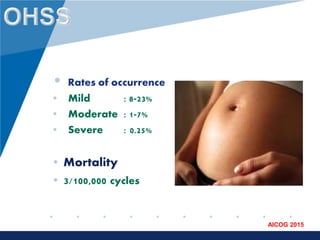
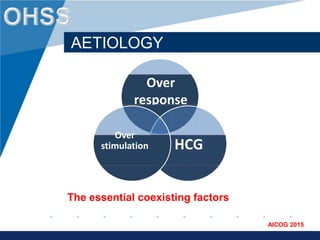
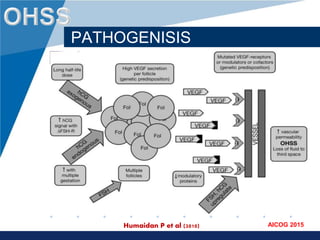
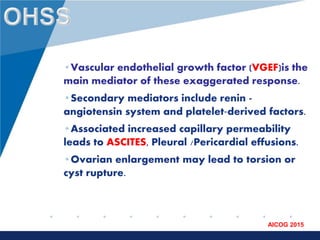
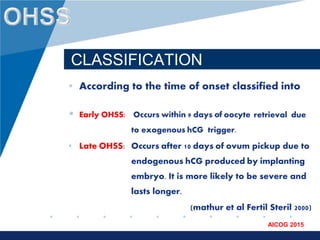
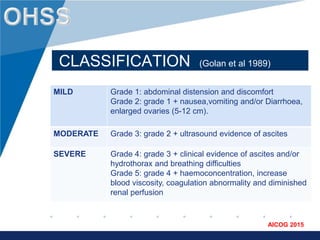
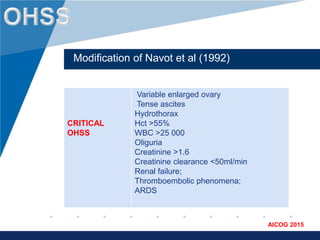
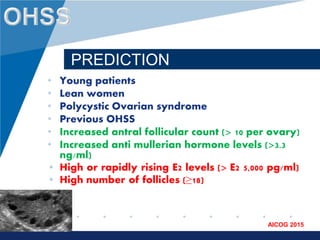
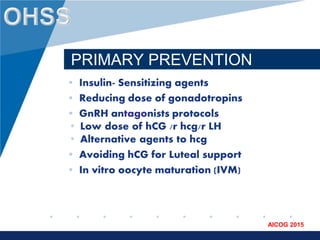
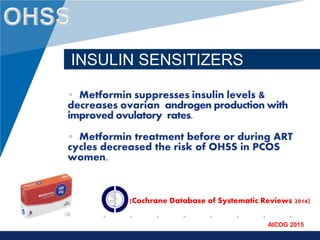
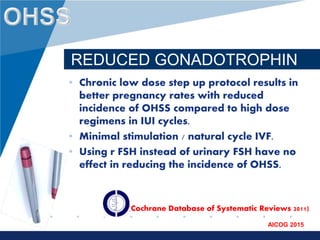
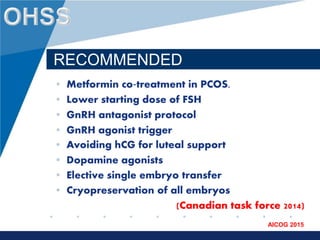
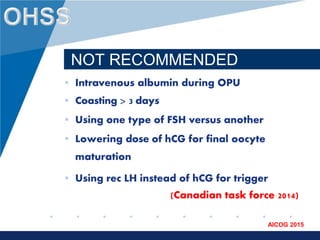
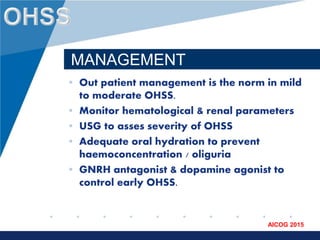
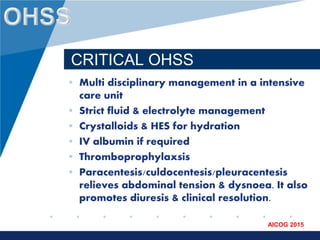
Ovarian hyper stimulation syndrome (OHSS) is an exaggerated response to ovulation induction that is usually associated with exogenous gonadotropin stimulation. It is typically a self-limiting condition, but can progress to become severe and be associated with increased pregnancy complications. OHSS is classified based on severity of symptoms and managed through prediction, prevention strategies like using a GnRH antagonist protocol or cryopreserving all embryos, and treatment of symptoms for mild-moderate cases or intensive care for critical OHSS. Further research aims to reduce OHSS risk while allowing for fresh embryo transfers.