Lecture 11 & 12 Clot
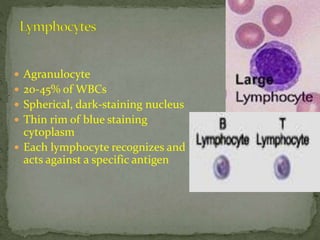
- 1. Agranulocyte 20-45% of WBCs Spherical, dark-staining nucleus Thin rim of blue staining cytoplasm Each lymphocyte recognizes and acts against a specific antigen
- 2. T lymphocytes can attack foreign cells directly (17.6)
- 3. B lymphocytes transform into plasma cells and secrete antibodies
- 4. Hemostasis means prevention of blood loss and this achieved by: 1. Vascular constriction 2. Formation of a platelet plug 3. Formation of blood clot 4. Growth of fibrous tissue into the blood clot
- 5. After blood vessel has been cut, the smooth muscle wall contract; this immediately reduces the flow of blood from the ruptured vessel
- 6. Platelets or thrombocytes Formed in the bone marrow from megakaryocytes Do not have nuclei Function in the clotting process. Normal value – 150,000 to 300,000/cubic millimeter. It has a half life in the blood of 8 – 12 days, its functional process run out over several weeks Formation of platelet plug
- 8. 1. Contractile protein thrombosthenin that can cause the platelet to contract 2. Endoplasmic reticulum that store Calcium ions 3. Mitochondria capable of forming ATP 4. Enzymes that can synthesize prostaglandins which involves in local tissue reactions 5. Contain fibrin stabilizing factor 6. Growth factors that causes vascular cells to grow and multiply
- 9. Platelet begin to swell and assume irregular forms when comes in contact with collagen fibers They become sticky so that they adhere to collagen in the tissue They secrete ADP and form thromboxane which activate nearby platelets The damaged vascular wall activates increasing numbers of platelets thus forming platelet plug. (In small vessels the platelet plug is all that is necessary to stop the bleeding).
- 10. 1. Exposed collagen binds and activate platelets 2. Release of platelet factors 3. Attract more platelets 4. Aggregate into platelet plug
- 11. Blood coagulation take place in three steps 1. As result of rupture blood vessels, formation of prothrombin activator (protein manufacture in the liver) 2. Conversion of prothrombin to thrombin in the presence of calcium 3. The thrombin acts as enzyme to convert fibrinogen (blood protein) into fibrin fibers that enmesh platelet, blood cells and plasma to form clot Note: vitamin K is required by liver for formation of prothrombin
- 12. Prothrombin Prothrombin Ca Activator Thrombin Fibrinogen Fibrinogen monomer Ca Fibrin fibers Activated fibrin Stabilizing factor Cross linked fibrin fibers
- 13. SEM of a clot with platelet, fibrin mesh, rbc’s The clot composed of meshwork of fibrin fibers entrapping blood cells, platelets and plasma
- 15. Prothrombin activator is generally formed in two ways 1. Extrinsic pathway (begins with trauma to the vascular wall) 2. Intrinsic pathway (begin with the blood)
- 17. Preventing blood clotting in vascular system is 1. Smoothness of the endothelial cell surface 2. Layer of glycocalyx on the endothelium 3. Protein bound with the endothelial membrane thrombomodulin which binds thrombin
- 18. The most important anticoagulant in the blood 1. Fibrin fibers 2. Antithrombin III or antithrombin-heparin cofactor Both fibrin fibers and antithrombin acts as antithrombin About 85-90% of thrombin becomes adsorbed to the fibrin fibers The thrombin that does not adsorb combines with antithrombin III which block the effect of thrombin
- 19. Heparin is anticoagulant, low concentration in the blood Effectiveness of antithrombin III increases when it combines with heparin Heparin is formed by basophilic and mast cell
- 20. Plasma protein contain euglobulin called plasminogen when activated becomes plasmin Plasmin resemble trypsin Plasmin digest fibrin fibers and other protein coagulants Plasmin caused lysis of a clot
- 21. Injured tissue release activator called tissue plasminogen activator (t-PA) which convert plasminogen to plasmin
- 23. Red blood cells White blood cells Platelets 1 Site of formation formed in bone marrow, life-span: 4 months formed in bone marrow or thymus formed in blood marrow 2 Shape biconcave discs, no nucleus, red colour phagocytes: irregular, lobed nucleus & granular cytoplasm irregular shape, no nucleus, tiny pieces of cell fragments,
- 24. Red blood cells White blood cells Platelets 3 Size small in size some large & some small tiny cell fragments 4 Number 5,000,000 /mm3 7,000 /mm3 250,000/mm3 5 Function contain haemoglobin to carry oxygen from lungs to all parts of body phagocytes kill pathogens & digest dead cells lymphocytes produce antibodies for killing pathogens for blood clotting
- 25. Albumin Helps control osmotic pressure Helps control diffusion of water Globulin Includes antibodies (Abs) Transport proteins (lipids, iron, copper, etc.) Fibrinogen Involved in clotting
- 26. All the albumin and fibrinogen and 50 – 80% of globulin are formed in the liver The reminder of the globulin are formed in the lymphoid tissues
- 27. Total protein: 4.2 - 5.6 g/dl Albumin: 2.3 - 3.5 g/dl Globulin: 1.9 – 2.1 g/dl
- 28. 66 kDa ALBUMIN Accounts for ~50% of the total plasma protein and ~ 50% of the total liver protein production Half-life ~ 20 days Highly polar At pH 7.4 it is anionic with 20 negative charges per molecule
- 30. Functions of albumin Maintenance of the osmotic pressure of plasma Transport of free fatty acids
- 31. Globulin is made up of different proteins called alpha, beta, and gamma types. Some globulins are made by the liver, while others are made by the immune system. Other globulins transport metals, such as iron, in the blood and help fight infection.
