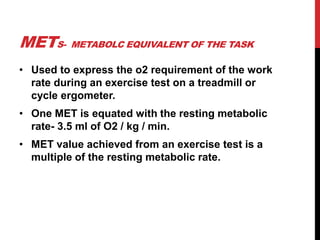
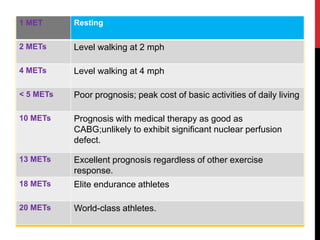
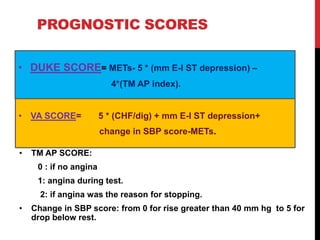
This document provides information about exercise electrocardiography (ECG or EKG). It discusses how exercise ECG is a non-invasive tool to evaluate the cardiovascular system's response to exercise. During exercise, the body's metabolic rate and cardiac output increase significantly. The document outlines safety precautions for exercise ECG and describes physiological responses like changes in heart rate and oxygen uptake during exercise and recovery. Contraindications for the test and criteria for terminating the test early are also summarized. Finally, the document discusses benefits of exercise testing after a heart attack and some prognostic scoring systems used with exercise ECG.