immunology.pdf immunity immune system mechanisms
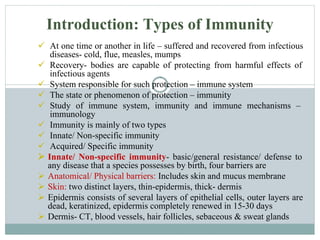
- 1. At one time or another in life – suffered and recovered from infectious diseases- cold, flue, measles, mumps Recovery- bodies are capable of protecting from harmful effects of infectious agents System responsible for such protection – immune system The state or phenomenon of protection – immunity Study of immune system, immunity and immune mechanisms – immunology Immunity is mainly of two types Innate/ Non-specific immunity Acquired/ Specific immunity Innate/ Non-specific immunity- basic/general resistance/ defense to any disease that a species possesses by birth, four barriers are Anatomical/ Physical barriers: Includes skin and mucus membrane Skin: two distinct layers, thin-epidermis, thick- dermis Epidermis consists of several layers of epithelial cells, outer layers are dead, keratinized, epidermis completely renewed in 15-30 days Dermis- CT, blood vessels, hair follicles, sebaceous & sweat glands Introduction: Types of Immunity
- 2. Skin is the first line of defense, prevents the entry of pathogens in to deeper tissues, low pH inhibit their growth as well Sebaceous glands- sebum, lactic acids & fatty acids- maintain low pH of skin between 3 to 5 – prevents the growth of most of the pathogenic bacteria Any wound, abrasions in intact skin leads to the entry of pathogens Mucus Membrane: Conjunctiva, GIT, RT, urogenital tract protected by mm, consist of outer epithelial layer and CT Saliva, tears, mucus secreted by epithelial cells contains antibacterial & antiviral substances- protects from pathogens Cilia in RT traps and propels microorganisms Microorganisms have evolved their own defense mechanisms Fimbriae or pilli on Neisseria gonorrhoeae interact with glycoprotein & glycolipid receptors on epithelial cells of mm Physiological Barriers: includes Temperature pH and soluble factors Temperature: Many species are not susceptible to diseases- because of their body temperature e.g. chicken displays natural immunity to Anthrax – 1070F pH: Gastric acidity – innate barrier as pathogenic bacteria grow at neutral pH New born more susceptible- stomach contents are less acidic, gastric flora has not been fully established
- 3. Soluble factors: also contribute to non-specific immunity Lysozyme: a hydrolytic enzyme in mucus secretions – cleave peptidoglycan of bacterial cell wall Interferons: group of antiviral proteins produced by virus infected cells Complement: group of heat labile serum proteins- inactive pro-enzyme form Upon activation- destroy pathogens, help them clear from the body Endocytic/ Phagocytic barriers: ingestion of extracellular macromolecules and particles through endocytosis, phagocytosis Endocytosis- receptor mediated endocytosis or pinocytosis, Phagocytosis- ingestion of particulate material including whole microorganisms Break down into simpler products and eliminated from the cell Barriers created by inflammatory response: Tissue damage caused by wounds or invasion by pathogenic microorganisms or by variety of agents/ substances like drugs, pollens, inert physical materials such as wood, pieces of metals etc. can induce a complex sequence of events- inflammation In 1st century AD- Roman Physician Celsus- four cardinal signs of inflammation- rubor (redness), tumor (swelling), calor (heat), dolor (pain)- In 2nd century AD Galen added 5th sign- functio laesa (loss of function) Inflammation- useful process, results in clearance of pathogen followed by tissue repair & regeneration
- 4. Acquired or specific immunity: Reflects the presence of functional immune system capable of specifically recognizing and selectively eliminating the pathogens Four features- specificity, diversity, memory, self/non-self recognition Developed after birth during life time, may be acquired actively or passively Active immunity: When an individual is exposed to microorganisms/ foreign substances- immune system responds- usually long lived Passive immunity: Through the transfer of antibodies- usually short lived Both types may be acquired either through natural or artificial means Naturally acquired immunity: Its is of further two types Naturally acquired active immunity: Person is exposed to an Ag in daily life/ disease It may be life long in some disease, for few years, sub-clinical infections- immunity Naturally acquired passive immunity: Transfer of maternal antibodies Trans placental transfer- from placenta to fetus before birth- IgG e.g. if mother is immune to rubella, polio, diphtheria- new born will also be temporarily immune, Clostrum after birth- rich in IgA, in poultry through egg yolk- IgG, amniotic fluid- IgA In mammals e.g. calf, now trans placental transfer, clostrum is the only source, FCS is free of maternal Abs- used in research
- 5. Artificially acquired immunity: Its is of further two types Artificially acquired active immunity: Through vaccination/ immunization, same mechanism as pathogens but no disease Vaccine- live attenuated or inactivated bacterial/ viral- polio vaccine, tetanus toxoids etc. Artificially acquired passive immunity: Through introduction of already prepared purified antibodies Immediate immunity- short lived, Abs neutralizes Ag- catabolized Half life is usually up to 3 w, ATS 14-21 days Abs- serum, antiserum is used, study of serum, Ag-Ab interactions- serology Electrophoresis- two types of serum proteins, albumin & globulins Globulins- further three types- Alpha, Beta & gamma Gamma-globulins- Immunoglobulins (Igs)- Abs Five classes- IgG, IgM, IgA, IgD and IgE
- 6. Immune system – structurally & functionally diverse cells, tissues & organs- throughout the body Immune/ lymphoid organs – 1. Primary 2. Secondary Primary- appropriate micro-environment- maturation of lymphocytes Secondary- trap Ag from tissue & vascular spaces- site for interaction of mature lymphocytes with Ag Central cells of immune system- lymphocytes- 25% of WBCs in blood and 99% of lymph Approximately 1012 in human = brain + liver Cells of Immune System Lymphocytes: Only possesses the four attributes, central cells, all other cells play accessory role- activation of lymphocytes, phagocytosis, secretion of immune effector molecules like cytokines 20-40% of WBCs, circulate in blood, lymph, migrate to tissue spaces and lymphoid organs- lymphocytes re-circulation Three types- function and cell membrane components- B-cells/ B-lymphocytes, T- cells/ T-lymphocytes, Null cells All three types- small (6µm diameter), motile, phagocytic cells- Indistinguishable morphologically B/T-cells- not interacted with Ag- naïve, virgin, un-primed cells- in Go phase of cell cycle, if don’t interact with Ag- die apoptosis (short life span-few days to few weeks) Cells of Immune System
- 7. Interaction of B/T cell with Ag- enter in to cell cycle from Go to G1 (early & late gene activation stage)- S-stage (lymphoblast stage- 15µm), S-synthesis of DNA, finally M-division stage- proliferate & differentiate into effector cells & memory cells Effector cells- short life span, B-cell lineage- plasma cells (Ab secreting cells) T-cell lineage- TH cells and CTL-cytotoxic T lymphocytes Memory cells- long lived cells- Go phase- activated with second encounter of same Ag B-lymphocytes: name- site of maturation, bone marrow in mammals & bursa of Fabricus in birds Distinguished from the BCR- membrane bounded Immunoglobulins (Abs)- serve as receptor for Ag, B-220- first marker of B-cell lineage Express class-II MHC molecule – as antigen presenting cells APC Interaction Ag and BCR- a naïve B-cell together with T-cell & macrophages- activated and divides in to plasma & memory cells, plasma cells lack membrane bounded Igs – secrete one of the five classes of Igs (Abs)- neutralizes Ag- Humoral immune response T-lymphocytes: name- site of maturation, thymus, have TCR- not membrane bound Immunoglobulins, protein receptors which recognize an Ag only when presented along with MHC molecule- MHC- restriction Fundamental difference- humoral & cell mediated branches of immunity
- 8. The earliest marker of T-cell lineage – Thy-1, appear during maturation in thymus & then remains throughout life span Two sub-populations of T-cells- T-cells that express CD4 receptors (cluster of differentiation) – recognize Ag associated with MHC-II called CD4+ or TH cells- MHC-II restricted T-cells that express CD8 receptors – recognize Ag associated with MHC-I called CD8+ or TC cells- MHC-I restricted TH cells proliferate extensively- recognition of Ag-Class-II MHC complex on APC- secrete many cytokines- activate B-cells, converted to plasma & memory cells, plasma cells secrete Abs- humoral immune response TC cells activated- interaction with Ag-Class-I MHC complex on the surface of self cells (virus infected cell)- generate CTLs which mediate killing of self/ target cells- CMI Ration of CD4+ : CD8+ cells is 2:1in normal peripheral blood, may be altered in immunodeficiency or auto-immune diseases Null cells: Neither have TCR or BCR- lack four attributes One functional population – NK cells, large, granulated, 5-10% of peripheral blood lymphocytes, play important role in defense against tumor cells Interact with tumor cells in two ways: Direct contact in non-specific Ab independent process, Specific Ab-dependent cell mediated cytotoxicity
- 11. Mononuclear Cells: include circulating monocytes- blood & macrophages- tissues Monocyte- macrophage- number of changes 5-10 fold increase in size, intracellular organelles- increase in number & complexity, cell acquires more phagocytic ability, produces more hydrolytic enzymes and secrete more soluble factors Macrophages: two types 1. Fixed macrophages: Takes residence in a particular tissues and named accordingly Liver- Kupffer cells, CT- histocytes, Lungs- alveoler macrophages, Kidney- mesangeal cells, Brain- microglial cells 2. Free/ wandering macrophages- move through amoeboid movement throughout the tissues Phagocytosis- ingesting exogenous Ag, insoluble particles, injured & dead cells of host, cellular debris, activated clotting factors etc. Granulocytes: three types on the basis of cellular morphology & cytoplasmic staining characteristics Neutrophils: produced in bone marrow- hematopoiesis Granulated cytoplasm- stained with both acidic & basic dyes Polymorphonulear leukocytes- multilobed nuclei Released in peripheral blood circulation- 7-10 hours, migrate in to tissues- 3 days life span First line of defense against infections, first cells to reach at inflammation site Neutrophilia – acute infection, Phagocytic activity is more than macrophages Cells of Immune System
- 12. Eosinophils: Biolobed nucleus, granulated cytoplasm- stained with acidic dye- eosin Y Motile, phagocytic, can move from blood to tissues, Phagocytic role- less than macrophages Play major role in defense against parasites- eosinophilic cytoplasmic granules - secrete certain substances- damage parasite membrane Basophils: Single lobed nucleus, granulated cytoplasm- stained with basic dye- methylene blue. Non-phagocytic Cytoplasmic granules- secrete- pharmacologically active substances, play major role in allergic responses Migrate in to tissues- mast cells, secrete histamine – development of allergies Dendritic cells: named- covered with long membranous processes- resembling dendrites of nerve cells Express high level of MHC-II- act as APCs help in activation of TH cells, two types Non-lymphoid dendritic cells: found in tissues other than lymphoid, named accordingly, Langerhans cells- epidermis, interstitial cells- heart, liver, kidney, GIT etc. capture Ag from tissues spaces- regional lymph nodes Lymphoid dendritic cells: interdigitating dendritic cells- found in T-cell rich areas of lymphoid organs- spleen, lymph nodes & thymus- act as APCs Follicular dendritic cells- found in lymphoid follicles of lymph nodes- B-cells activation
- 15. Two types- Primary (central) Secondary (Peripheral) Immature lymphocytes- hematopoiesis become mature and Ag committed within primary lymphoid organs In mammals Bone marrow- B-cell maturation and Thymus- T-cell maturation, in birds Bursa of Fabricus- B-cell maturation as no bone marrow Secondary organs trap Ag from tissue & vascular spaces- provide a site where mature immunocompetent lymphocytes can interact with Ag to generate an immune response Main secondary lymphoid organs are Lymph Nodes and Spleen GIT, RT possesses MALT including Peyer’s patches, tonsils, adenoids, appendix- mucosal immunity Primary Lymphoid Organs: Thymus: flat, bilobed organ-situated above the heart Each lobe surrounded by fibrous tissue capsule send projections of CT- trabaculae, divide each lobe into smaller lobules Outer portion of each lobe- cortex- densely packed with thymocytes (immature T-cells) Inner portion medulla- sparsely packed with thymocytes Both cortex and medulla cris-crossed with three dimensional network of thymic stromal cells composed of epithelial cells, interdigitating dendritic cells, macrophages- make up the framework of thymus and help in maturation of T-cells Cortical epithelial cells (nurse cells) have long membranous processes- hold as many as 50 thymocytes Organs of Immune System
- 16. Function: Maturation & selection of T-cells- Epithelial cells secrete many hormones and cytokines (alpha 1 thymosin, beta 4 thymosin, thymopoeitin, thymulin) Maturation, proliferation and differentiation of T-cells Express Ag binding receptors, differentiate in to sub-populations Selection process: two types Positive selection and negative selection T-cells bearing receptors that can recognize self MHC molecule are selected and other are eliminated through apoptosis Self reactive T-cells- recognize self MHC with self Ag are eliminated Both as a result of positive and negative selection only those mature T-cells whose TCR can recognize self MHC molecule along with foreign Ag are selected and allowed to move into secondary lymphoid organs About 95-99% thymocytes die through apoptosis Bone marrow: Site of maturation of B-cells in mammals, Bursa of Fabricus in birds Process of B-cells maturation remains unknown
- 19. Secondary Lymphoid Organs Lymph Nodes: encapsulated bean-shaped structures containing reticular network- packed with lymphocytes, macrophages and dendritic cells Clustered at the junction of lymphatic vessels, first organized lymphoid structure to encounter Ag that enters in to tissue spaces Divided into three regions: Cortex, Para-cortex and Medulla Cortex: Outermost region contains Lymphocytes (B-cells) and macrophages arranged in Primary follicles, B- cell rich area/ thymus independent area Following Antigenic challenge- enlarges in to secondary follicles with germinal center Intense B-cell maturation and differentiation into plasma and memory cells occurs in germinal center In childeren with B-cells deficiency cortex lacks primary follicles and germinal centers Para-cortex: situated beneath cortex, contains T-cells and dendritic cells Dendritic cells express MHC-II molecule and act as APCs for TH, Para-cortex- T-cell rich area/ thymus dependent area Medulla: Inner most portion, sparsely packed with lymphocytes, mostly plasma cells actively secreting Abs Function: Ag carried to LN by lymph to Para-cortex, trapped, processed and presented along with MHC-II by dendritic cells- resulting in TH activation which activates B-cells Ag activated TH cells, B-cells moves to primary follicles of cortex, interaction between follicular dendritic cells, B-cells, TH cells- development of secondary follicle and germinal center B-cells- plasma and memory cells, plasma cells move to medulla where secrete Abs Multiple Afferent Lymphatic vessels pierce capsule of LN and empty lymph in sub-capsular sinuses, single efferent vessel drains lymph away from LN- contains high conc. of Abs & 50 fold more lymphocytes Blood supply to LN- lymphatic artery, drainage lymphatic vein, extravasation of lymphocytes at the level of Post-capillary venuoles Organs of Immune System
- 23. Spleen: Large, ovoid organ, left side of abdominal cavity, Unlike LN which trap localized Ag from regional tissue spaces, spleen- adopted to filter blood and trap blood born Ags and thus respond to systemic infections Surrounded by capsule- send trabaculae which divides in to compartments, two compartments red pulp and white pulp separated by marginal zone Red Pulp: consists of network of sinusoids filled with RBCs and macrophages Dead and defective RBCs are destroyed in it- graveyard of RBCs White Pulp: contains peri-arteoler lymphatic sheath (PALS) around the splenic artery mainly composed of T-lymphocytes, Around the PALS, marginal zone rich in B-cells organized in primary follicles Upon Ag challenge primary follicle develop in to secondary follicle containing germinal center Unlike LN, no lymphatic supply, blood born Ags are carried to spleen through splenic artery which empties in to marginal zone Ag from marginal zone is trapped by dendritic cells- carries it to PALS, where TH are activated, which then activates B-cells converted in memory and plasma cells Abs are carried by splenic vein in to the circulation where it interact with Ag- humoral immunity Mucosal-associated lymphoid tissues (MALT): Mucus membranes lining GIT, RT, urogenital tracts- 400m2 area, protected by MALT Tonsils: lingual- at the base of tongue, palatine- at the side of the tongue, naso-pharangeal (adenoids)- nasopharynx Payer’s patches- 30 to 40 nodules along the outer wall of intestine, BALT, RALT, NALT
- 25. S U B S T A N C E S C A P A B L E O F I N D U C I N G A S P E C I F I C I M M U N E R E S P O N S E F O U R I M M U N O L O G I C A L P R O P E R T I E S Immunogenicity Antigenicity Allerogenicity Tolerogenicity F O R P R O T E C T I O N A G A I N S T D I S E A S E S – I M M U N O G E N P R O P E R T I E S O F A N A N T I G E N Foreignness Molecular weight – 100,000 Da good, < 5000-10,000 Da poor Chemical composition – Protein best followed by polysaccharides, lipids & NA are not alone Complexity Recipient genotype, dose and route of administration ANTIGENS
- 26. Adjuvants – Latin word adjuvare – to help Definition – Not immunogen by themselves, tends to increase the immunogenicity Examples: Alum, Freund’s incomplete & complete, Liposome & ISCOMs Used when, low immunogenicity, costly Epitopes Haptens Mitogens: Induce cell division in B and T lymphocytes irrespective of their antigenic specificity Polyclonal activators B-cell mitogens T-cell mitogens Both Lectins, super-antigens
- 27. A N T I B O D I E S : A N T I G E N B I N D I N G P R O T E I N S Membrane bounded – B-cells as receptors Secreted by plasma cells Effector molecules of humoral immunity - serum Structure: Monomer, Y-shape, 2 heavy & 2 light chains Disulfide bonds, Flexible – T-shape, hinge region Variable region of heavy & light chain on upper ends of Y- arms Constant region of heavy & light chain on stem and lower ends of Y-arms Fab and crystalizable fragment, Amino and carboxylic terminals Epitopes: Antigenic determinants on Abs – 3 types Isotypic, idiotypic and allotypic Immunoglobulins: Structure & Function
- 28. Classes of Immunoglobulins: Function Five classes/ isotypes of Igs: IgG, IgM, IgA, IgD and IgE IgG, IgD and IgE – Monomer, IgA – Dimer, IgM – Pentamer IgG: Most abundant, 80% of serum, 4 subclasses IgG1 (9mg/ml), IgG2 (3mg/ml), IgG3 (1mg/ml), IgG4 (0.5mg/ml) Monomer, can cross the blood vessels and placenta, protects fetus Protect against circulating bacteria & viruses, neutralize toxins Trigger complement system, enhances the effectiveness of phagocytic cells IgM: Pentamer, 5-10% of serum Monomer as receptor on B-cells, Pentamer when secreted by plasma cells Ist Ig produced in response to Ag Ist Ig synthesized by neonate
- 29. Move less freely, remain in blood Strong activator of complement than IgG Enhances phagocytic activity IgA: 10-15% of serum, major secretary Igs (milk, saliva, tears, mucus) Blood – mostly monomer, may be dimer, trimer or tetramer External secretions- always dimer (J-chain & secretary component) Mucosal immunity, clostrum – GIT pathogens IgD: 0.2%, similar to IgG No known function in serum, receptor on B-cells IgE: 0.002%, slightly larger than IgG Binds by Fc portion to basophiles & mast cells Pollens react – histamine & other chemical mediators release Allergic responses and defense against parasites
- 30. TCR are MHC restricted, CD4 cells are MHC-II, CD8 cells are MHC-I restricted Antigen presenting cells (APCs), synthesize & express MHC-II and present the processed Antigenic peptide to CD4 cells Self cells: synthesize & express MHC-I and present Antigenic peptide to CD8 cells APCs: Monocytes, macrophages, B-cells, dendritic cells, Langerhans cells, thymic dendritic cells, epithelial cells, venular endothelial cells Antigen Processing: Extracellular pathogens – exogenous Ag Intracellular pathogens – endogenous Ag, posses different challenges Exogenous Ag – processed through endocytic pathway – Ab production Endogenous Ag – processed through cytosolic pathway – CMI Antigen Processing and Presentation
- 31. Endocytic Processing Pathway APCs – internalize Ag through phagocytosis, endocytosis or both Macrophages – phagocytosis, other cells - endocytosis B-cells – receptor mediated endocytosis using BCR Ag processed in to peptides of 13-18 residues Three compartments: early endosome (pH 6-6.5), late endosome/ endolysosome (pH 5-6) and late lysosome (pH 4.5-5) Acid dependent hydrolytic enzymes in each compartments: proteases, nucleases, lipases, glycosidases, phospholipases, phosphatases Two school of thoughts 1-3 hours – from entry till the appearance of processed peptide in cleft of MHC-II on the surface of same APC
- 32. Cytosolic Processing Pathway Endogenous Ag/ Virus – self cells, processed through cytosolic pathway Degraded in to peptide of 8-9 residues Presented by MHC-I to TC cells – activate CTLs - CMI Cytosolic proteolytic system: Ag binds with carrier proteins “ubiquitin” carried to proteosome Large cylindrical particles containing four subunits with a central hollow of 10-20Ao Degradation of Ag inside prevents the proteolysis of other proteins in side cytoplasm Low Molecular mass proteins (LMP)- alternate to Cytosolic proteolytic system
- 33. Antigen Presentation Assembly & Stabilization: Processed peptides fit in to the cleft of MHC-I & MHC-II Both are synthesized within RER MHC-II: Two chains - alpha & beta – make cleft together MHC-I: Two chains – large alpha make cleft & small beta2 microglobulin stabilizes it Assembly of antigenic peptide processed through cytosolic pathway in to the cleft of MHC-I takes place within RER – Ag moves to RER It may misfit in to MHC-II – Occupied by third invariant chain MHC-II moves from RER to Lysosome – invariant chain degraded by enzymes and Antigen fit in to the cleft of MHC-II MHC-II & MHC-I along with processed Ag is displayed on the surface of APCs & Self cell, respectively – presented to CD4 & CD8 cells for humoral & CMI, respectively Clinical Applications: For the design of new vaccines, to understand the mechanism & treatment of certain autoimmune diseases
- 34. Used in two ways: either for detection of Ag or Ab if one of them is known Highly specific, measurement of Ag or Ab – Serology Three categories: Primary, Secondary & Tertiary binding tests Primary: ELISA, RIA, IFA/FAT Secondary: Precipitation & Agglutination tests, CFT Tertiary: Neutralization & Protection tests Reagents required: Serum, -200C, heat inactivation at 560C in water bath Complement: group of heat labile serum proteins, source guinaea pig serum Antiglobulins: Anti-Ab, Anti-species Ab, Anti-isotypic Ab Monoclonal Ab: highly specific & pure Antigen-Antibody Interactions/ Immunodiagnostics
- 35. Primary Binding Tests Direct: for detection of Ag with known Ab Indirect: for detection of Ab with known Ag Named on the basis of Indicator system used Radio-immunoassays (RIA): Radioisotopes are used as indicator like 3H, C14, I125 RIA for Ab/ Indirect: Known Ag is impregnated to nitrocellulose filter paper Unknown serum sample added and incubated Radiolabeled Anti-Ab are added and radioactivity is observed under X-ray film RIA for Ag/ Direct or Competitive RIA: Unlabeled Ag will displace radiolabeled Ag from immune-complexes Known Ab and Radiolabeled Ag are added in test tube, incubated, radioactivity of supernatant is observed Unknown Ag/ sample is added, it will replace the radiolabeled Ag which will come in supernatant showing radioactivity Amount of radioactivity is directly proportional to Ag present in sample Highly sensitive, qualitative as well as quantitative but costly and not safe
- 36. Immunofluorescence assays (IFA): Fluorochromes/ fluorescent dyes are used as indicator like FITC, RITC, Oramine etc. FITC yellow color compound – UV invisible – fluoresce with bright green color Direct FAT for Ag: Unknown Ag/ sample is attached on to nitrocellulose paper Known Ab conjugated with FITC added, incubated and fluorescence is observed under UV invisible or fluorescent microscope Can detect low level of Ag directly from infected body tissues like Negri bodies in rabbied brain Indirect FAT for Ab: Known Ag is attached on to nitrocellulose paper Unknown serum sample is added, incubated Known Anti-Ab conjugated with FITC added, incubated and fluorescence is observed under UV invisible or fluorescent microscope Highly sensitive, qualitative as well as quantitative but costly
- 37. Enzyme immunoassays (EIA): Enzymes along with respective substrates are used as indicator like HRP, Alkaline phosphatase etc. On addition of substrate, color development/ OD value is measured Direct ELISA for Ag: Known Ab is attached on to the surface of ELISA plate wells, washed Unknown Ag/ sample is added, incubated, washed Known Ab conjugated with enzyme is added, incubated Substrate added, OD value is observed through ELISA reader Sandwich ELISA as Ag is sandwiched between two Ab molecules Indirect ELISA for Ab: Known Ag is attached on to the surface of ELISA plate wells, washed Unknown serum sample is added, incubated Known Anti-Ab conjugated with enzyme added, incubated and OD value is observed through ELISA reader Highly sensitive, qualitative as well as quantitative, comparatively economical, safe and most commonly used
- 38. Ag or Ab is detected on the basis of the results of primary reaction Precipitation Tests: Soluble Ag + Ab, mixture cloudy after few minutes, precipitate in 1 hour if +ve Slide and tube precipitation tests Optimum level of both is required for precipitation to occur AGID/ AGPT, Immuno-electrophoresis, CCIE, Western blotting Simple, economical, specific but less sensitive, difficult to read Agglutination Tests: Particulate Ag + Ab – Agglutination/ clumping Simple, economical, more sensitive, easy to read Slide & tube agglutination tests/ macro-agglutination tests Micro-agglutination tests – Haemagglutination tests: HA, HI, IHA etc. Antigen-Antibody Interactions/ Secondary Binding Tests
- 39. Complement Fixation Test Two systems: Test system & Indicator system Major/ Test system: Ag + test serum + complement Minor/ Indicator system Sheep RBCs + Amboceptors If no hemolysis - +ve If hemolysis - -ve Tertiary Binding Tests: Neutralization Test: To test the neutralization ability of Ab against an Ag in-vitro Protection Test: To test the protective ability of Ab against an Ag in-vivo
- 40. Development of effective immune response – lymphoid cells, inflammatory & hematopoietic cells Complex interaction between these cells is mediated by a group of low molecular weight (30KDa) regulatory proteins - cytokines Secreted by WBCs, particularly lymphocytes in response to inducing stimuli Binds to receptors on target cells, signal transduction, biological effect Hormones – messengers of endocrine system, Cytokines – messengers of immune system Cytokines may act in three ways Autocrine: same cell act as cytokine producing & target cell Paracrine: target cell is near by to producing cell Endocrine: binding to target cells in distant part of the body CYTOKINES
- 41. Cytokine may exhibit four properties Pleotropy: Cytokine has biological effect on different target cells – pleotropic e.g. IL-4 Redundancy: Two or more cytokines – same biological effect on single target cell – redundant e.g. IL-2, IL-4, IL-5 Synergy: When combined effect of two or more cytokines is greater than their individual effect – synergism e.g. IL4 + IL-5 Antagonism: Effect of one cytokines is inhibited by the other – antagonistic e.g. IL-4 by IFN-γ Nomenclature: Previously on source of release e.g. lymphocytes – lymphokines, monocytes – monokines Technically incorrect- as monokines and lymphokines also secreted from other cells Now named on the basis of function Interleukins: Cellular communication among leukocytes, IL1 to IL-17... Interferons: Glycoproteins – in response to virus infection – antiviral IFN-α, IFN-β, IFN-γ
- 42. Tumor Necrosis factor: anti-tumor TNF-α, TNF-β Growth factors: Stimulate the growth of many cells, CSF, G-CSF, M- CSF, GM-CSF Transforming Growth factors: TGF-β Chemokines: Inflammation, IL-8 Structure: Proteins, four structural groups I: Four α helix – IL2,3,4,5,6,7,10,11,13, G-CSF, GM-CSF, Interferons II: Long β sheets – TNF-α, β, IL-1, TGF-β III: Both α helix & β sheets: Chemokines, IL-8 IV: Mosaic, mixed structure- IL-12 Discovery & Purification: up to 1960s chromatography Disadvantages: low yield- sub-nanomolar level, less purity Recombinant DNA technology: in 1960 1st compound – cDNA cloning techniques To date genes IL-1 to 13, IFNs, TNF, TGF, LIF, Oncostatin M cloned
- 43. Functions of Cytokines: Main source TH , macrophages, B-cells Development of humoral and cellular immune responses Induction of inflammatory response Regulation of hematopoiesis Control of cellular proliferation & differentiation Induction of wound healing In-vitro diagnostic and in-vivo therapeutic uses Cytokines antagonists: Inhibit the action of cytokines Binds directly to cytokines Binds to their receptors on target cells
- 44. Antibodies produced – purified Ag - Polyclonal Advantages in localization, phagocytosis & complement mediated lysis of Ag Due to undesirable, non-specific, cross-reacting Ab - In-vitro diagnostic and in-vivo therapeutic uses Purified through chromatographic techniques – very difficult Alternate – purified clones of mono-specific plasma cells in-vitro – but short life span Solution by George Kohler & Cesar Milstein in 1975 by fusing B-cells, myeloma cells – hybridoma, Nobel Prize - 1984 Formation & selection of hybrid cells: 1970s two somatic cells fused – heterokaryon, fusion by Sendai virus, PEG Initially 2-5 nuclei, loss of chromosomes until stabilizes Hybridoma and Monoclonal Antibodies
- 45. Selection of hybridoma: HAT medium Denovo pathway: Phosphoribosyl pyrophosphate + uradylate – nucleotide and DNA - blocked by aminopterin Salvage pathway: Hypoxanthine + Thymidine – catalyzed by HGPRT + TK enzymes, only hybrid cell will survive Production of Monoclonal Antibodies: Three steps Generating B-cells hybridoma Screening for Monoclonal antibody specificity Propagating hybridoma secreting specific monoclonal antibodies Ag – mice – Primed B-cells from spleen (HGPRT+, Ig+) + Myeloma cells ((HGPRT-, Ig-, immortal) – PEG – Heterokaryon along with un- fused B-cell and un-fused myeloma cells HAT selection – only B-cells – myeloma cell hybridoma will grow Assay for desired Ab in culture supernatant – ELISA, RIA, FAT Reclone Ab+ hybridoma: Expand in Tissue culture (10-100µg/ml), peritoneal cavity of histocompatable mice (1-25mg/ml), Alginate gel (100 fold more than tissue culture, Fermenter (1000L – 100g in 2w)
- 46. Purification of Proteins: Can purify any protein out of complex mixture, present at extremely low level with 100% purity Previously IFN – chromatographic techniques Disadvantages – 1% purity, 99% impurities DS Secher & DC Burke prepared anti-IFN monoclonal antibodies Fixed on sephadex in an Immuno-adsorbant column Identification and isolation of lymphocytes sub-populations: Monoclonal antibodies can be produced to different membrane bound receptors or proteins – surface of lymphocytes sub- populations CD4+ on TH and CD8+ on TC, anti-CD8 Ab conjugated with FITC and anti-CD4 Ab with PE Identified and isolated in FAC Uses of Monoclonal Antibodies
- 47. Tumor detection and imaging: Tumor specific membrane proteins/ receptors – only on tumor cells Monoclonal Ab are prepared against them – detect tumor Ab are radiolabeled and injected in the body Used to image metastatic tumors Tumor Killing: in two ways Complement mediated lysis: a large no of tumors are resistant Immunotoxins: ricin, shigella & diphtheria toxins – potent toxins Two components: Binding polypeptide & inhibitor chain Binding component is removed & replaced with specific Ab Monoclonal Ab will guide toxic component to tumor cell Safe: will not damage the normal cells Diagnostic Reagents: More than 100 diagnostic agents available Home pregnancy diagnosis using anti-HCG monoclonal Ab coated strips Cancerous T-cells – Thymoma cells
- 48. Immunity – Active and Passive Passive – Natural passive – Maternal Ab (tetanus, mumps, polio, diphtheria), Artificial passive – ATS, anti-snake venom Active – Natural active – disease, Artificial active – immunization/ vaccination Vaccine – Live modified or killed whole or a part of microorganism which when administered in to the body do not cause disease rather elicit a high humoral or CMI As prophylaxis – infectious diseases Whole organism vaccines – bacterial or viral Live attenuated vaccines – viral or bacterial Attenuation – losses pathogenicity, retains immunogenicity Bacillus Calmattee Guerin (BCG)–M. bovis, increased conc. of bile – 13 years – live attenuated vaccine against TB, Polio vaccine – Sabin and Salk strains VACCINES
- 49. Advantages: increased, prolonged immunity, no boosters required Both humoral and CMI Disadvantages: Reversion back to virulence, stability less Contaminants may cause problems, post-vaccination reactions Irreversible attenuation through gene deletion technology, losses immunogenicity along with pathogenicity Inactivated bacterial / viral vaccines: Inactivation - mechanical, chemical Heat – degradation of epitopes, chemical – formaldehyde, BEI, β- propiolactone Advantages: More stable, safe, no reversion back to virulent form Disadvantages: Require booster, short immunity, less CMI more humoral immunity Post-vaccination complications
- 50. Purified Macro-molecules as vaccines: Keeping in view the disadvantages of both Specific surface macromolecules used as vaccine e.g. Capsular LPS as vaccine against meningitis Advantages: more specific, less un toward reactions Disadvantages: activates B-cells directly, no activation of TH cells Poor immunogenic - LPS + Protein carriers e.g. Capsular LPS + Tetanus toxoids – more immunogenic, vaccine against two or more diseases in single shot But difficulty in obtaining purified macromolecules in large quantity
- 51. Recombinant Antigen Vaccine – Most immunogenic Ag is cloned in to an appropriate cloning vector, expressed in an expression host and used as vaccine after purification First ever – FMDV, VPI cDNA – plasmid – E. coli First in human – HBV – gene for Major surface protein – YAC – Yeast cells, used after harvesting and purification Advantages: Specific immune response, no un to ward reaction, minimum post-vaccination complications, safe , stable Disadvantages: Exogenous Ag – only humoral immune response Recombinant Vector Vaccine – Biological vectors are used – attenuated poliovirus, adenovirus, Salmonella, BCG etc. Recombinant vaccinia vector vaccine of small pox Advantages: specific, safe, stable, CMI Disadvantages: Less immunogenic RECOMBINANT VACCINES
- 52. Synthetic peptide vaccine: Most immunogenic peptide is identified Amino acid sequence of highly conserved region is identified which must have Receptors on cell surface Capable of producing neutralizing Ab Influenza – HA sialic acid residues HBV, malaria, diphtheria, HIV in process Multivalent Subunit Vaccine: SMAA - Immunogenic peptide of multiple Ag activating B-cells and T- cells are attached to their Monoclonal Abs fixed on sephadex Liposomes – Ag is incorporated in to lipid vesicles using detergents ISCOMs – Ag is incorporated in to protein miscles Advantages: Better immunogenicity, both humoral and CMI,
- 53. Anti-idiotypic vaccine: Unique a.a. sequence of VH and VL chain of Ab not only act as Ag binding site but also antigenic determinant Ab against VH and VL chain of a specific Ab can be used as vaccine Adjuvants: Freund’s incomplete & Freund’s complete adjuvants Alum adsorbed vaccines, Liposome and ISCOMs Oil adjuvants: surfactants to prepare stable emulsion, Tween 80, Span 80, HLB = 7 Methodology: Isolation, identification, characterization, purification Seed cultivation, attenuation, inactivation Quantification (CFU/ml, PFU/ml) Infectivity testing (LD50/ EID50/ TCID50) Adjuvant, HLB Tests (Safety, stability, sterility, potency/ efficacy) Lyophilization, packing, labeling Marketing