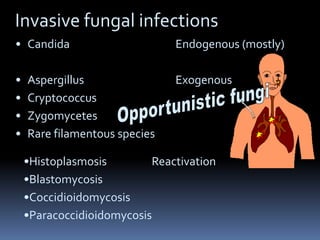
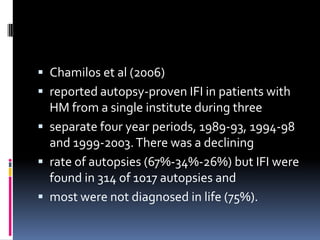
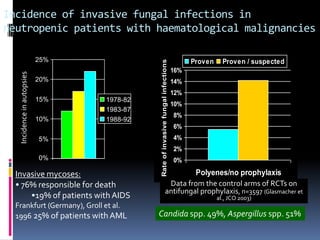
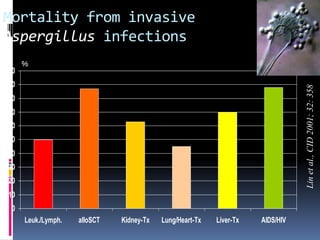
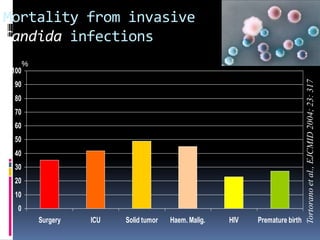
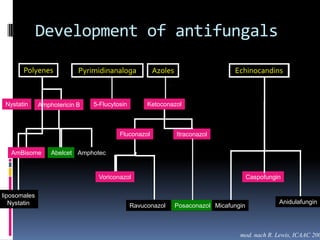
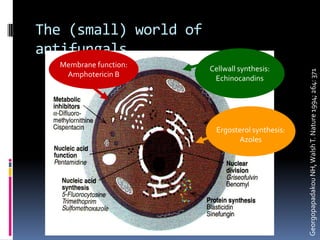
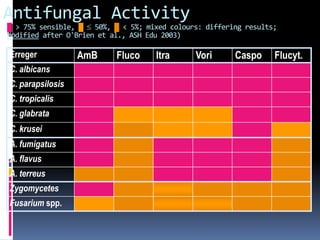
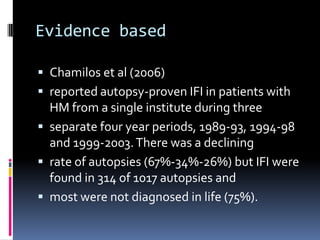
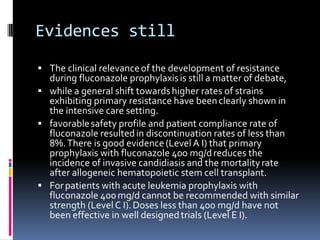
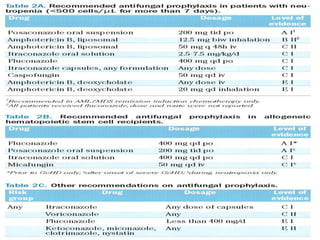
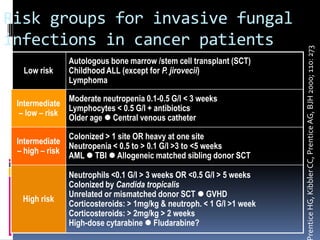
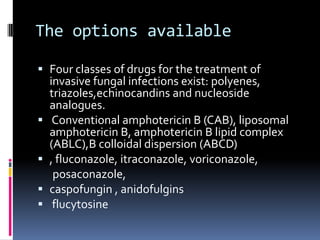
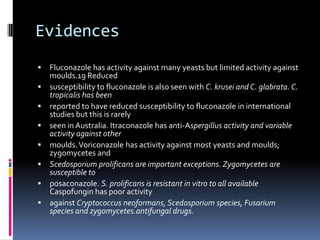
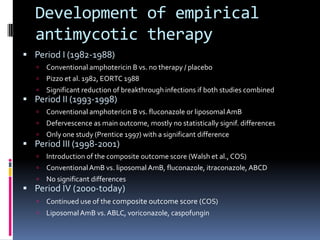
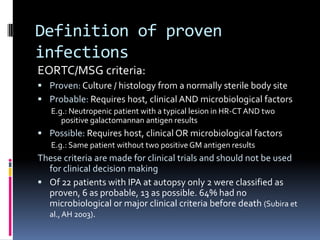
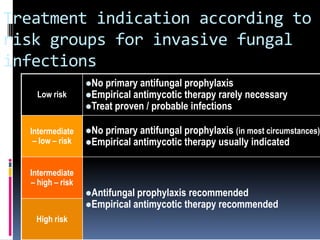
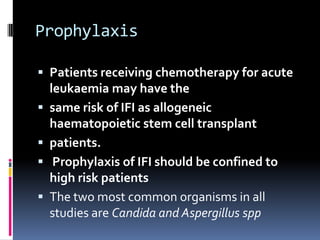
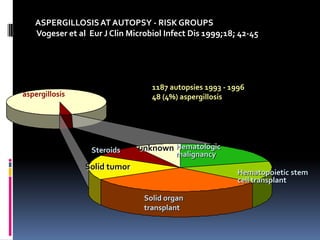
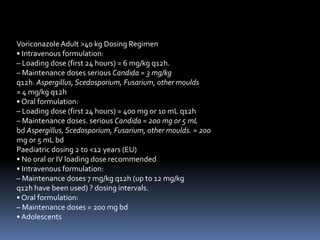
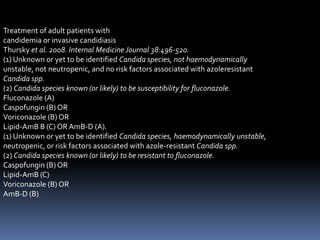
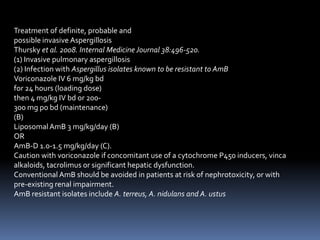
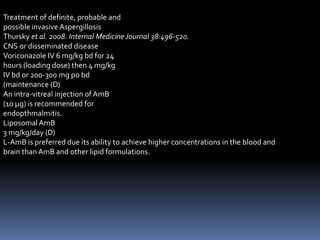
The document discusses the management of invasive fungal infections in Nigeria. It notes increasing cases of such infections with poor diagnostic tools. The main invasive fungal pathogens are discussed including Candida, Aspergillus, Cryptococcus, and some rare molds. Risk factors for invasive fungal infections in cancer patients are presented. The need for empirical antifungal therapy due to limitations in diagnosis is explained. The options for antifungal drugs including various azoles and echinocandins are also summarized.