Chronic myeloid leukemia
•Download as PPTX, PDF•
19 likes•9,939 views
Report
Share
Report
Share
Recommended
The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic NeoplasmsThe 5th edition of the World Health Organization Classification of Haematolym...

The 5th edition of the World Health Organization Classification of Haematolym...Dr Seena Tresa Samuel
More Related Content
What's hot
The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic NeoplasmsThe 5th edition of the World Health Organization Classification of Haematolym...

The 5th edition of the World Health Organization Classification of Haematolym...Dr Seena Tresa Samuel
What's hot (20)
The 5th edition of the World Health Organization Classification of Haematolym...

The 5th edition of the World Health Organization Classification of Haematolym...
Viewers also liked
Viewers also liked (20)
Similar to Chronic myeloid leukemia
Similar to Chronic myeloid leukemia (20)
Unit 18 (B); Leukemia! A disease of white blood Cells

Unit 18 (B); Leukemia! A disease of white blood Cells
Chronic Myeloid Leukemia by Dr. Sookun Rajeev Kumar

Chronic Myeloid Leukemia by Dr. Sookun Rajeev Kumar
Presentation of diagnosis related to cancer by heena

Presentation of diagnosis related to cancer by heena
leukemia in children with difference btw all and bll

leukemia in children with difference btw all and bll
APPROACH TO PATIENT WITH MASSIVE SPLENOMEGALY ONLY ME.pptx

APPROACH TO PATIENT WITH MASSIVE SPLENOMEGALY ONLY ME.pptx
Recently uploaded
Genuine Call Girls Hyderabad 9630942363 Book High Profile Call Girl in Hyderabad Genuine Escort ServiceGenuine Call Girls Hyderabad 9630942363 Book High Profile Call Girl in Hydera...

Genuine Call Girls Hyderabad 9630942363 Book High Profile Call Girl in Hydera...GENUINE ESCORT AGENCY
Recently uploaded (20)
Nagpur Call Girl Service 📞9xx000xx09📞Just Call Divya📲 Call Girl In Nagpur No💰...

Nagpur Call Girl Service 📞9xx000xx09📞Just Call Divya📲 Call Girl In Nagpur No💰...
Chandigarh Call Girls Service ❤️🍑 9809698092 👄🫦Independent Escort Service Cha...

Chandigarh Call Girls Service ❤️🍑 9809698092 👄🫦Independent Escort Service Cha...
Call Girls Bangalore - 450+ Call Girl Cash Payment 💯Call Us 🔝 6378878445 🔝 💃 ...

Call Girls Bangalore - 450+ Call Girl Cash Payment 💯Call Us 🔝 6378878445 🔝 💃 ...
❤️Chandigarh Escorts Service☎️9814379184☎️ Call Girl service in Chandigarh☎️ ...

❤️Chandigarh Escorts Service☎️9814379184☎️ Call Girl service in Chandigarh☎️ ...
Pune Call Girl Service 📞9xx000xx09📞Just Call Divya📲 Call Girl In Pune No💰Adva...

Pune Call Girl Service 📞9xx000xx09📞Just Call Divya📲 Call Girl In Pune No💰Adva...
Gastric Cancer: Сlinical Implementation of Artificial Intelligence, Synergeti...

Gastric Cancer: Сlinical Implementation of Artificial Intelligence, Synergeti...
Circulatory Shock, types and stages, compensatory mechanisms

Circulatory Shock, types and stages, compensatory mechanisms
👉 Amritsar Call Girls 👉📞 8725944379 👉📞 Just📲 Call Ruhi Call Girl Near Me Amri...

👉 Amritsar Call Girls 👉📞 8725944379 👉📞 Just📲 Call Ruhi Call Girl Near Me Amri...
Call Girl In Indore 📞9235973566📞 Just📲 Call Inaaya Indore Call Girls Service ...

Call Girl In Indore 📞9235973566📞 Just📲 Call Inaaya Indore Call Girls Service ...
ANATOMY AND PHYSIOLOGY OF REPRODUCTIVE SYSTEM.pptx

ANATOMY AND PHYSIOLOGY OF REPRODUCTIVE SYSTEM.pptx
7 steps How to prevent Thalassemia : Dr Sharda Jain & Vandana Gupta

7 steps How to prevent Thalassemia : Dr Sharda Jain & Vandana Gupta
Bandra East [ best call girls in Mumbai Get 50% Off On VIP Escorts Service 90...

Bandra East [ best call girls in Mumbai Get 50% Off On VIP Escorts Service 90...
Genuine Call Girls Hyderabad 9630942363 Book High Profile Call Girl in Hydera...

Genuine Call Girls Hyderabad 9630942363 Book High Profile Call Girl in Hydera...
Premium Call Girls Dehradun {8854095900} ❤️VVIP ANJU Call Girls in Dehradun U...

Premium Call Girls Dehradun {8854095900} ❤️VVIP ANJU Call Girls in Dehradun U...
Cardiac Output, Venous Return, and Their Regulation

Cardiac Output, Venous Return, and Their Regulation
Call Girls Shahdol Just Call 8250077686 Top Class Call Girl Service Available

Call Girls Shahdol Just Call 8250077686 Top Class Call Girl Service Available
Race Course Road } Book Call Girls in Bangalore | Whatsapp No 6378878445 VIP ...

Race Course Road } Book Call Girls in Bangalore | Whatsapp No 6378878445 VIP ...
Goa Call Girl Service 📞9xx000xx09📞Just Call Divya📲 Call Girl In Goa No💰Advanc...

Goa Call Girl Service 📞9xx000xx09📞Just Call Divya📲 Call Girl In Goa No💰Advanc...
Chronic myeloid leukemia
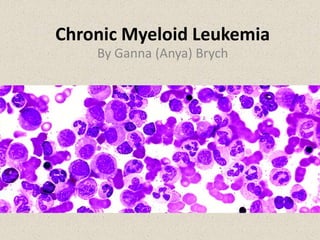
- 1. Chronic Myeloid Leukemia By Ganna (Anya) Brych
- 2. General Overview • Also called: -chronic myelogenous leukemia -chronic granulocytic leukemia -chronic myelocytic leukemia. • mostly affects adults (chance increases in people 65 and older) • Can develop in children/younger people • Epidemiology= Can not be transmitted • Prognosis = live good-quality lives with medication
- 3. Symptoms • Some don’t have symptoms in first stages Possible symptoms: -Leukopenia (shortage of normal white blood cells) -Neutropenia (low levels of normal neutrophils) -Thrombocytopenia (shortage of blood platelets) -Bleeding and bruising -Anemia -Shortness of breath
- 4. Symptoms (cont.) Possible symptoms (cont.) : -Feeling of fullness in the abdomen -Fever -Enlarged lymph nodes -Night sweats -Weight loss -Loss of appetite -Recurrent infections
- 5. Diagnosis • Blood Tests - a complete blood count (CBC) - lower-than-normal red cell count - abnormal number of platelets (either too high or too low) - High white cell count - a blood cell examination (test for leukemic blast cells and marrow cells) - high proportion of white cells
- 6. Diagnosis (cont.) • Bone Marrow Tests - bone marrow aspiration (remove a liquid marrow sample) - bone marrow biopsy (remove a small amount of bone marrow) • measure the number/structure of chromosomes • determine any chromosome abnormality (Ph chromosome) • confirm blood test findings
- 7. Diagnosis (cont.) • Hematopathologist confirms the diagnosis + identifies the phase • Looks for: -presence of the Philadelphia chromosome -number of cells with the Bcr-Abl oncogene Can Perform: • Cytogenetic analysis - identifies certain changes in chromosomes and genes by use of a karyotype • Fluorescence in situ hybridization (FISH) - detects Bcr-Abl using fluorescent dyes • Polymerase chain reaction (PCR) - identify and measure Bcr-Abl oncogenes not found by “FISH”
- 8. Causes • Risk factors -exposure to very high doses of radiation -high-dose radiation therapy (radiotherapy) • Abnormal chromosome (Philadelphia or Ph chromosome) = translocation between chromosomes 22 and 9 • Causes development of cancer-causing gene (oncogene) Bcr-Abl
- 9. Development • oncogene causes production of mutated protein called Bcr-Abl tyrosine kinase by stem cells • starts with a mutation to a single stem cell (in the bone marrow) • Stem cells form blood cells • multiplies into many cells • The CML cells grow and survive better than normal cells • Uncontrolled growth of CML cells = cancerous
- 10. Phases • Each phase determined by the number of blast cells • Severity of symptoms increases • 3 Phases -Chronic Phase CML -Accelerated Phase CML -Blast Crisis Phase CML
- 11. Chronic Phase CML • symptoms are mild or not noticeable. • white cells can still fight infection. • long-term drug therapy can control chronic phase • return to normal activities after treatment begins.
- 12. Accelerated Phase CML • Low of red cells, • low number of platelets • an increase or decrease in white cells • a high number of blast cells • Symptoms may appear: -swollen spleen -stomach discomfort
- 13. Blast Crisis Phase CML • increased number of blast cells in marrow and blood • low red cell and platelet counts • Symptoms : -infection -bleeding -a lack of energy or feelings of tiredness -shortness of breath -stomach pain (from an enlarged spleen) -bone pain • effects similar to those caused by an acute leukemia
- 14. Treatment • 2001 FDA approved tyrosine kinase inhibitor drugs (most commonly used today) • Dose depends on the phase of CML • TKI drug therapy doesn't cure chronic phase CML -> stable remission • Regular blood and marrow tests to check progress of treatment
- 15. Chronic Phase Treatment • Tyrosine kinase inhibitor (TKI) drugs -imatinib mesylate (Gleevec®) -dasatinib (Sprycel®) -nilotinib (Tasigna®) • If Initial Therapy Fails -interferon alpha (Roferon®-A and Intron® A) -pegylated interferon alpha -hydroxyurea (Hydrea®) -cytarabine (Cytosar-U®) -busulfan (Myleran®) ** harsher side effects **
- 16. Accelerated Phase and Blast Crisis Phase Treatment • Tyrosine kinase inhibitor (TKI) drugs -imatinib mesylate (Gleevec®) -dasatinib (Sprycel®) -nilotinib (Tasigna®) • If Initial Therapy Fails -interferon -busulfan (Myleran®) -cytarabine (Cytosar-U®) -hydroxyurea (Hydrea®) • Leukapheresis (removal of white blood cells) • Stem cell transplant
- 17. Bibliography • "BCR Rearrangement–Negative Chronic Myelogenous Leukemia Revisited." Journal of Clinical Oncology. American Society of Clinical Oncology, n.d. Web. 15 Mar. 2014. <http://jco.ascopubs.org/content/19/11/2915/F3.expansion>. • "Chronic Myeloid Leukemia (CML)." Learn About Cancer. American Cancer Society, n.d. Web. 15 Mar. 2014. • "Chronic Myeloid Leukemia." MedlinePlus. U.S. National Library of Medicine, n.d. Web. 15 Mar. 2014. <http://www.nlm.nih.gov/medlineplus/chronicmyeloidleukemia.htm l>.<http://www.cancer.org/cancer/leukemia- chronicmyeloidcml/index>. • "Chronic Myelogenous Leukemia." Leukemias. Memorial Sloan Kettering Cancer Center, n.d. Web. 15 Mar. 2014. <http://www.mskcc.org/cancer-care/adult/chronic-myelogenous- leukemia>. • Shah, Neil P. "Chronic Myeloid Leukemia." Disease Information and Support. The Leukemia and Lymphoma Society, n.d. Web. 15 Mar. 2014. <http://www.lls.org/#/diseaseinformation/leukemia/chronicmyeloidleuk emia/>.