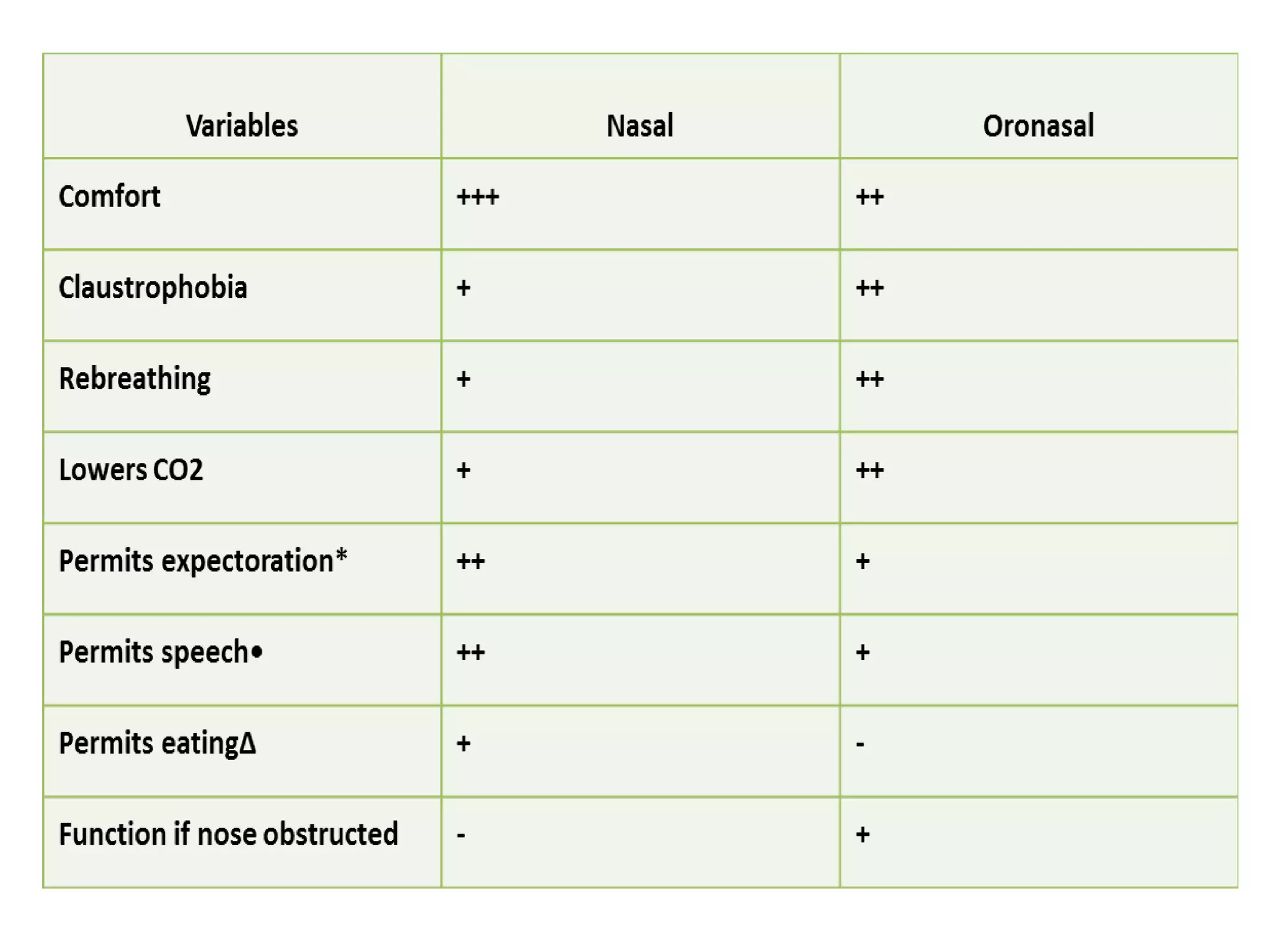
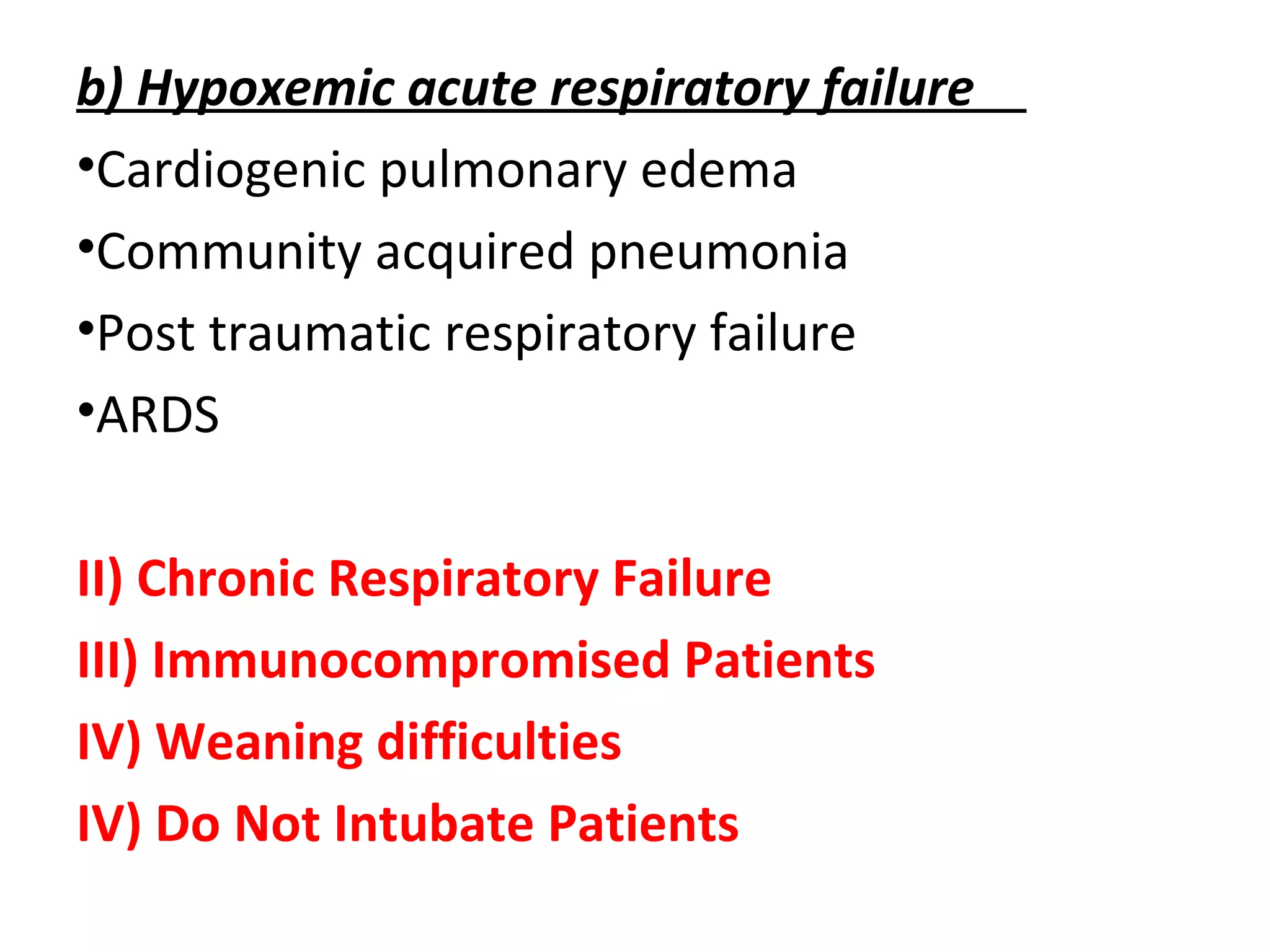
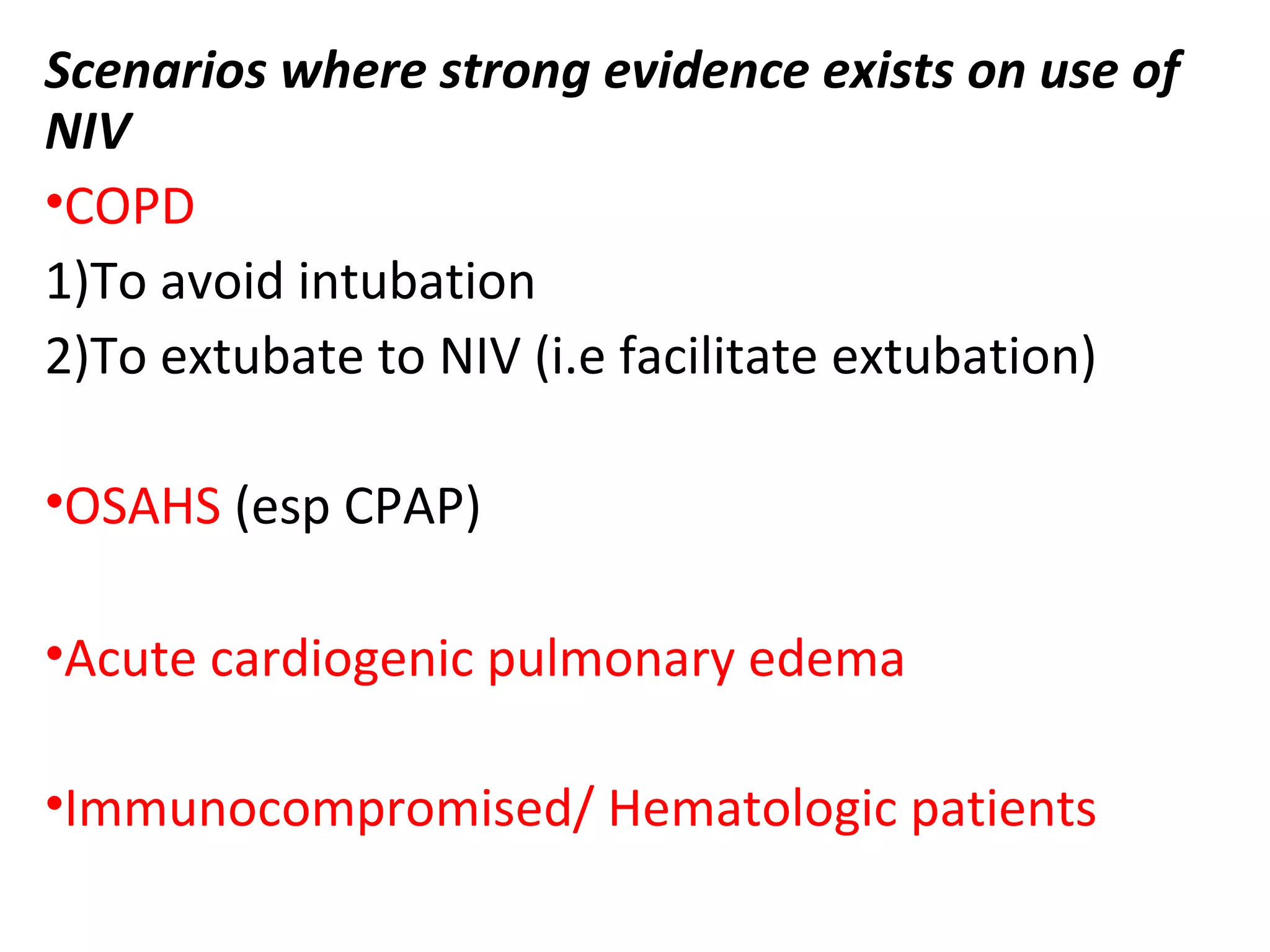
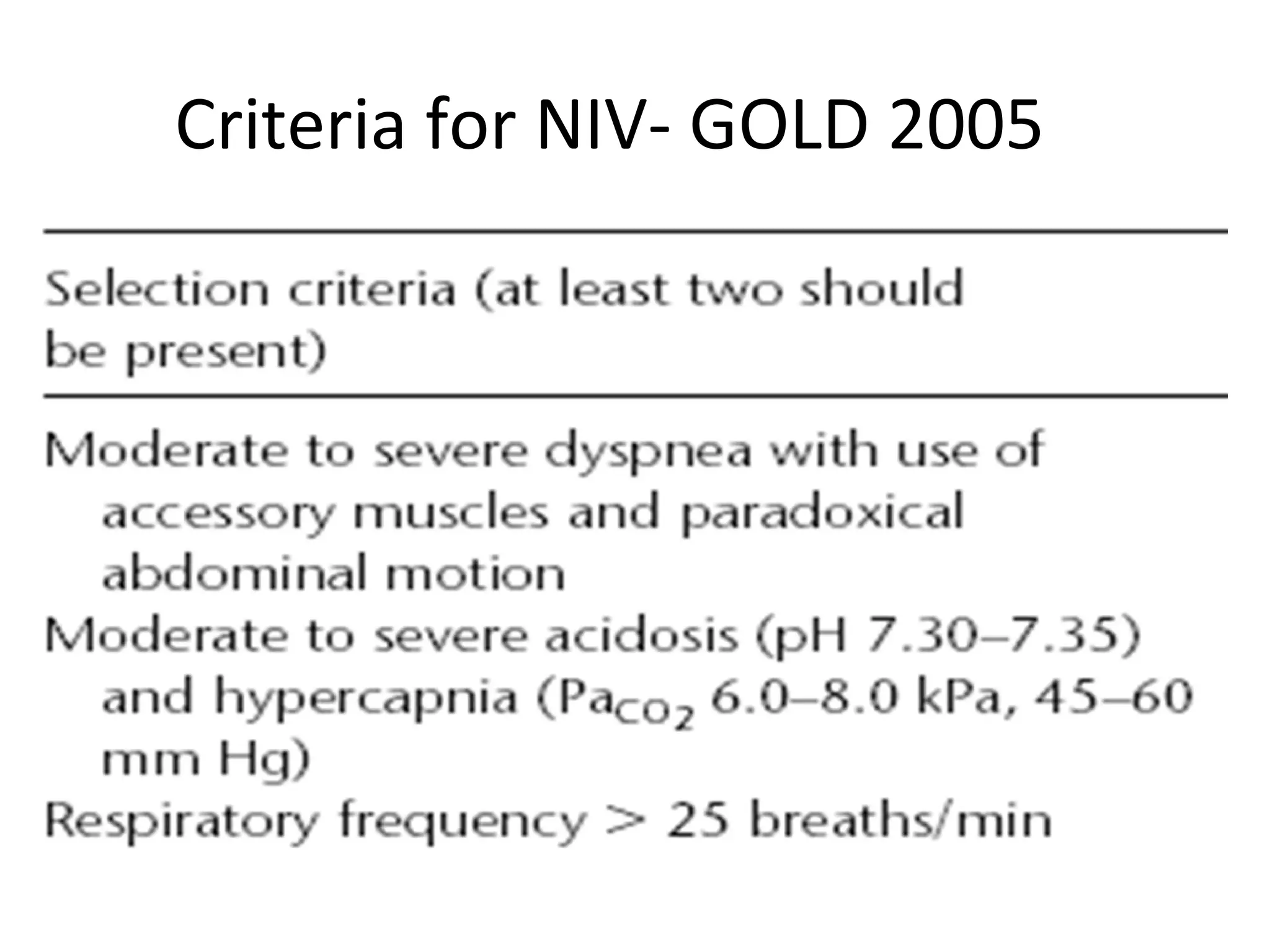
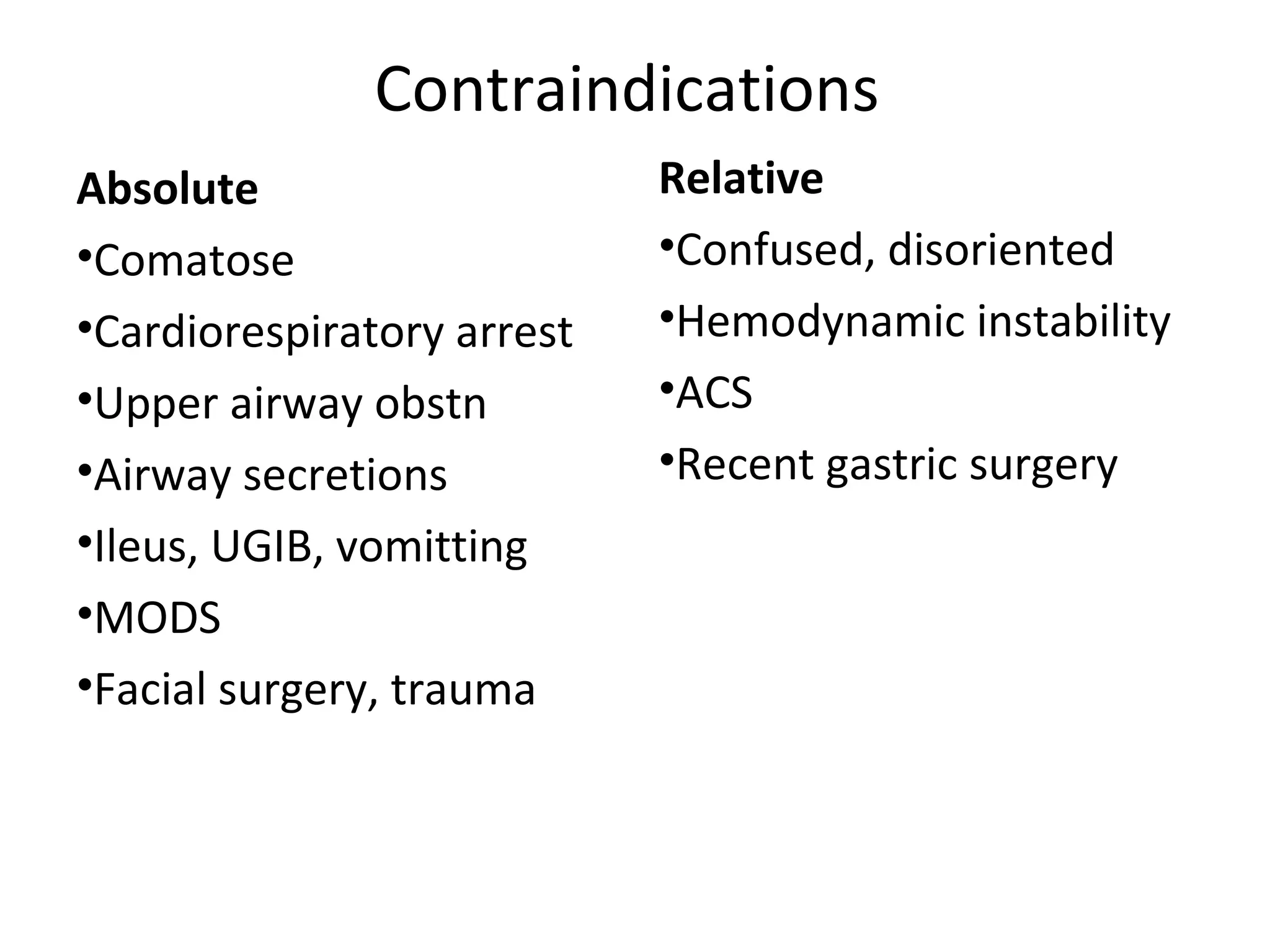
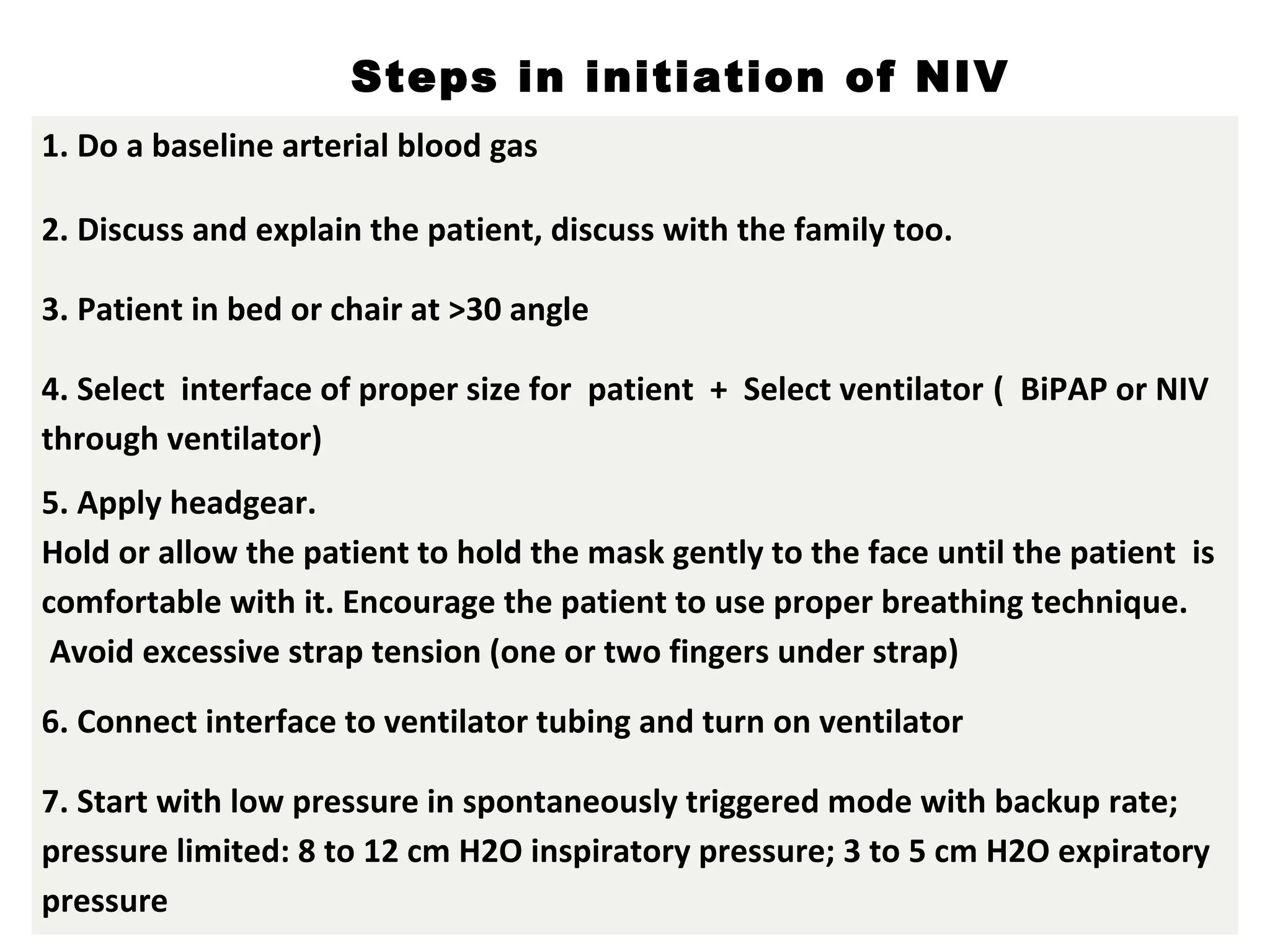
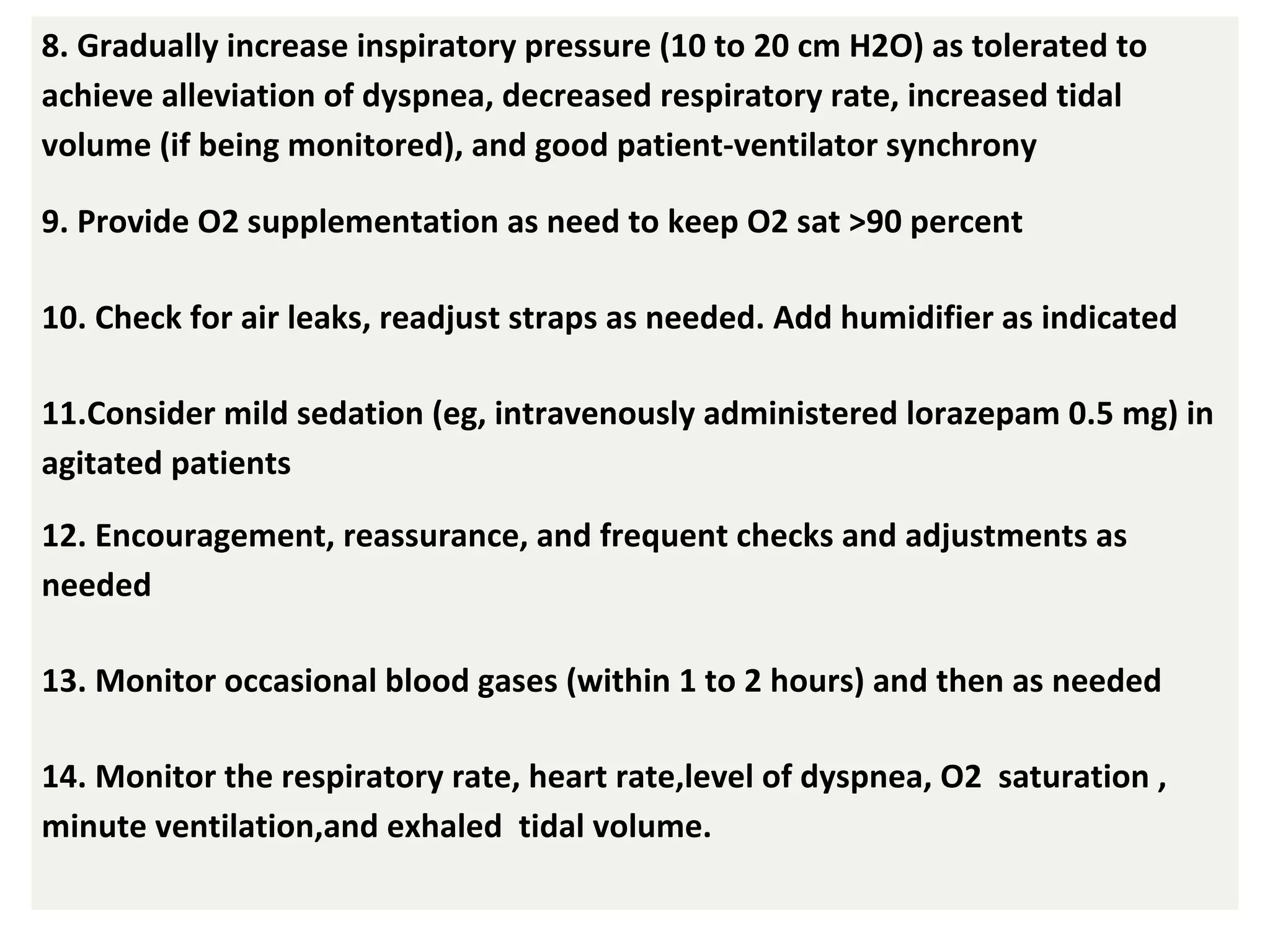
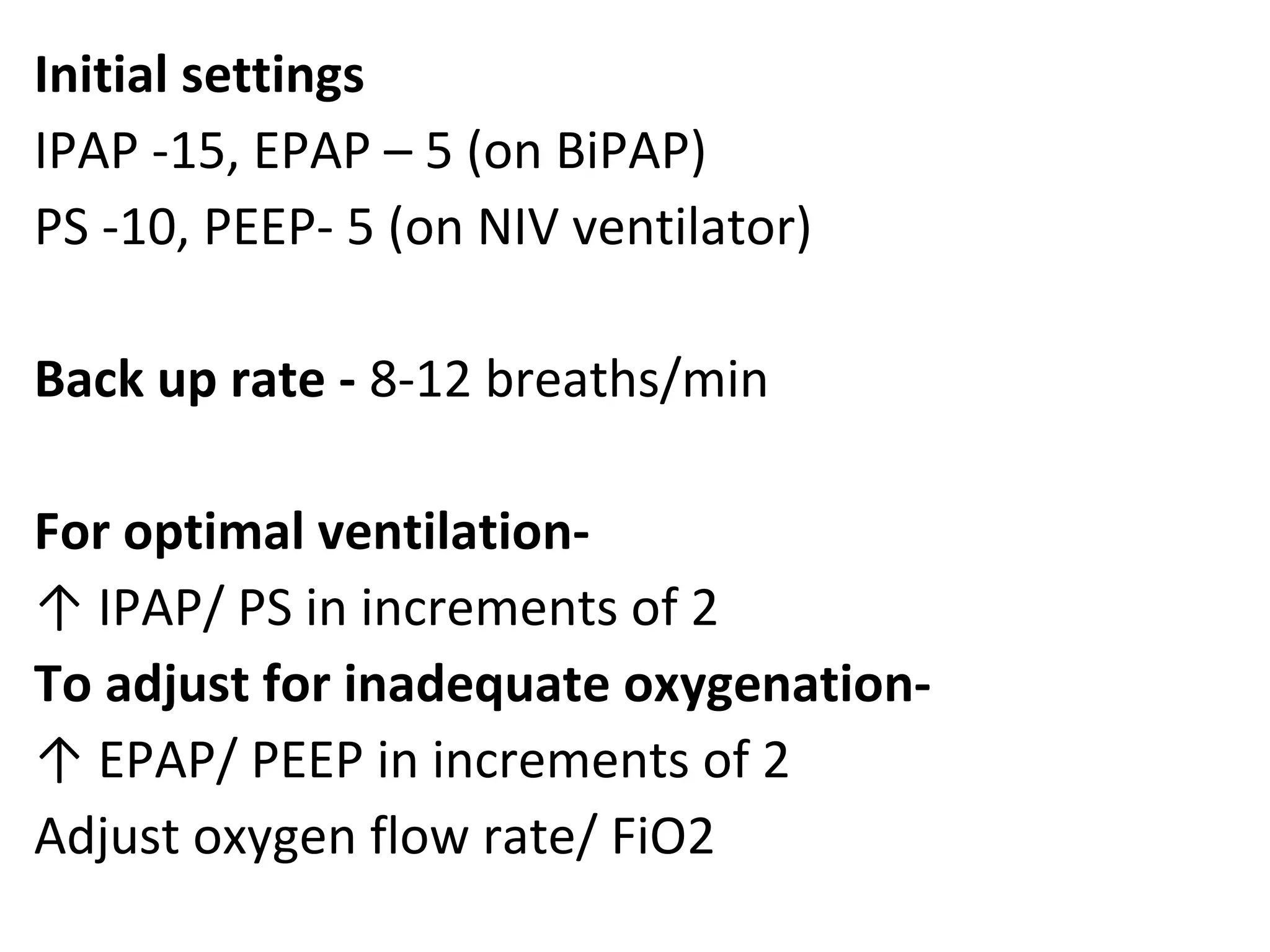
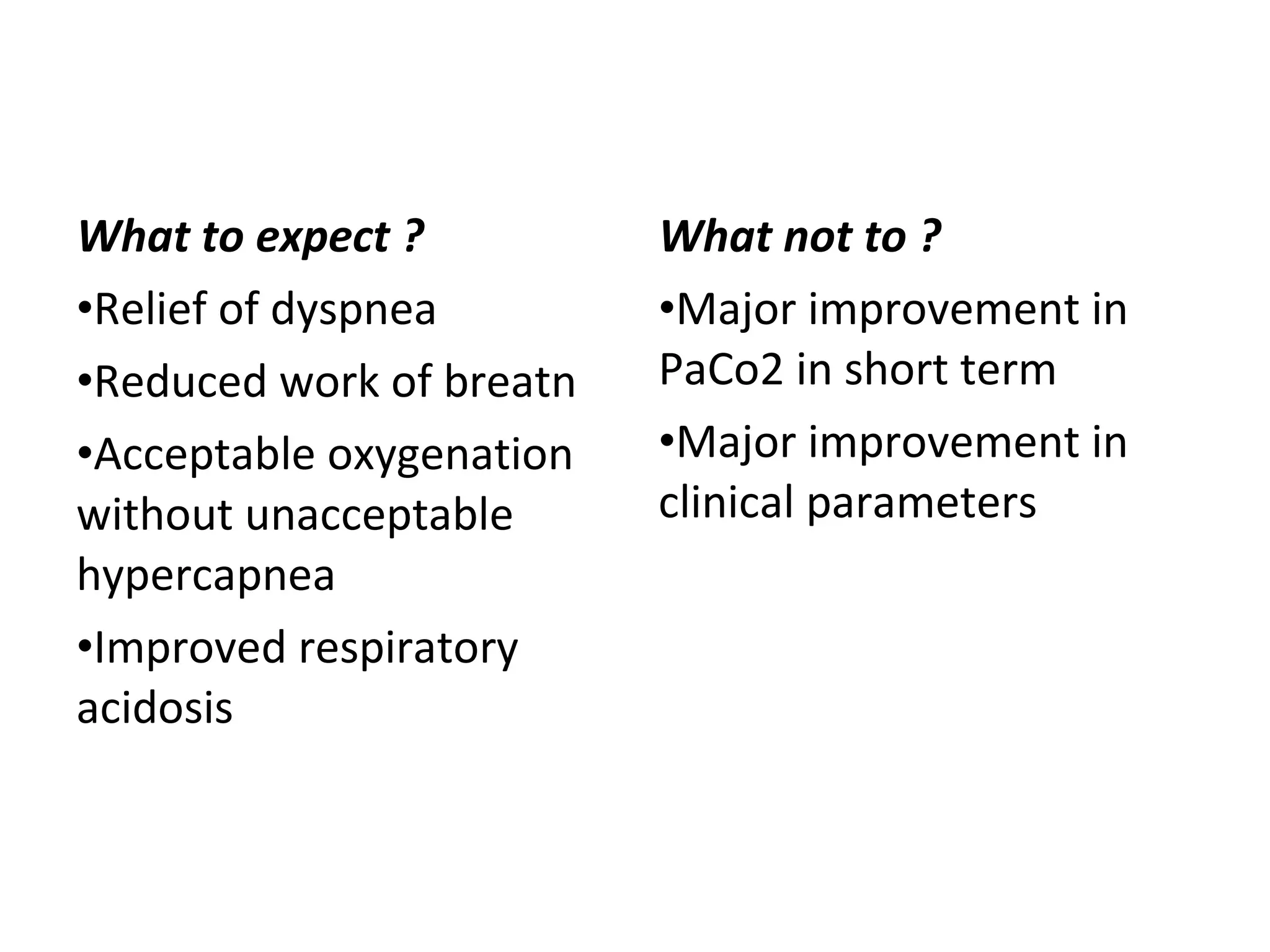
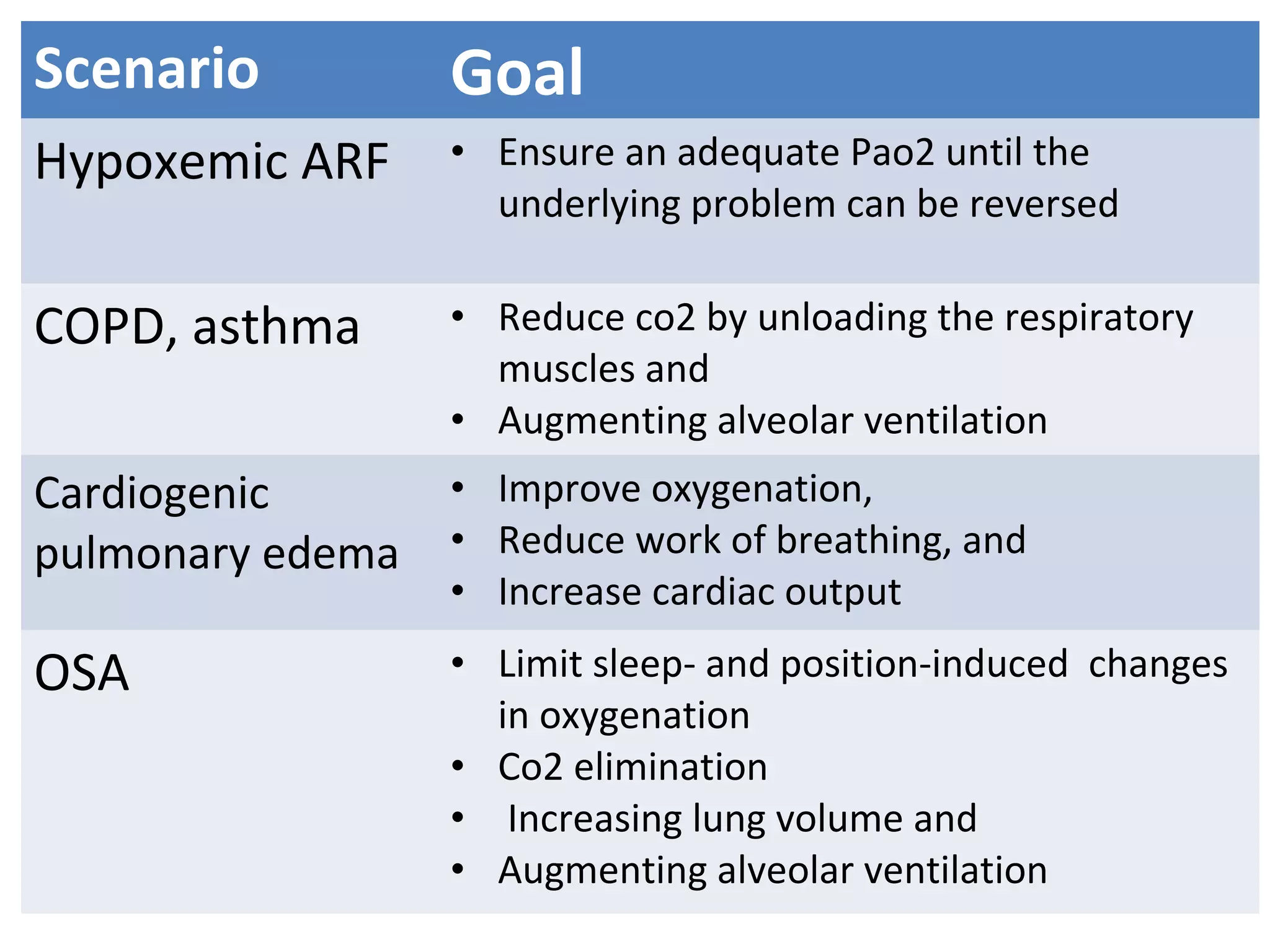
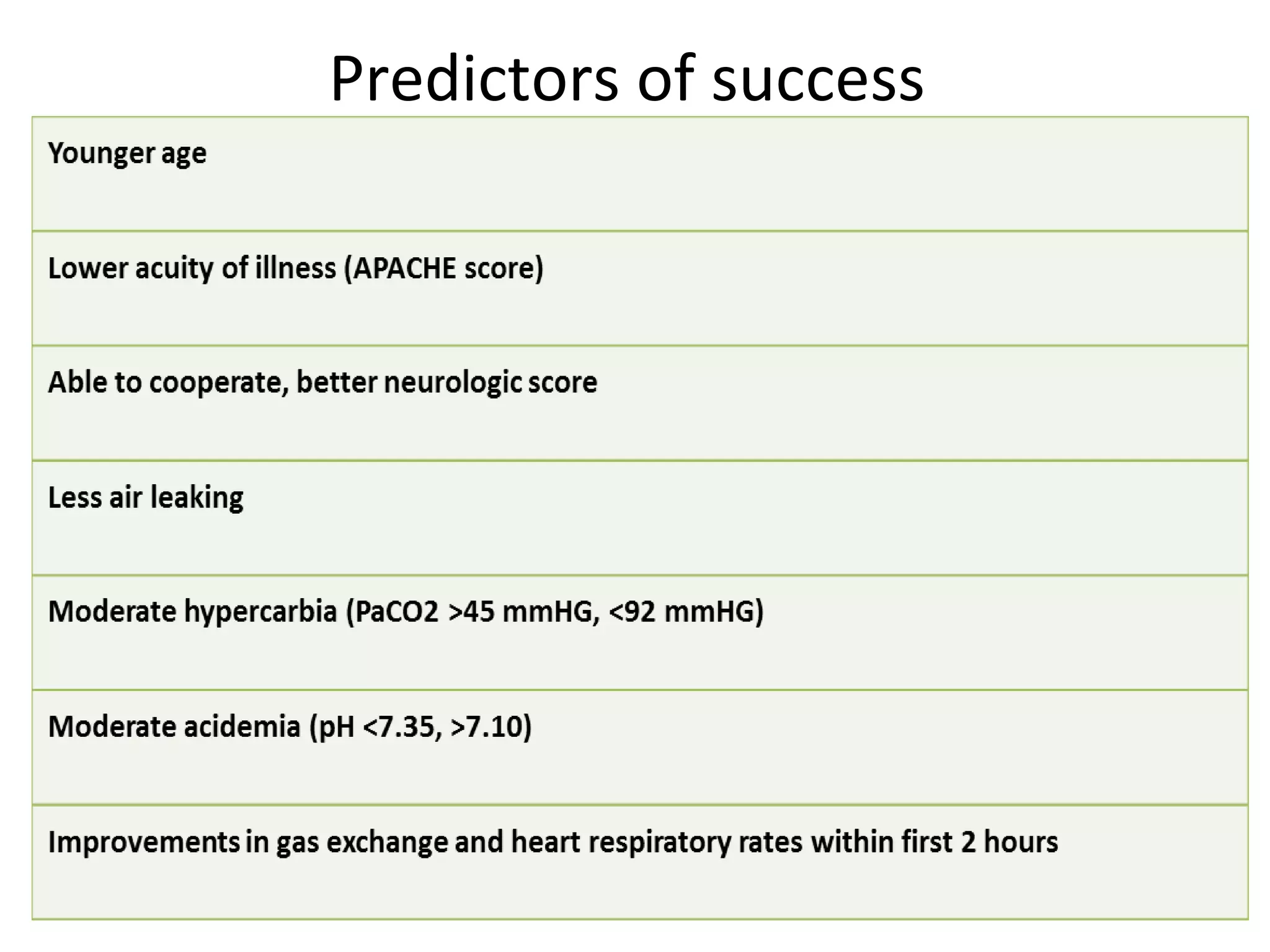
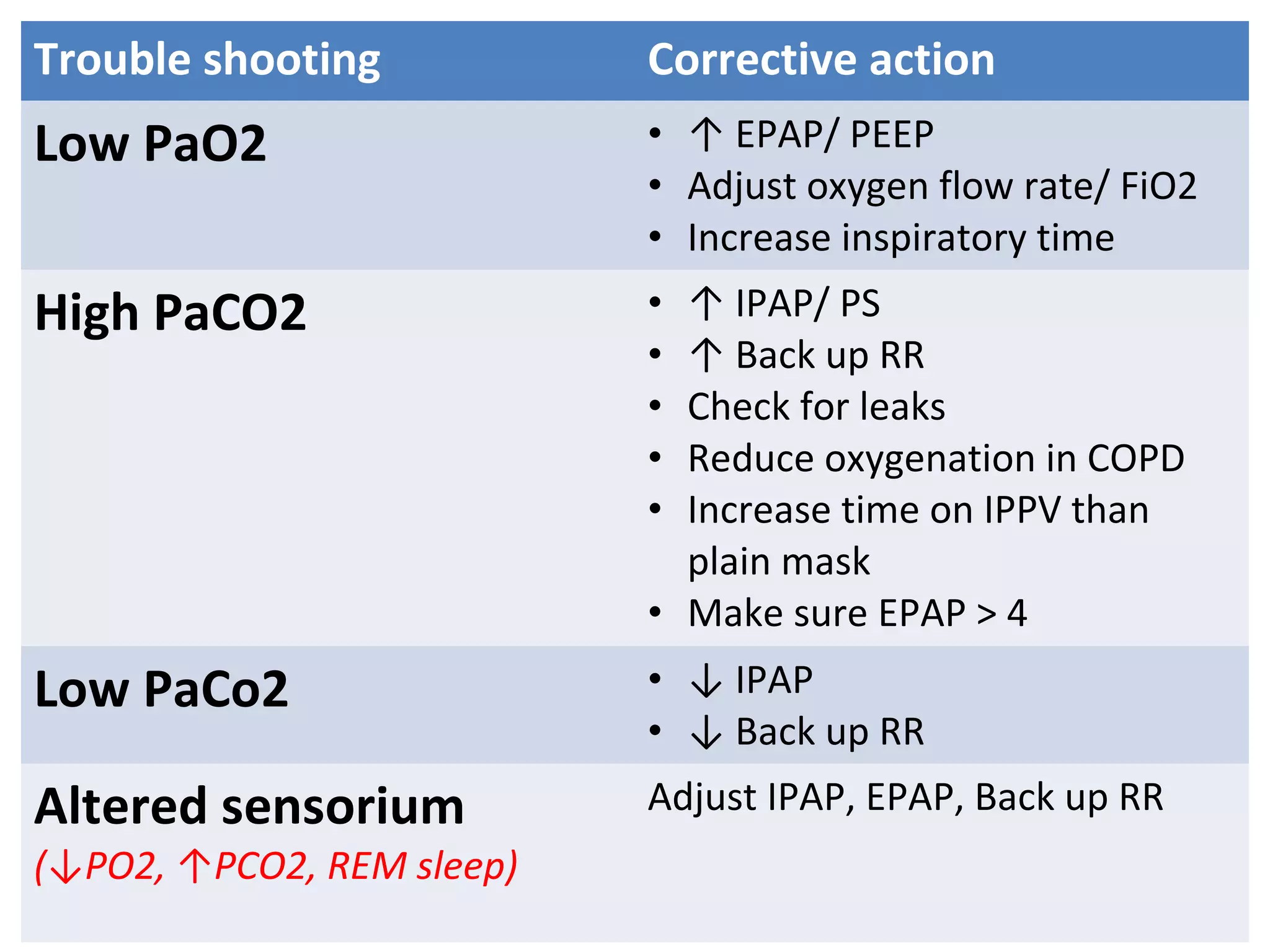
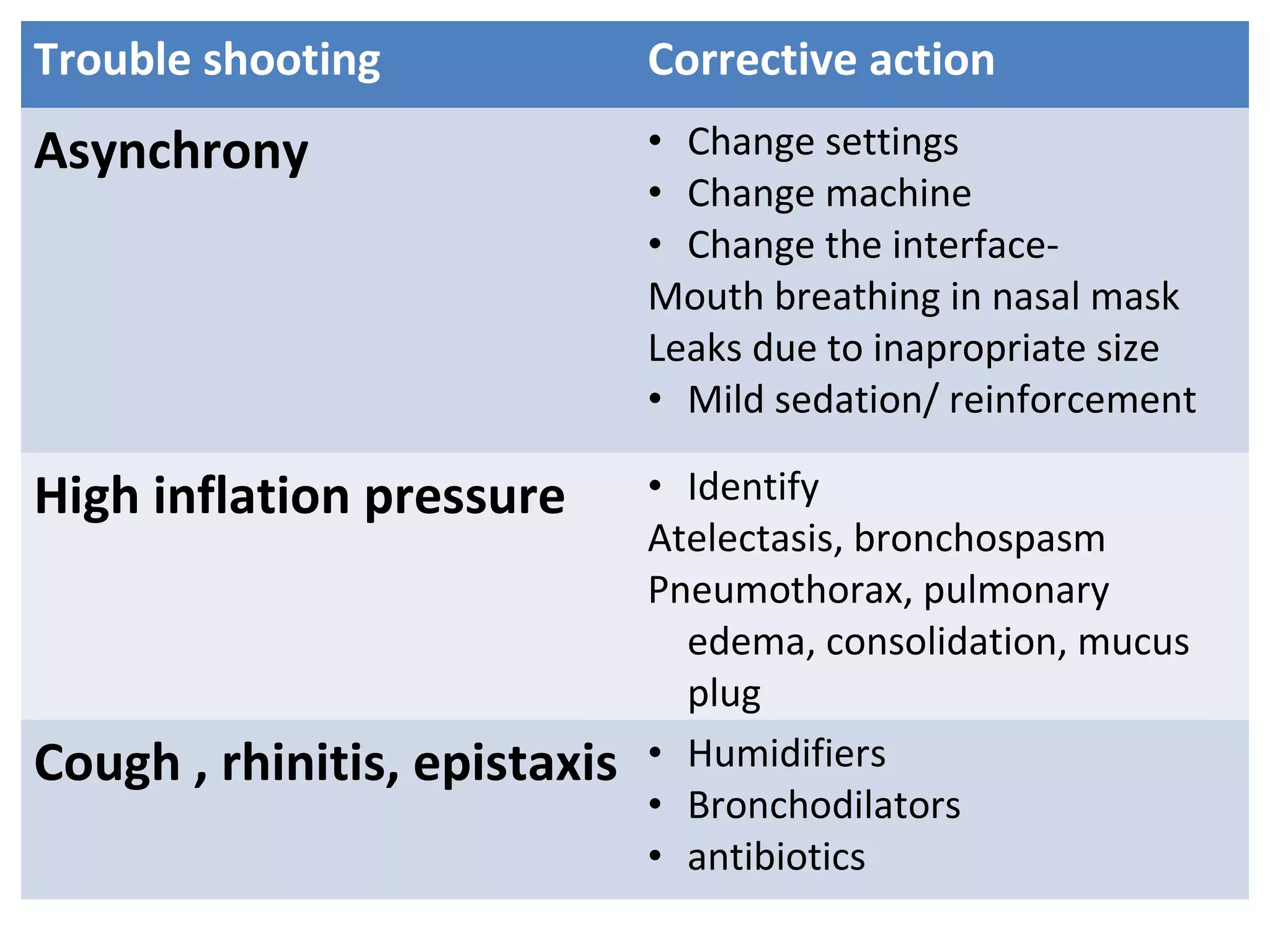
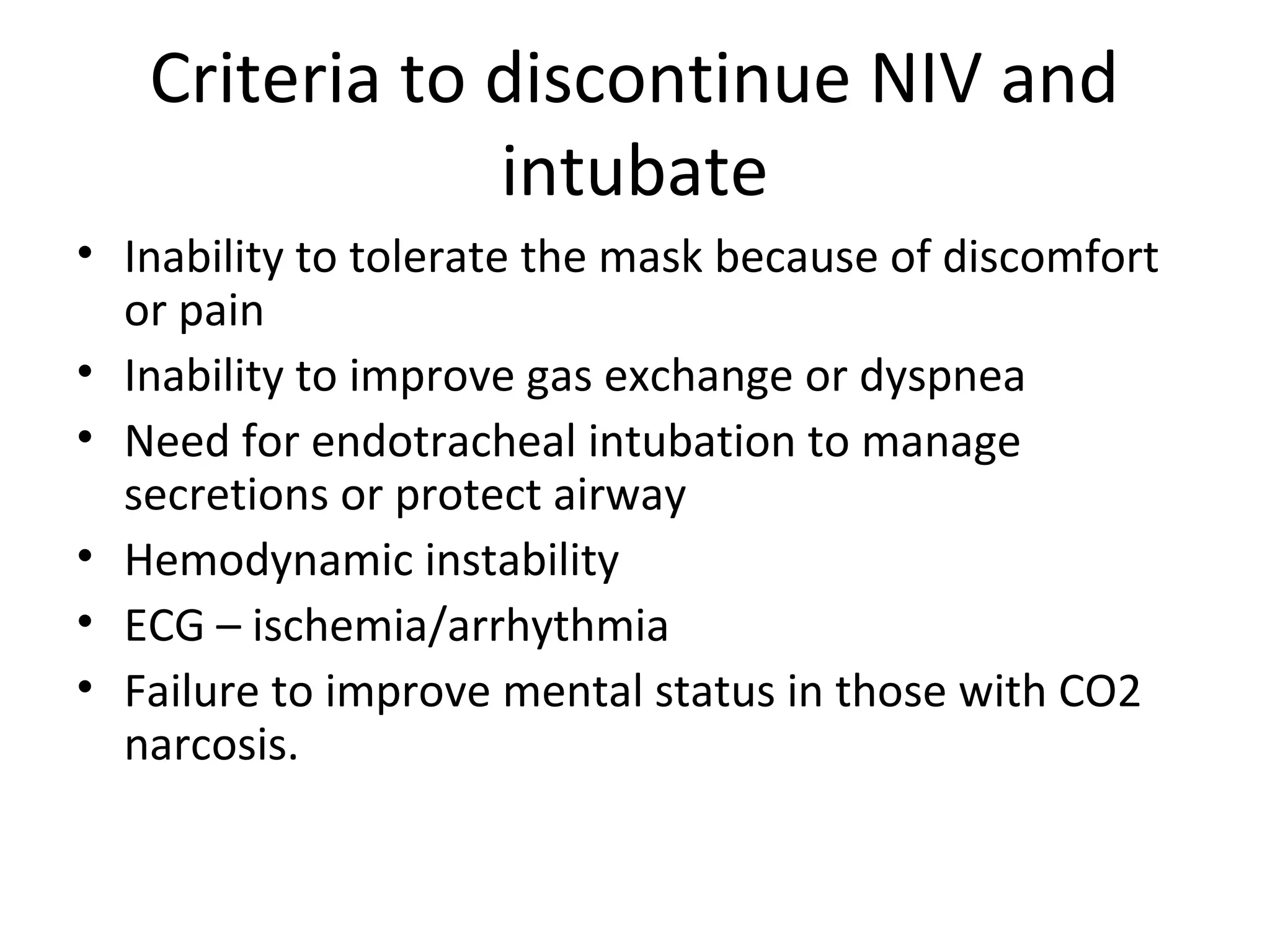
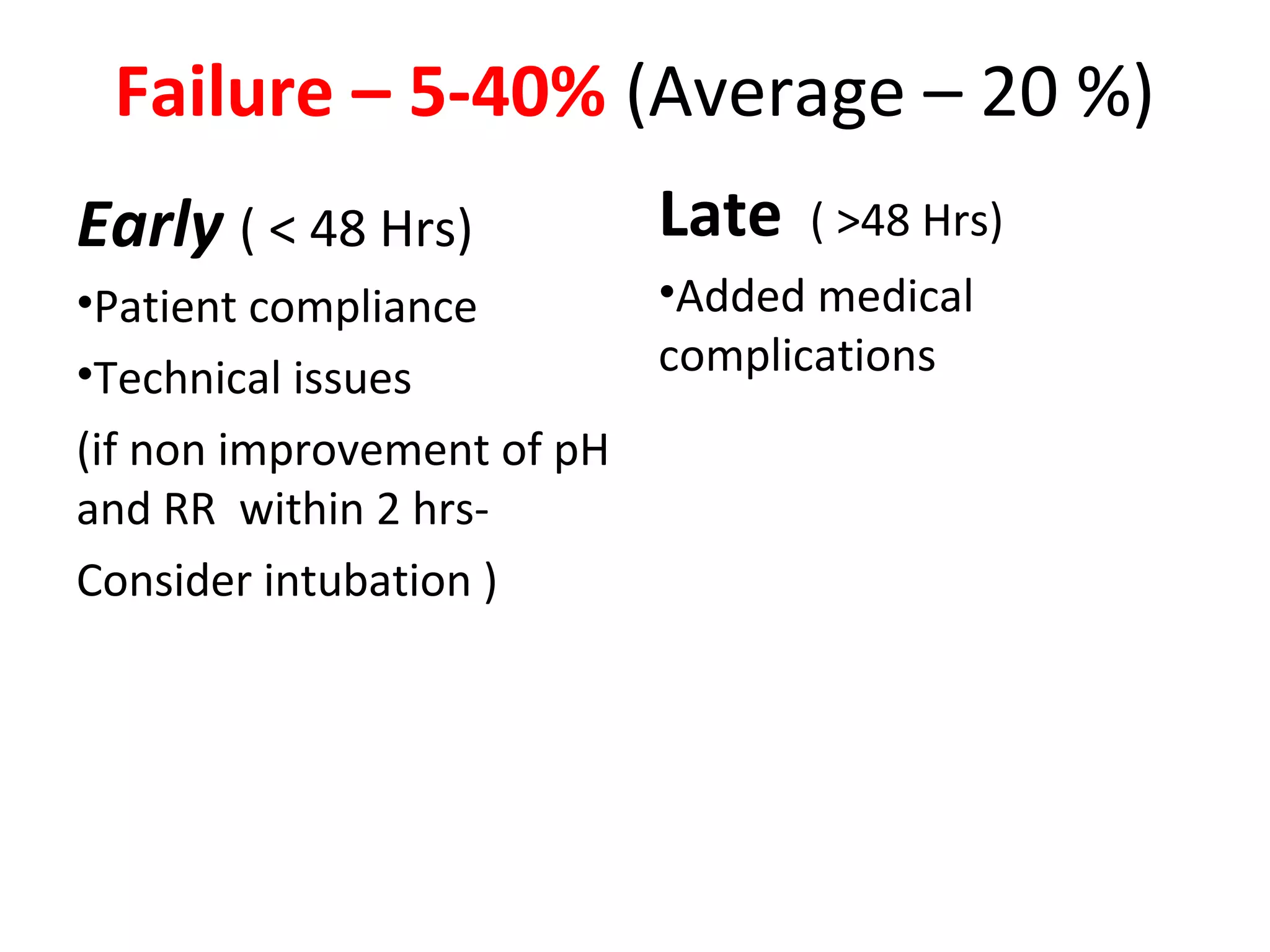
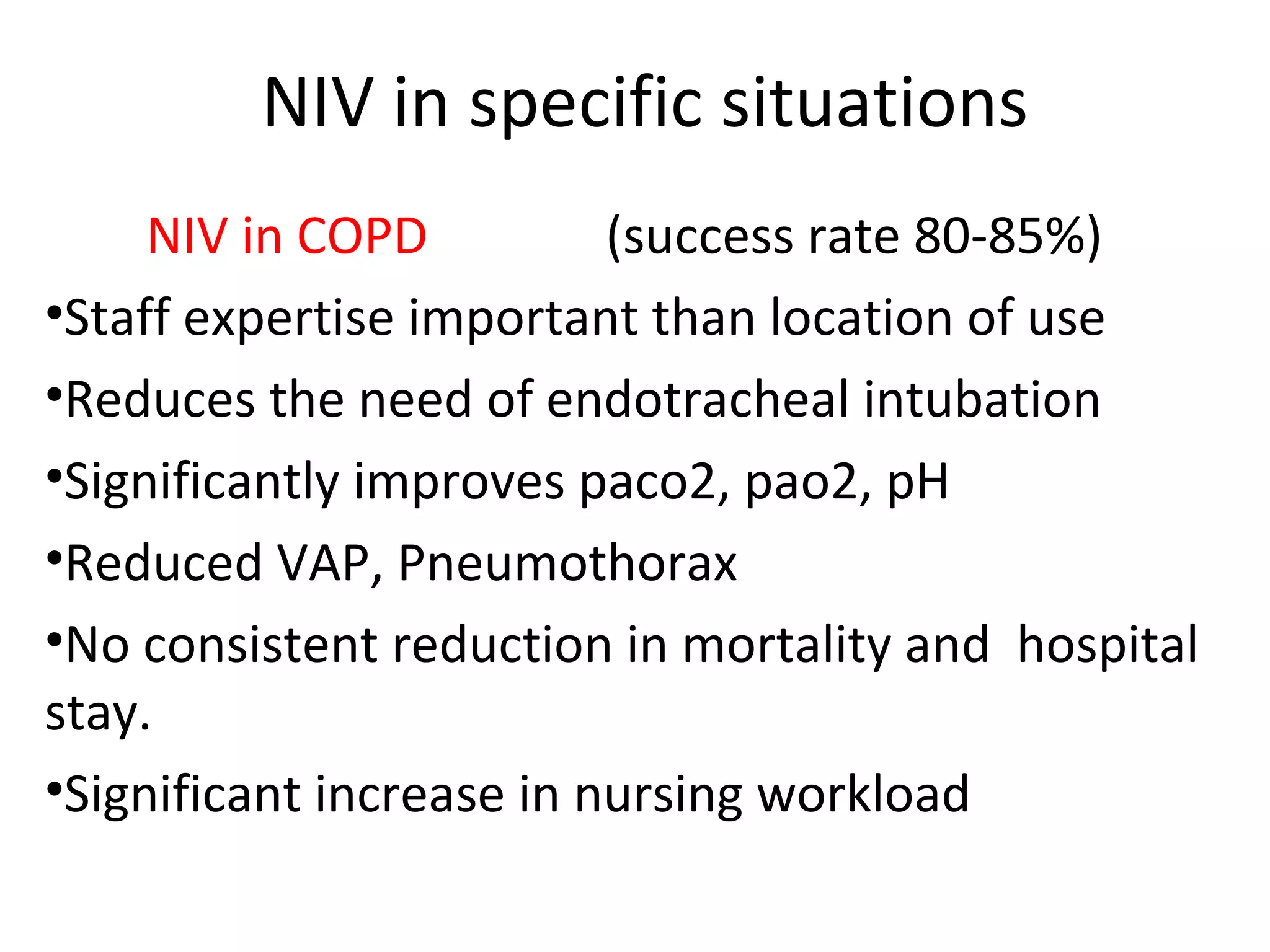
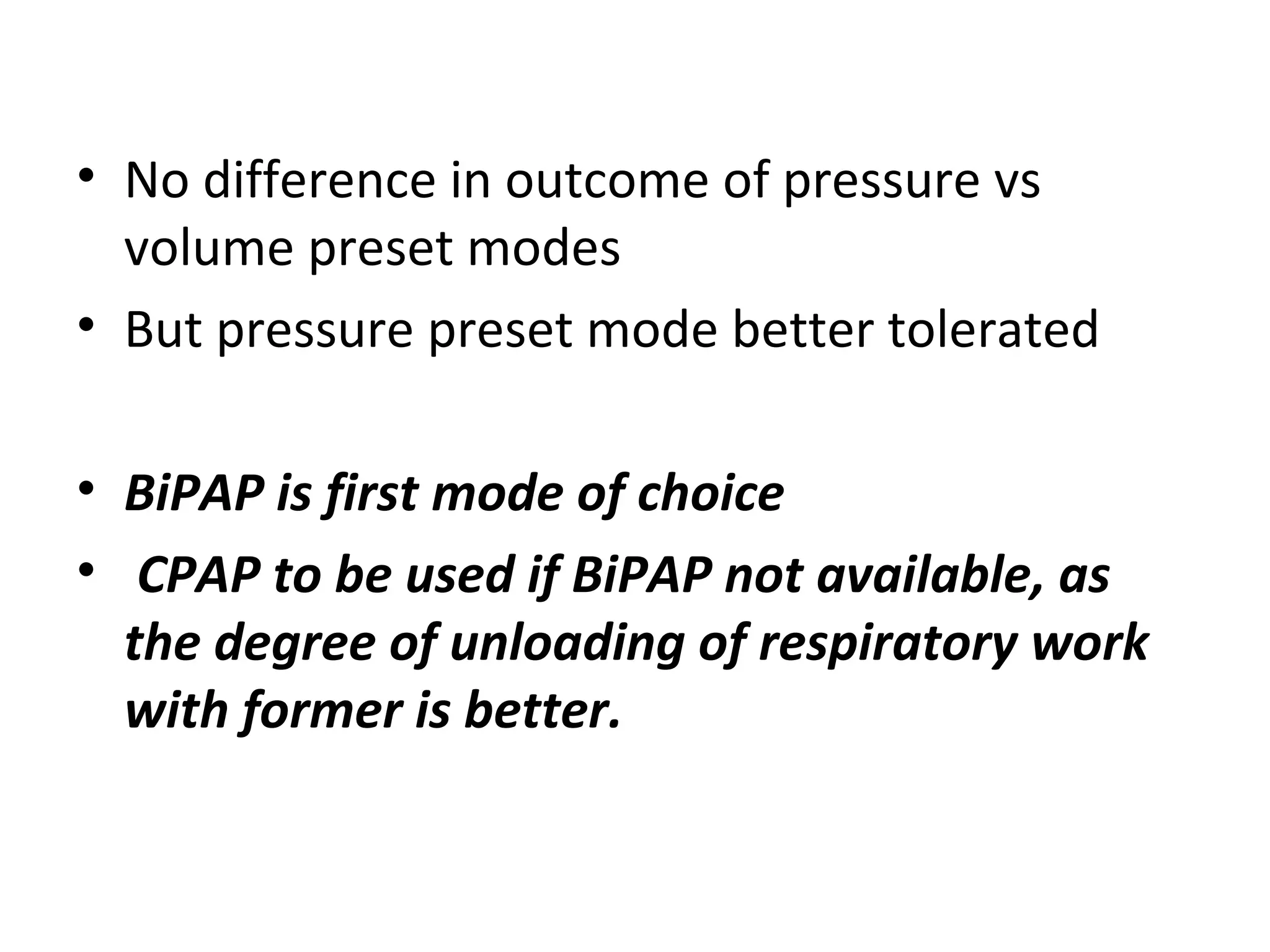
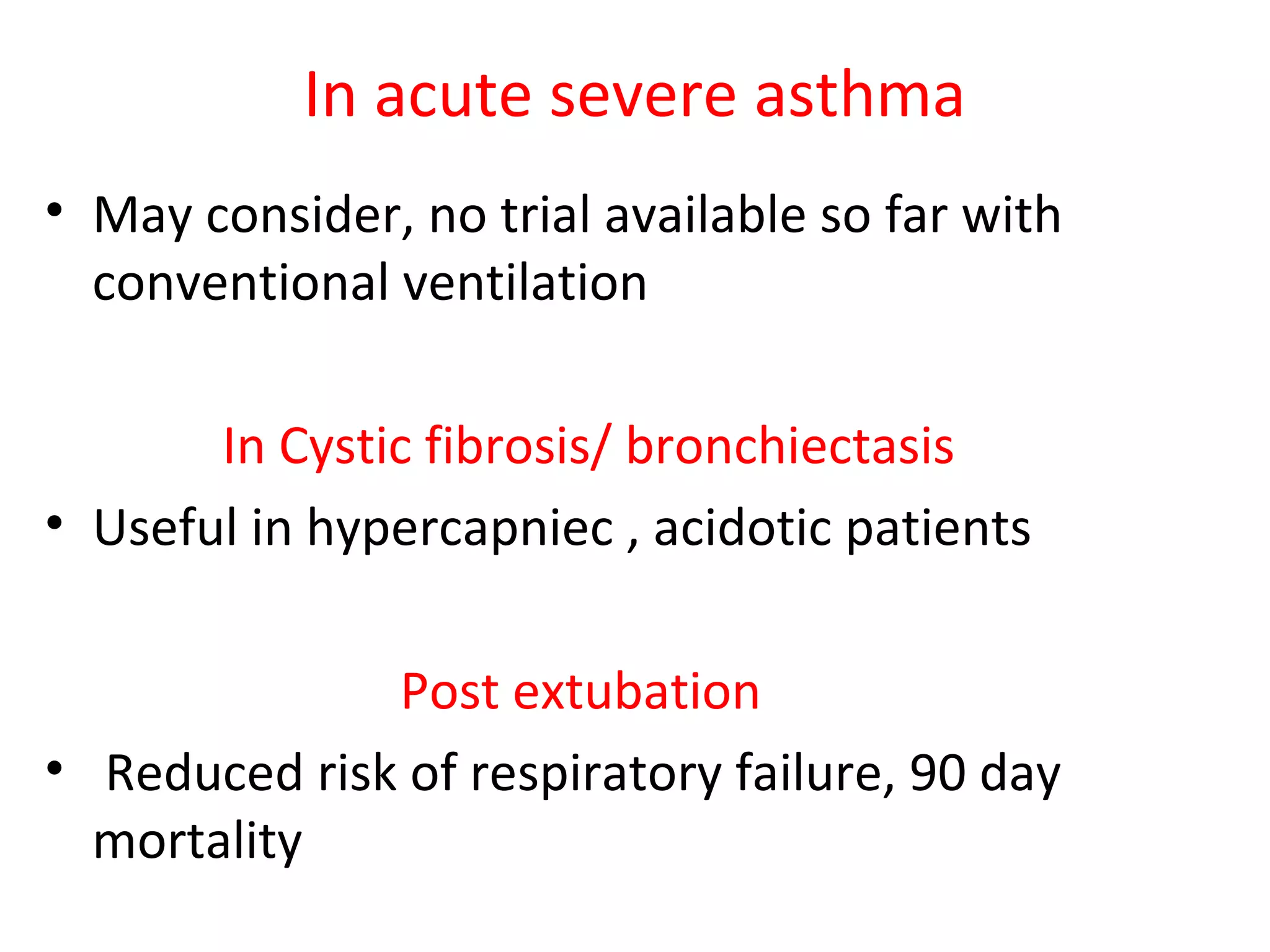
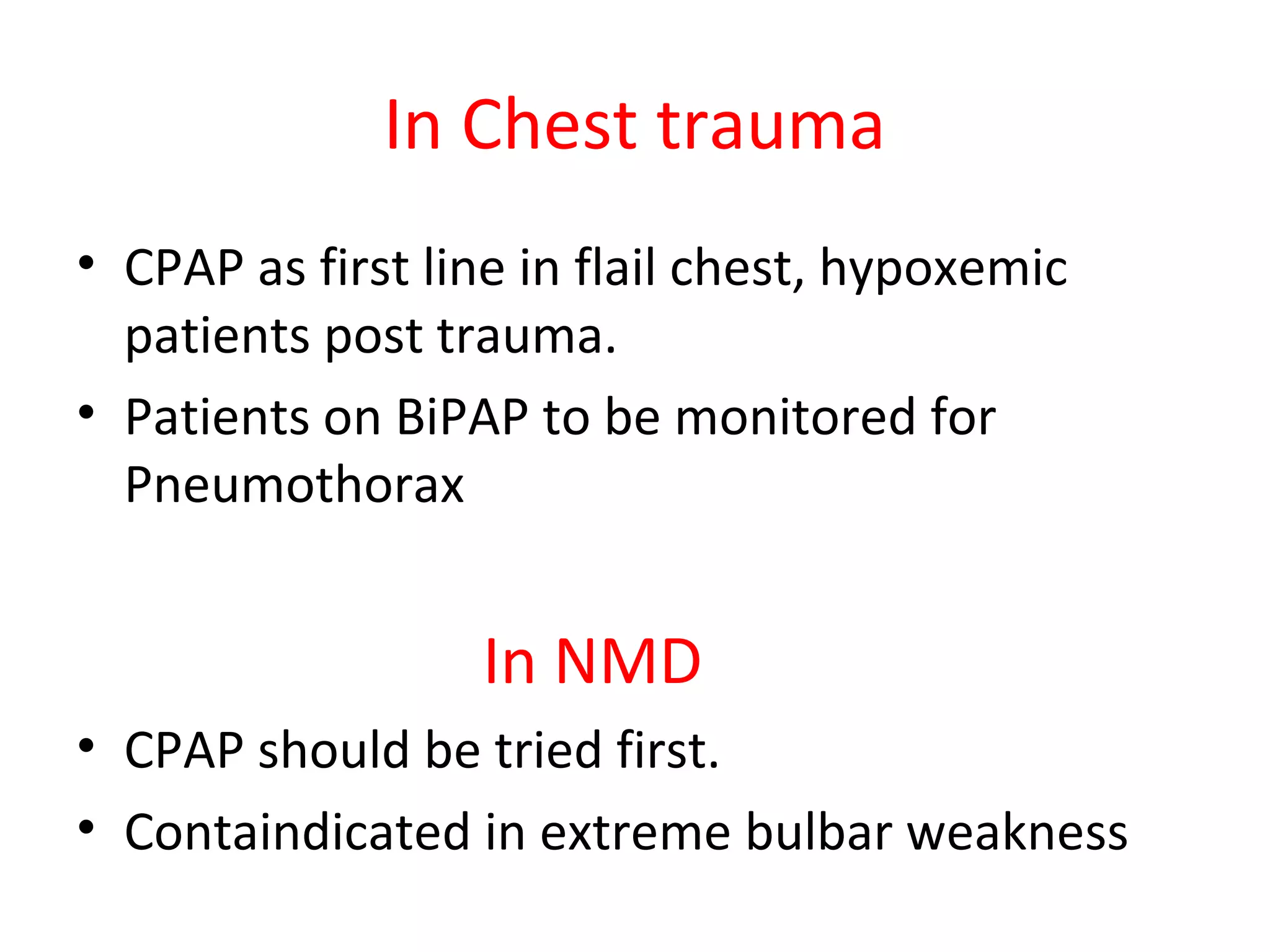
This document provides information on non-invasive ventilation (NIV). It discusses the types of NIV including negative pressure ventilation and positive pressure ventilation. The advantages of NIV include avoiding complications of intubation, ease of application and removal, intermittent use, use in non-ICU settings, improved comfort, and preservation of speech and swallowing. NIV can be used for conditions like COPD exacerbations, cardiac pulmonary edema, and immunocompromised patients. Settings and protocols for initiating and monitoring NIV are outlined. Troubleshooting tips are provided for issues like low oxygen levels or high carbon dioxide levels.