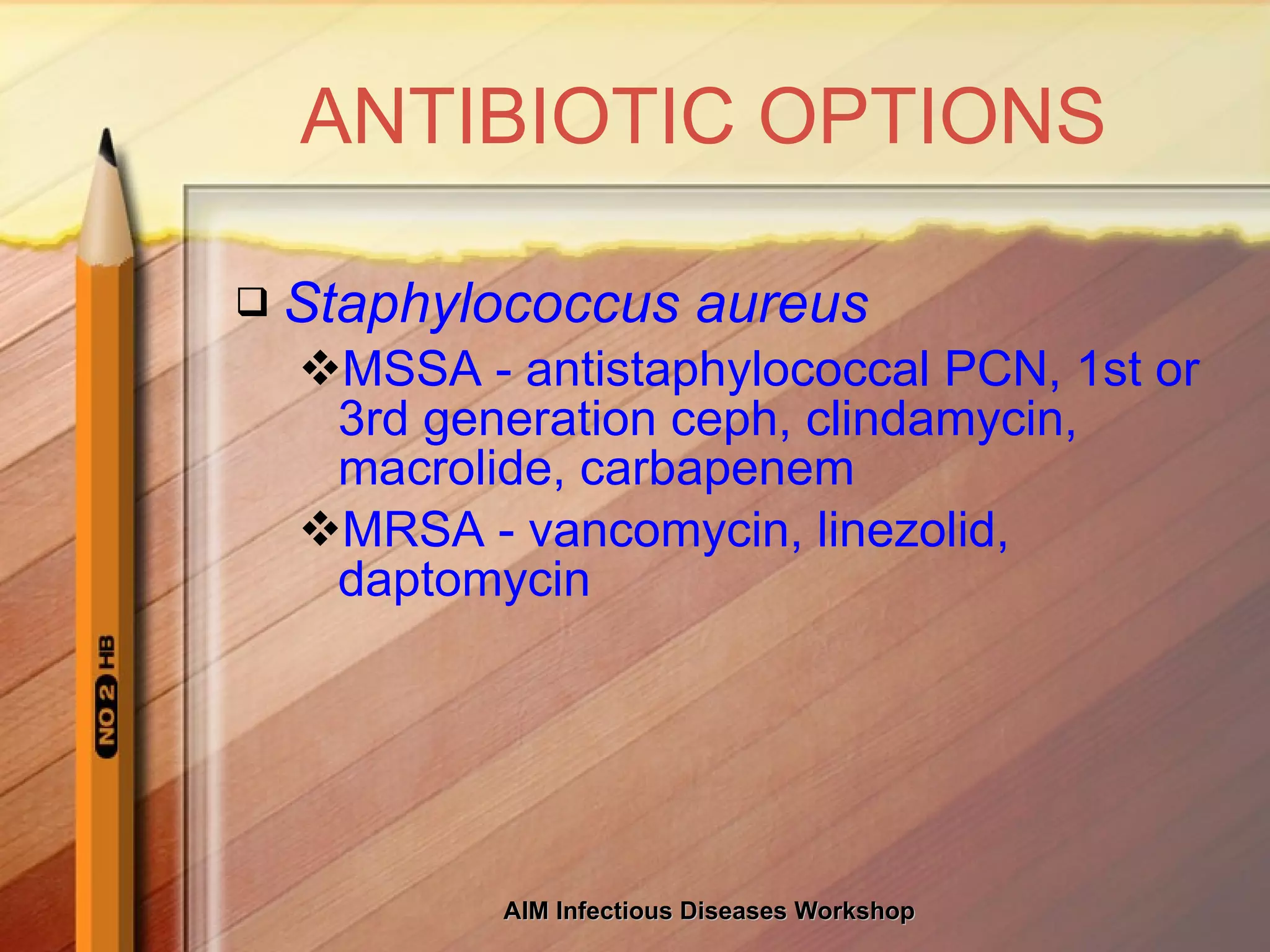
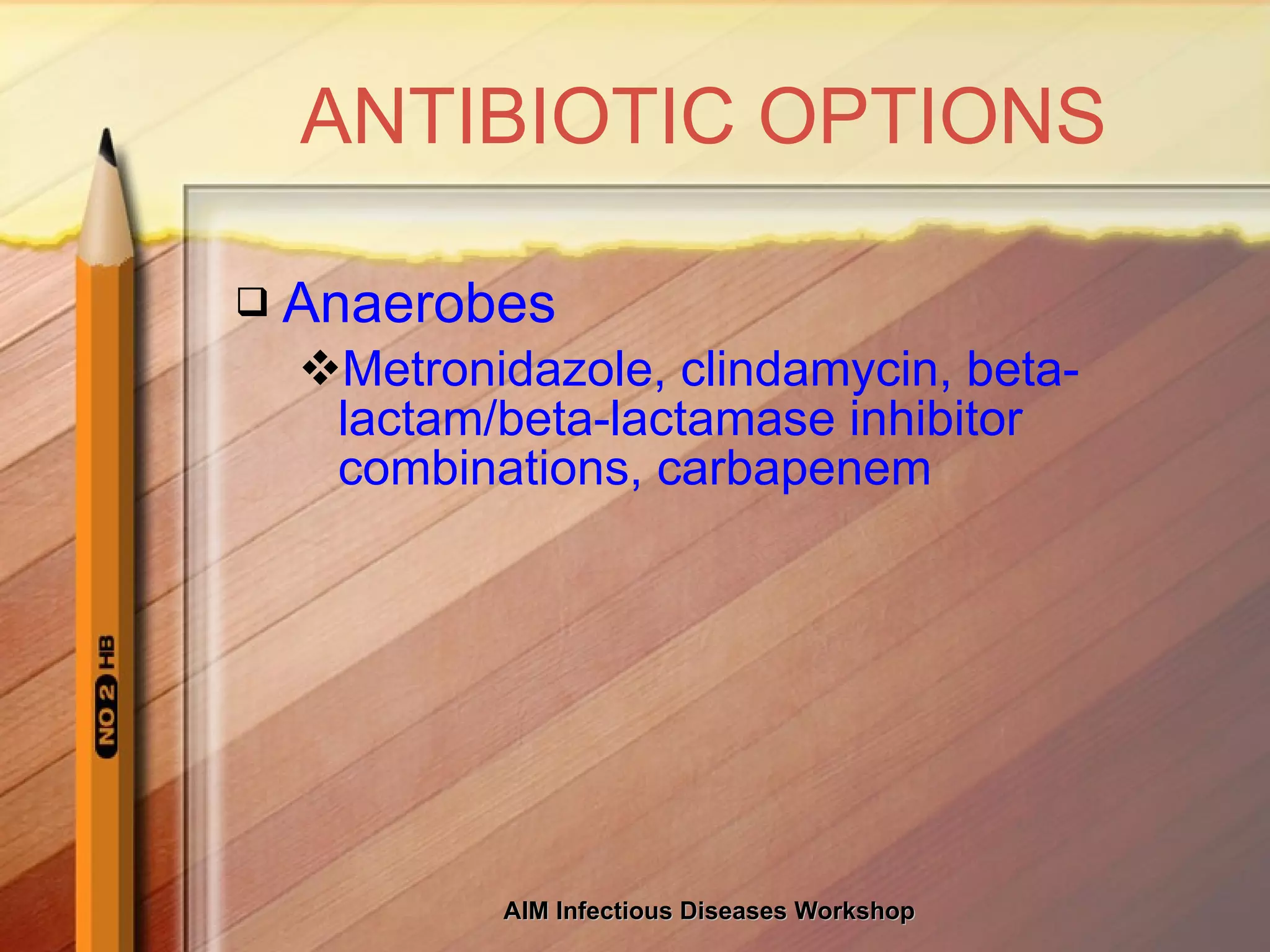
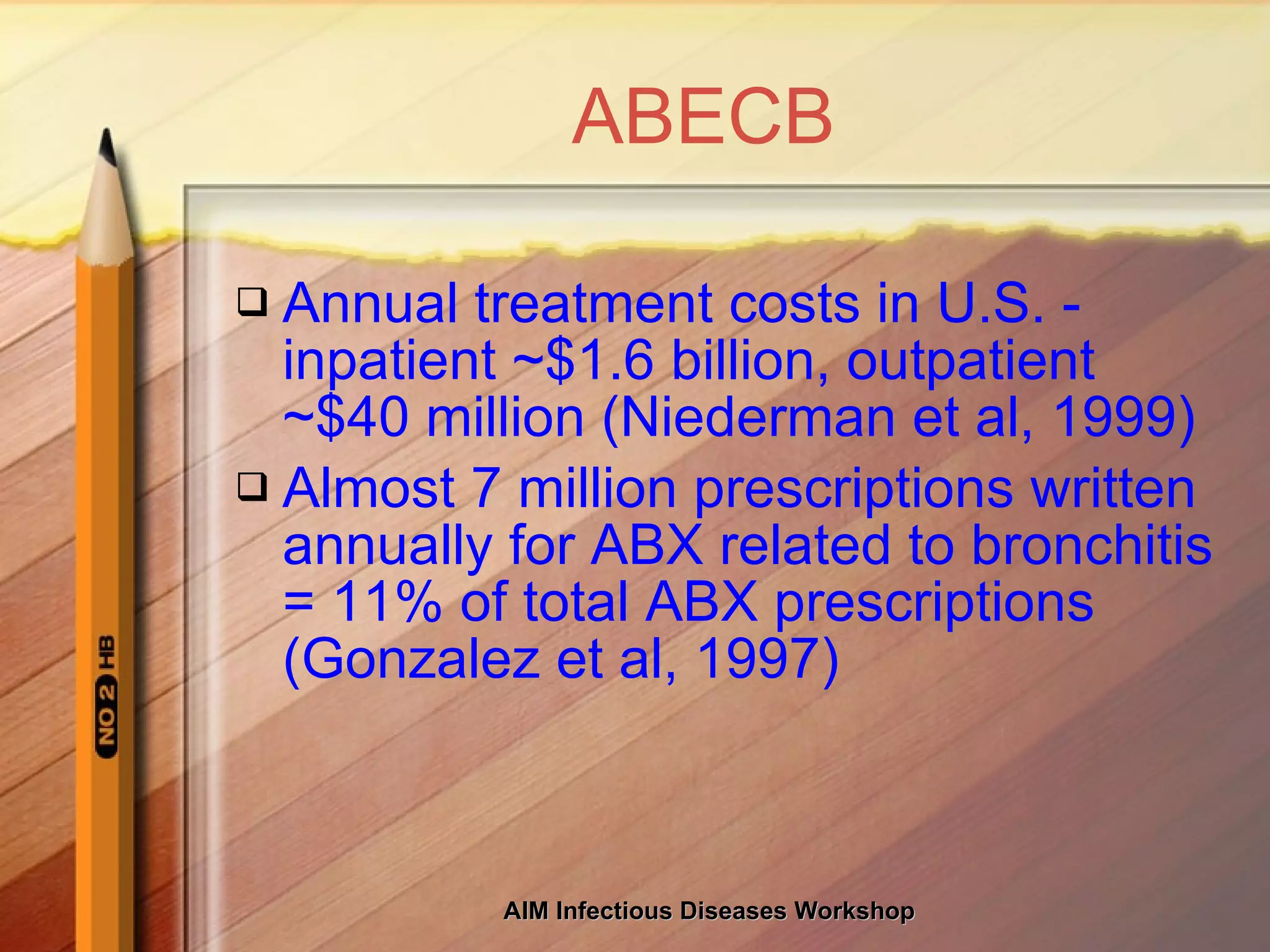
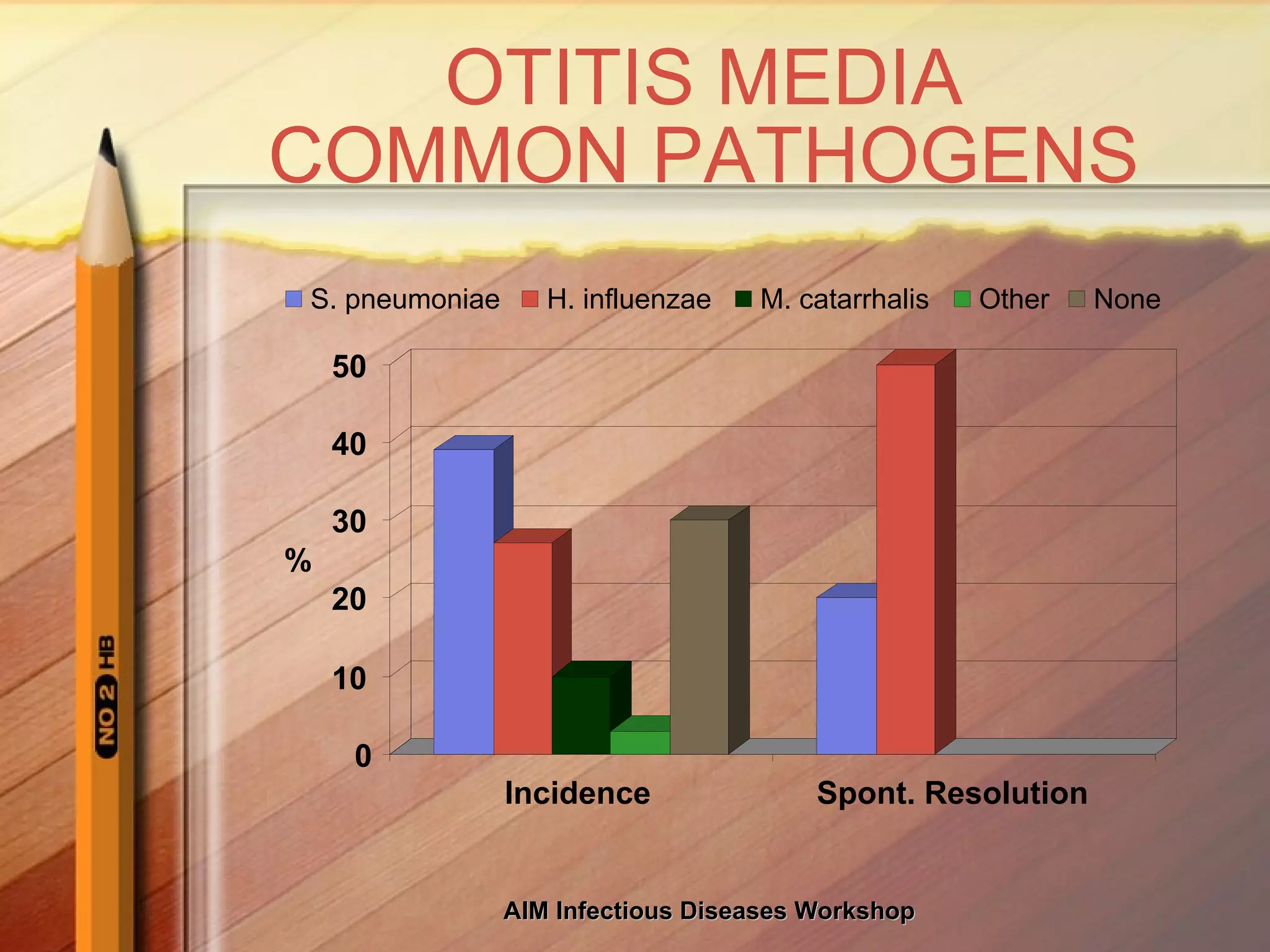
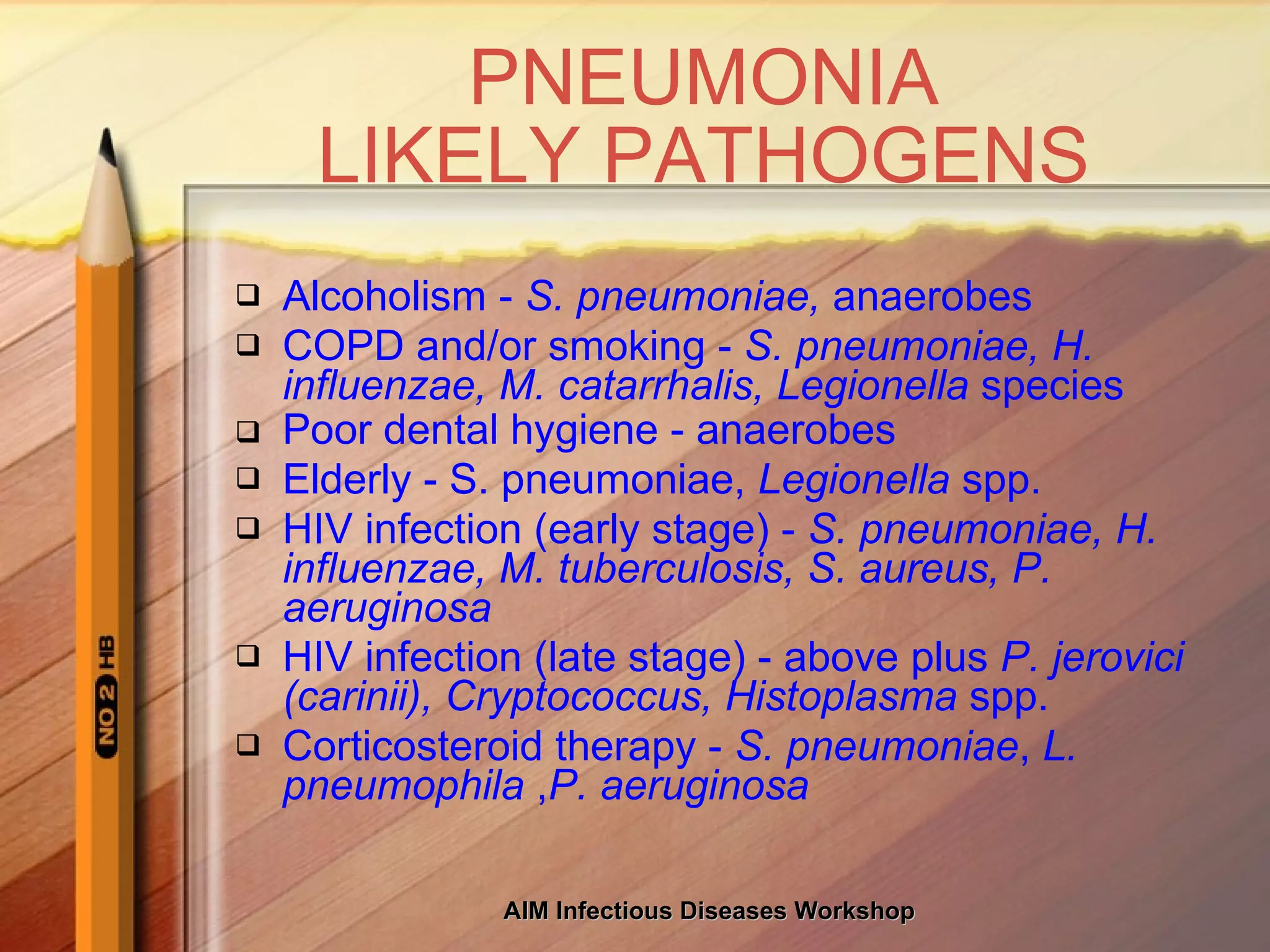
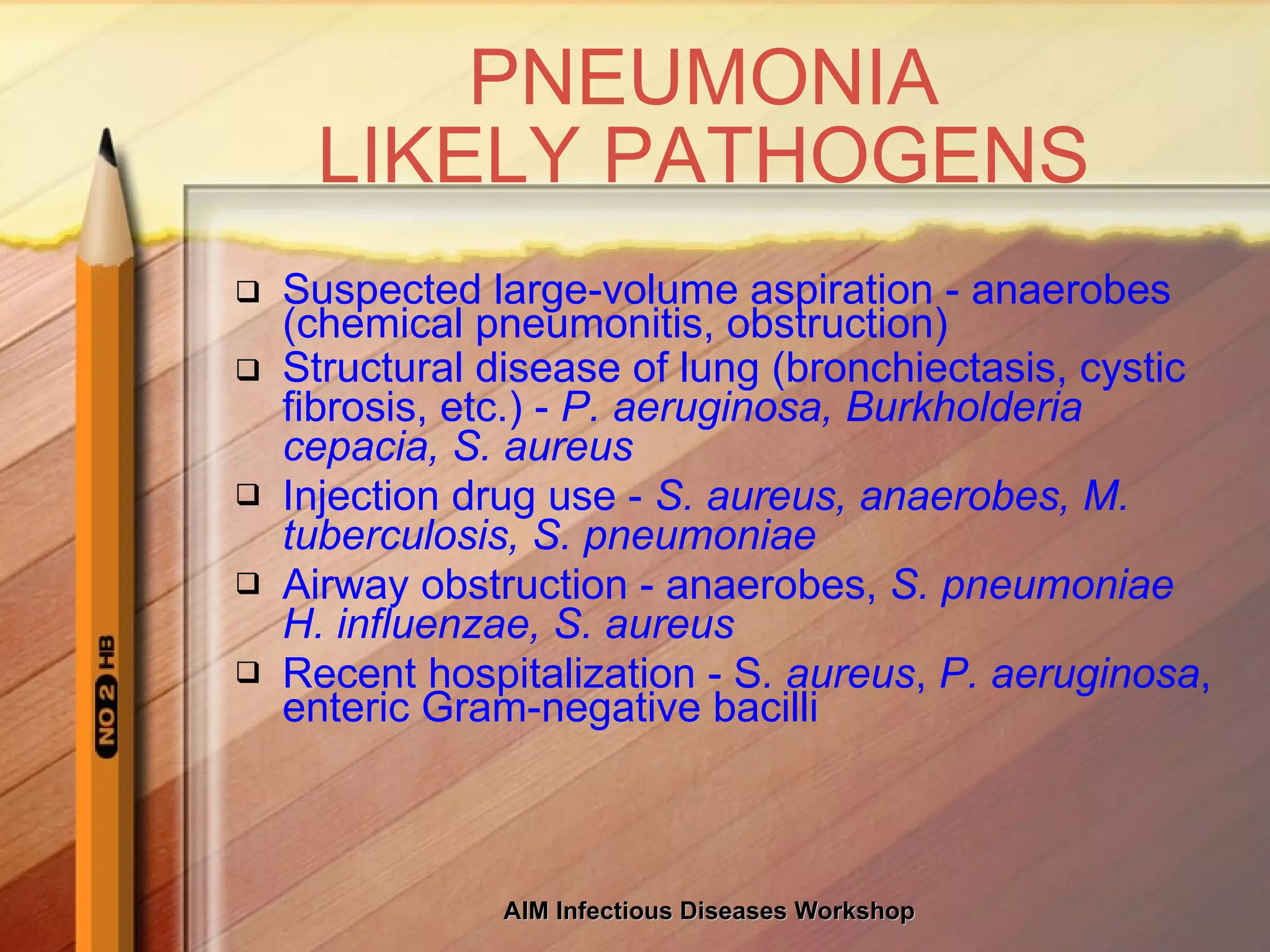
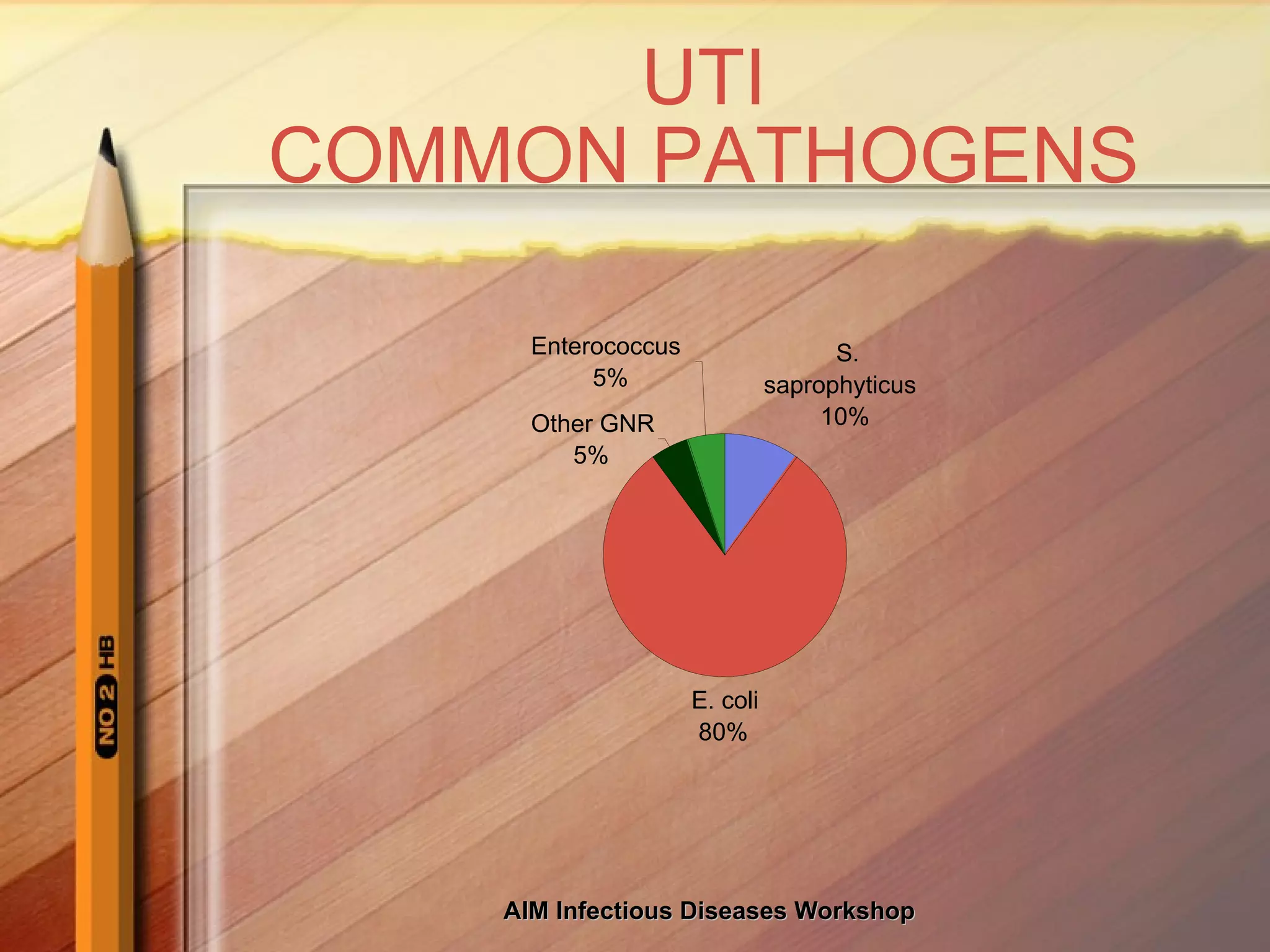
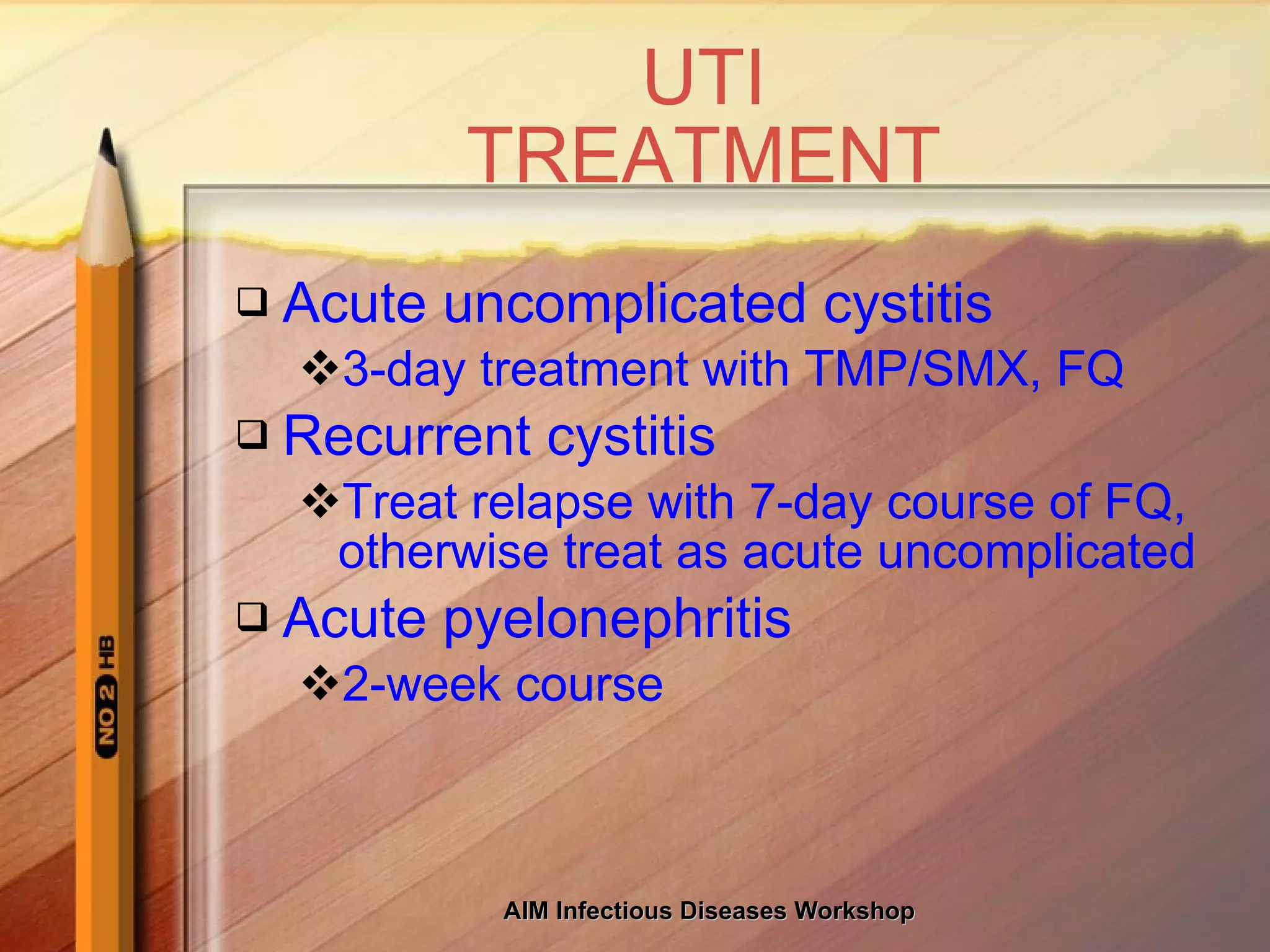
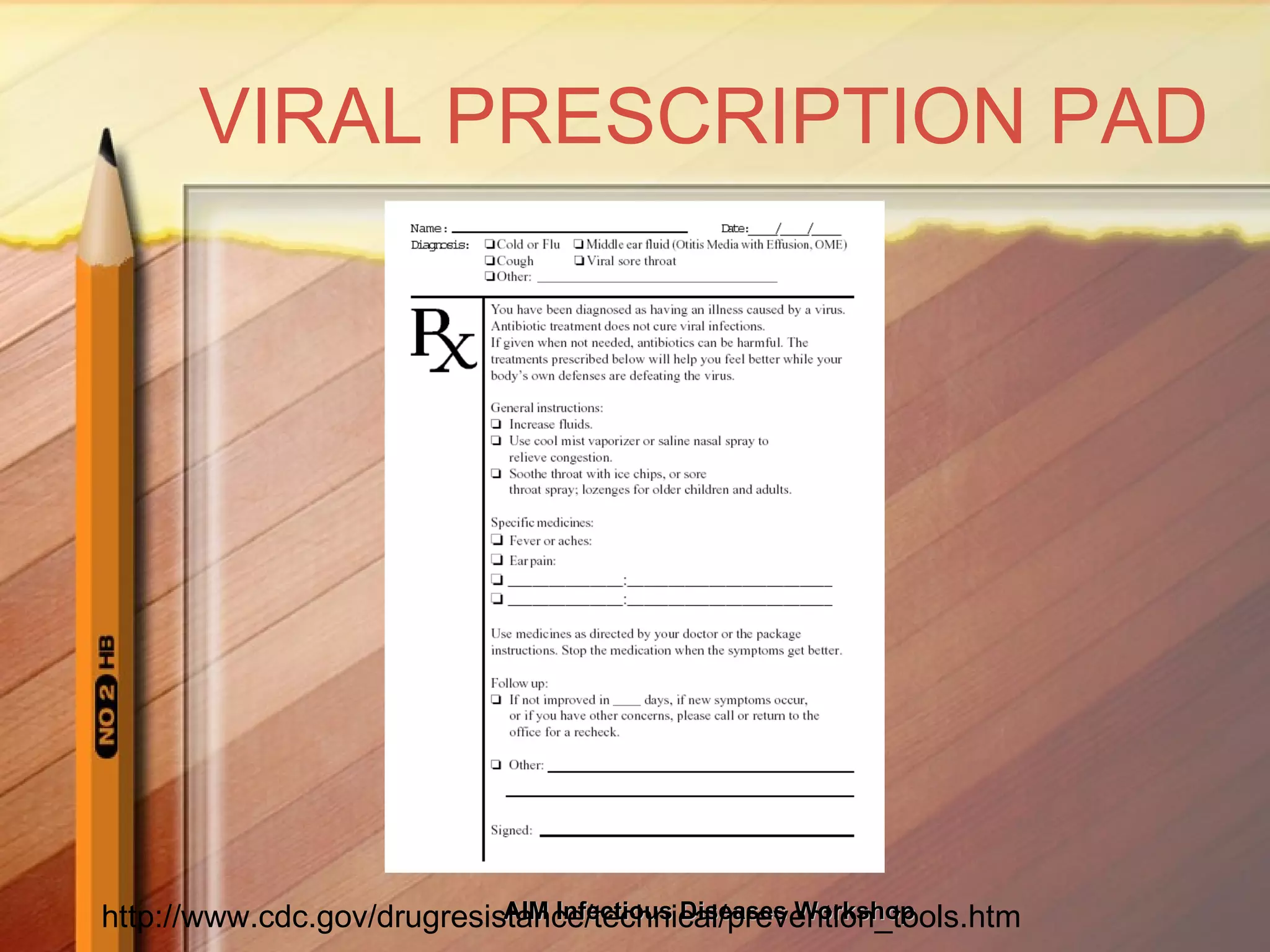
This document discusses the judicious use of antibiotics and increasing antibiotic resistance. It provides information on common infectious disease syndromes, likely pathogens, and antibiotic treatment options. It emphasizes using narrow-spectrum antibiotics when possible, older agents when feasible, and combination therapy only when necessary to help reduce antibiotic overuse and resistance.