Formation&Development Of Reproductive System
•Download as PPT, PDF•
6 likes•4,115 views
Report
Share
Report
Share
More Related Content
What's hot
What's hot (20)
Development of male and female reproductive system

Development of male and female reproductive system
Genetic development and anatomy of female reproductive organs

Genetic development and anatomy of female reproductive organs
Viewers also liked
Viewers also liked (20)
Development& Various Parts Of Peripheral Nervous System

Development& Various Parts Of Peripheral Nervous System
Similar to Formation&Development Of Reproductive System
Similar to Formation&Development Of Reproductive System (20)
Hormonal control of reproduction in male and female mammals

Hormonal control of reproduction in male and female mammals
More from raj kumar
More from raj kumar (20)
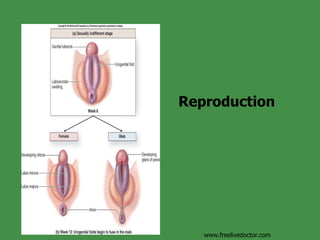
Formation&Development Of Reproductive System
- 13. Development of Accessory Sex Organs and Genitalia www.freelivedoctor.com