presentation1-160607012326 (1).pdf
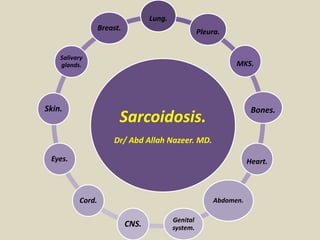
- 1. Sarcoidosis. Dr/ Abd Allah Nazeer. MD. Lung. Pleura. MKS. Bones. Heart. Abdomen. Genital system. CNS. Cord. Eyes. Skin. Salivary glands. Breast.
- 2. Sarcoidosis is an inflammatory, multisystemic, disease of unknown etiology, characterized pathologically by the presence of non-caseating granulomas. Pulmonary involvement in sarcoidosis is reported in up to 90% of patients. It resolves spontaneously in the majority of cases, but fibrosis causing permanent functional impairment develops in 20 to 25% of patients, resulting in death in 5-10% of them. Sarcoidosis is the most frequent among the interstitial lung diseases, showing a higher incidence in women than in men and begins most often between 20 and 40 years of age. The extra pulmonary involvement, particularly skin and eyes, is present in 25% of cases, while more rare is the involvement of central nervous system, heart and kidneys. There are multiple clinical and radiological appearances: half of patients is asymptomatic at the time of diagnosis and the involvement of various organs can vary significantly from patient to patient. Chest X-ray has been widely used in the past in the diagnosis and staging of the disease. The use of high-resolution computed tomography (HRCT) provides detailed information on the wide spectrum of radiological presentation of sarcoidosis. In some cases the definitive diagnosis of sarcoidosis needs transbronchial biopsy or broncho- alveolar lavage especially in clinical or radiological atypical cases.
- 3. Clinical features The most common clinical features are respiratory symptoms (cough, dyspnea, bronchial hyper- reactivity), fatigue, night sweats, weight loss and erythema nodosum. However, up to 50% of cases of sarcoidosis are asymptomatic and abnormalities are identified incidentally on the chest radiograph. Pulmonary function tests typically show a restrictive ventilatory pattern with decreased lung volumes and reduced carbon monoxide diffusion. In presence of endobronchial involvement, an obstructive ventilatory pattern may occur Siltzbach defines 5 stages of sarcoidosis: • stage 0 : normal chest radiograph • stage I : lymph node enlargement • stage II : lymph node enlargement and pulmonary opacities • stage III : pulmonary opacities • stage IV : pulmonary fibrosis
- 5. Lymphadenopathy typical patterns The most common pattern is a well-defined, bilateral and symmetric hilar and right paratracheal lymph nodes enlargement. Bilateral hilar lymph nodes enlargement, alone or in combination with mediastinal lymph nodes enlargement, occurs in an estimated 95% of patients affected with sarcoidosis. Middle mediastinal nodes (at the left paratracheal level, subcarinal level and level of the aortopulmonary window), prevascular nodes, or both, are involved in approximately 50% of patients. Bilateral hilar lymph nodes enlargement may be a finding of infection or malignancy. However, in the absence of specific symptoms or signs, sarcoidosis is the most common cause of this feature. Although histological confirmation is not required for a diagnosis of sarcoidosis in these patients, a biopsy should be performed if the imaging findings worsen or specific signs and symptoms develop.
- 6. Multiple enlarged mediastinal lymph nodes in the prevascular space and pre-tracheal retro-caval space.
- 7. Axial HRCT scan that shows bilateral subcarinal and hilar enlarged lymph nodes.
- 8. Axial HRCT scan that shows bilateral subcarinal and hilar enlarged lymph nodes.
- 9. (a) Axial contrast material–enhanced CT scan (mediastinal window) shows typical bilateral and symmetric hilar (arrows) and subcarinal (*) lymphadenopathy.(b) Axial unenhanced CT scan (mediastinal window) obtained at the level of the left pulmonary artery shows enlargement of right paratracheal and left hilar lymph nodes (arrows). Although the right hilum is not shown, it too was affected. (c) Axial unenhanced CT scan (mediastinal window) shows punctate calcifications of hilar lymph nodes (arrows), a pattern that also occurs in other chronic granulomatous diseases. (d) Axial contrast-enhanced CT scan shows bilateral eggshell-like calcifications of hilar and mediastinal lymph nodes (arrows).
- 10. Atypical patterns: Atypical patterns of lymphadenopathy occur more frequently in patients older than 50 years. Lymph nodes enlargement may be asymmetric or show unusual locations (i.e., internal mammary chain, paravertebral or rtero- crural regions). Such findings should lead to the inclusion of entities such as lymphoma or tuberculosis in the differential diagnosis. Isolated unilateral hilar lymph nodes enlargement, usually on the right side, is seen in less than 5% of cases. Enlargement of mediastinal lymph nodes without hilar lymph nodes enlargement is even less common. The enlarged nodes may occasionally become calcified, this being related to the duration of the disease (calcification occurs in 3% of patients after 5 years and in 20% after 10 years). The calcifications in sarcoidosis may be indistinguishable from those seen in tuberculosis and histoplasmosis. Eggshell-like calcifications may also be identified in silicosis.
- 11. Calcified enlarged lymph nodes in the pre-tracheal space in a patient with sarcoidosis. Nodular pattern with peribronchovascular and subpleural distribution, where nodules show a tendency to conglomerate leading to formation of masses.
- 12. Axial CT scan shows bilateral enlargement and peripheral calcification of mediastinal and hilar lymph nodes.
- 13. Four different patients with sarcoidosis show various patterns of atypical lymphadenopathy.
- 14. PARENCHIMAL MANIFESTATIONS : TYPICAL PATTERNS MICRONODULES WITH A PERILYMPHATIC DISTRIBUTION A perilymphatic distribution of micronodular lesions is the most common pattern of parenchymal disease in patients with sarcoidosis (75-90% of cases). HRCT shows well-defined, small (2-4 mm) and rounded nodules, usually with a bilateral and symmetric distribution, predominantly in the upper and middle lung zones. The nodules are found most often in the peribronchovascular interstitium and less often in the interlobular septa. The micronodular lesions may coalesce over time, forming larger lesions. Sarcoid granulomas frequently cause nodular or irregular thickening of the peribronchovascular interstitium.
- 15. Frontal chest radiograph that exhibits a sarcoidosis-related diffuse bilateral micronodular pattern, more profuse in upper lung zones.
- 16. Nodules with a typical perilymphatic distribution. Scheme of distribution (A) MIP axial planes (B) and MIP coronal planes (C) showing perilymphatic nodules in sarcoidosis with typical involvement of dorsal regions of upper lobes.
- 17. Diffuse bilateral micronodular pattern showing a peribronchovascular distribution, compatible with sarcoidosis.
- 18. Micronodular pattern with a peribronchovascular distribution and numerous subpleural nodules showing tendency to conglomerate. Infra-carinal enlarged lymph nodes.
- 19. FIBROTIC CHANGES In most patients, sarcoid granulomas resolve with time without treatment. However, an estimated 20% of patients develop pulmonary fibrosis, showing linear opacities, traction bronchiectasis and architectural distortion, in a patchy distribution, usually in the upper and middle lung zones. Frontal chest radiograph showing pulmonary masses in middle and upper zones causing traction and pulmonary architectural distortion along with bullae formation. Findings related to fibrotic lung changes in sarcoidosis.
- 20. Axial unenhanced high-resolution CT scan obtained in a patient sarcoidosis shows bilateral cystic spaces and cavities results of chronic fibrosis . The fibrotic cystic lesions that occur in sarcoidosis typically involve the upper and middle lung zones and follow the large airways in a perihilar distribution
- 21. HRCT scans at the level of the aortic arch (A) and the pulmonary trunk (B) showing a classic appearance of advanced fibrotic sarcoidosis. A dense conglomerate mass in the right upper lobe and bilateral traction bronchiectasis that radiate from the hilum towards the dorsal regions of upper lobes. There is also evident intralobular interstitial thickening in the upper lobes.
- 22. Alveolar sarcoid pattern of airspace consolidation in pulmonary sarcoidosis. Axial high-resolution CT scan shows alveolar consolidation in the left upper lobe and patchy subpleural alveolar opacities in the right upper lobe. Architectural distortion and traction bronchiectasis, signs of fibrosis, also are evident
- 23. BILATERAL PERIHILAR OPACITIES: Areas of lung consolidation with irregular, blurred margins, radiating from the hilum toward the periphery, with or without air bronchogram. These areas of consolidation are formed by multiple confluent nodular opacities. Centrilobular and subpleural micronodular interstitial pattern accompanied by diffuse bilateral reticular areas with more extensive involvement of perihilar regions. Suggestive findings of stage III sarcoidosis.
- 24. Typical manifestations of pulmonary sarcoidosis. (a) Axial high-resolution CT scan shows multiple micronodules with a peribronchovascular distribution in both lungs, predominantly in the upper and middle lobes. One cluster of nodules in the periphery of the left upper lobe (arrow) has coalesced to form a conglomerate lesion (macronodule). (b) Coronal reformatted image from high-resolution CT clearly shows upper-lobe predominance of the micronodules.
- 25. ATYPICAL PATTERNS: PULMONARY NODULES AND MASSES Pulmonary nodules and masses are seen in 15%-25% of patients. On CT, they usually appear as ill-defined irregular opacities, measuring 1-4 cm in diameter, that represent coalescent interstitial granulomas. These lesions are typically multiple and bilateral, commonly located in perihilar or peripheral regions. HRCT showing an interstitial pattern with spiculated nodules in a peribronchovascular and subpleural distribution, predominantly in middle and upper lung zones. Associated to traction bronchiectasis and enlarged right hilum lymph nodes. Suggestive findings of sarcoidosis as first option.
- 26. Coronal maximum-intensity projection image obtained with lung window settings that shows a diffuse bilateral micronodular pattern with a peribronchovascular distribution and larger nodules.
- 27. CT scan of a patient with sarcoidosis shows bilaterally scattered ground glass pulmonary nodules mimicking metastasis .
- 28. Small satellite nodules are often identified at the periphery of these masses, giving an appearance that has been termed the "sarcoid galaxy sign".
- 29. Axial high-resolution CT scan shows several large, ill-defend nodules and areas of consolidation resulting from the confluence of multiple parenchymal micronodules composed of numerous tiny granulomas in both lungs. Fine nodular opacities are seen around the large nodules , and small low-attenuation spots that correspond to the spaces between partially coalescent small nodules are visible peripherally. This appearance has been termed the sarcoid galaxy sign.
- 30. PATCHY AIRSPACE CONSOLIDATION Patchy airspace consolidation is seen in 10%-20% of patients with sarcoidosis. It is usually bilateral and symmetric and predominantly affects the middle and upper lung zones. These regions may contain air bronchograms and commonly show ill-defined margins, with a nodular pattern toward the lung periphery. This pattern is known as the acinar or alveolar form of sarcoidosis, which may mimic pneumonia, tuberculosis, or bronchiolitis obliterans organizing pneumonia. Axial HRCT scan showing patchy bilateral lung consolidations, predominantly in hilum, with air bronchogram areas associated with small bilateral peripheral nodules. Related to distortion of the lung parenchyma. Suggestive findings of sarcoidosis.
- 31. PATCHY GROUND-GLASS OPACITIES Patchy ground-glass opacities result from the confluence of multiple granulomatous nodules and fibrotic interstitial lesions, which may cause airway compression but not airspace filling like that seen in alveolitis. These ground-glass opacities show ill-defined margins and air bronchogram may be present. Differential diagnosis must be made with bronchoalveolar carcinoma, lymphoma, pneumoconiosis, pneumonia and bronchiolitis obliterans organizing pneumonia. Axial HRCT scan in a patient with sarcoidosis showing an increased attenuation with a patchy pattern and a ground-glass appearance, predominantly in peripheral areas and upper lung zones. Interstitial thickening and some images of tree in bud nodules were also visible
- 32. LINEAR RETICULAR OPACITIES This pattern is produced by interlobular and intralobular septal thickening and is commonly seen in the subpleural space of the upper and middle lung zones. Although this pattern may simulate lymphangitic carcinomatosis, this disorder is characterized by a more extensive and more severe involvement of the interlobular septa and subpleural space than is typical either in lymphoma or in sarcoidosis. HRCT. Mixed pattern with a diffuse thickening of the interstitium, with both linear and nodular characteristics, along with thickening of the peripheral septa and axial interstitium.
- 33. MILIARY PATTERN This pattern is rare in sarcoidosis (< 1% of cases) and its presence requires a wide differential diagnosis, including entities such as tuberculosis, pneumoconiosis, metastatic lesions, histoplasmosis and histiocytosis. ATYPICAL MILIARY OPACITY
- 34. CT scans (A,B) demonstrate a distribution of nodules that is quite diffuse and uniform resembling a miliary pattern. The bronchoalveolar lavage revealed sarcoidosis. Five months CT scan follow-up (c) after therapy shows a marked reduction of nodules.
- 35. AIRWAY INVOLVEMENT The most common imaging findings of airway involvement are a mosaic attenuation pattern, air trapping, tracheobronchial abnormalities and atelectasis. Mosaic Attenuation Pattern: It refers to the presence of heterogeneous attenuation in the lung parenchyma on inspiratory CT images. In patients with sarcoidosis, this pattern results from airway involvement by granulomas or fibrosis, which may lead to obstruction. Air trapping: It is characterized by focal areas of decreased attenuation on expiratory CT images. It is a common, albeit nonspecific, feature. There is no correlation with the stage of the disease. Tracheobronchial Abnormalities: Stenosis, irregularity, distortion and focal areas of bronchiectasis. Atelectasis: As a result of the obstruction of lobar or segmental bronchi by granulomas.
- 36. Axial unenhanced high-resolution expiratory CT scan obtained in a patient with pulmonary sarcoidosis shows air trapping.
- 37. Axial unenhanced high-resolution expiratory CT scan obtained in a patient with pulmonary sarcoidosis shows a mosaic pattern consisting of multiple areas of low attenuation , interspersed with larger areas of normal lung parenchyma. This appearance is produced by air trapping.
- 38. HRCT scans (A,D) in patient with sarcoidosis showing some subtle areas of decreased attenuation related to air trapping (yellow arrows in A,B,D). There are also small perilymphatic nodules in the apical segment of the left lower lobe (red arrow in C).
- 39. Stage IV pulmonary sarcoidosis in a 60-year-old woman. Chest radiogram and thoracic HRCT demonstrate fibrotic changes and ground glass opacities with upper predominance (a finding confirmed on coronal CT reformation). This distribution is typical of sarcoidosis.
- 40. Stage IV pulmonary sarcoidosis in a 62-year-old man. Thoracic CT demonstrates extensive fibrotic change with a central distribution that distort the lung parenchyma and a cavitary lesion, predisposing to fungal infection, an aspergiloma (arrows). Note the presence of lymph nodes calcifications and the enlargement of pulmonary artery, a finding that suggests pulmonary hypertension
- 41. PLEURAL DISEASE Pleural involvement in sarcoidosis is rare (1%-4%). Manifestations of pleural involvement include pleural exudates or transudate, Chylothorax, hemothorax, pneumothorax, pleural thickening and, rarely, pleural calcification. Thickening of the perivascular interstitium in both lungs associated to a slight granulation in the cisural area and paratracheal and prevascular enlarged lymph nodes in a patient with sarcoidosis. The image demonstrates a small pleural effusion on the right side.
- 42. Pleural involvement in sarcoidosis is demonstrated. Axial CT scan shows bilateral granulomas with perilymphatic distribution and nodular thickening of interlobular septae, peribronchovascular interstitium and interlobar fissure.
- 43. Axial contrast-enhanced CT scan obtained at the subcarinal level in a patient with pulmonary sarcoidosis shows chronic pleural effusion, diffuse pleural thickening (arrows), and hilar and mediastinal lymphadenopathy.
- 44. Intra-abdominal involvement of sarcoidosis can be found in the absence of pulmonary or lymphatic disease (1). Liver (50-80%), spleen (40-80%), lymph nodes (30%) and kidney are more commonly involved, sometimes without symptoms. The lesions are less characteristic, mimicking more common neoplastic or infectious diseases such as lymphoma, diffuse metastasis, granulomatous or mycobacterial infections (2). In this educational exhibit we review the imaging manifestations of intra-abdominal sarcoidosis. Sarcoidosis is a multisystem inflammatory disease of unknown etiology, characterized by non- caseating epithelioid cell granulomas in the absence of other granulomatous diseases such as tuberculosis, fungal infections, autoimmune processes, or delayed-type hypersensitivity to foreign antigens .
- 45. Sarcoidosis of the Liver follows lymph nodes and lung in the frequency of involvement. Furthermore, it is reported that a significant fraction (26%) have liver lesions without lung involvement. About 50-79% of livers are involved by biopsy and 67-70% by autopsy. The commonest radiologic manifestation of hepatic sarcoidosis is hepatomegaly, which is found in about more than half of the patients on abdominal computed tomography (CT) scans. It is often together with splenomegaly. Other findings range from asymptomatic incidental granulomas to portal hypertension and cirrhosis from granulomas in the portal triad and fibrosis due to chronic inflammation. Portal vein thrombosis is reported as a frequent complication of hepatic sarcoidosis possibly as a result of stasis from obliteration of small portal veins. It is also suggested that there is an additional correlation between chronic hepatic sarcoidosis and hepatocellular carcinoma. Ultrasound (US) findings include parenchymal echogenicity, coarsening of the liver parenchyma with or without discrete nodules and contour irregularity. Calcification is uncommon but can be seen with long- standing disease. The nodules which represent the coalescence of small granulomas are typically innumerable, diffusely distributed and range from 1 to 2 mm to several centimeters in size. They have been reported to be hypoechoic on US and hypodense on computed tomography (CT) scans, relative to the background liver parenchyma. However, they may also be hyperechoic based on the background liver echogenicity and degree of fibrosis present in the granuloma. Focal nodules are the lesions identified in 5% of patients at imaging. On MRI, the lesions are hypointense on all sequences most conspicuous on the T2-weighted fat- saturated images. They enhance less than the background liver on gadolinium-enhanced T1- weighted images. Rarely, an increased signal intensity of diffusely involved liver is detected on T2-weighted images when compared with the normal spleen.
- 46. A 61-year-old female patient affected by pulmonary biopsy proved sarcoidosis. Routine abdominal ultrasound exam (a and b) shows multiple, small, randomly distributed, hypoechoic nodules in the liver parenchyma.
- 47. Liver MRI of the same patient with pulmonary sarcoidosis, which demonstrates multiple, scattered, small, hyperintense nodules on T2-weighted images (a and d) and on diffusion-weighted images (b and e). After gadolinium administration above-mentioned lesions appear hypointense (c and f).
- 48. a. Axial ultrasound image shows multiple, diffusely distributed, small, hypoechoic, rounded granulomas in enlarged liver and periportal hypoechoic enlarged lymph node (arrow). b. Sagittal ultrasound image shows 3.5 cm sized, hypoechoic, focal splenic lesion. c. Axial contrast enhanced CT image shows contour irregularity of the enlarged liver. Multiple, diffusely distributed hypodense granulomas ranging from 1 to 2 cm are detected in the liver and spleen. d. Axial contrast enhanced CT image shows irregular, large, hypodense areas representing coalescence of the granulomas in the liver and hypodense granulomas ranging from 1 to 2 cm in the spleen.
- 49. a. Axial ultrasound image shows 1 cm sized, hypoechoic, rounded granuloma in the peripheral subcapsular region of the liver. b. Axial T1W- GRE image demonstrates hypointensity of the same lesion.
- 50. A 66-year-old female patient affected by breast cancer and sarcoidosis. Chest CT-scan shows pulmonary sarcoidal localizations and hilar lymphadenopathy (a and b). Abdomen CT scan demonstrates a slightly hypo-attenuating small liver lesion (c; white arrow) with associated enlarged lymph-nodes (d). MRI (e and f) also shows both liver lesion (e; white curved arrow), which appears hypo-intense in hepatobiliary phase, and lymph-nodes (f).
- 51. 57-year-old woman with sarcoidosis and hepatic involvement; Ultrasonographic image (A) shows predominantly hyperechoic heterogeneous areas on right lobe of liver (arrows). Contrast-enhanced CT images (B, C) show lobulated outline of liver, hypodense bands and septations in liver parenchyma (arrows)
- 52. Sarcoidosis of the Spleen By fine needle aspiration and angiography, the frequency of splenic involvement has been reported in 24-53% of cases. Splenomegaly from sarcoidosis is usually associated with multiple organ involvement, commonly the lungs and the liver. Splenic infiltration can be homogeneous or in the form of multiple nodules. Splenic nodules can be seen in 15% of the cases undergoing CT scanning of the abdomen and are more common than the hepatic ones. Similar to the hepatic nodules, the splenic nodules are seen as multiple, hypodense, hypointense and non-enhancing lesions, scattered in the spleen. They tend to be discrete but may coalesce with increasing size. The differential diagnosis of low-attenuation nodules in the liver and spleen includes infection, metastatic disease, and lymphoma.
- 53. Contrast-enhanced CT images of a 32-year-old female (a and b) demonstrate multiple, small, hypoattenuating nodular lesions randomly distributed in splenic parenchyma. In c and d, MR exam of a 61-year-old female depicts splenic sarcoidal involvement. Multiple hypointense target lesions are shown on T2-weighted image (c) and on enhanced T1-weighted image (d), creating an heterogeneous parenchymal appearance.
- 54. Hepatosplenic sarcoidosis. T2-weighted fat-saturated images show hypointense lesions in the liver and spleen (a). The lesions enhance less than the background liver on gadolinium-enhanced T1-weighted images (b).
- 55. Sarcoidosis of the Gastrointestinal System Sarcoidosis of the gastrointestinal (GI) tract is extremely rare and the majority of the cases are asymptomatic. On autopsy, approximately 10% of systemic sarcoidosis patients were found to have gastric granulomatous mucosal infiltration, most often in the antrum. Antral narrowing and deformity which leads to gastric outlet obstruction may develop due to gastric mucosal fold enlargement mimicking Menetrier's disease. A segmental linitis plastica- type picture which should be differentiated from gastric carcinoma is the most common abnormality found on upper GI series. Extrinsic compression from extensive retroperitoneal lymphadenopathy may also occur throughout the GI tract. Small bowel involvement is the least common site of all in gut sarcoidosis. Extrinsic compression by abdominal and mesenteric lymph nodes or reduction of the lumen size secondary to cicatrizing constriction in consequence of mucosal granulomatous lesions, results in intestinal obstruction. Colorectal sarcoidosis can occur in the presence of grossly normal appearing mucosa. Colonic sarcoidosis involves multiple nodules, polyps, stenosis, obstructive lesions, aphthous erosions, or ulcers.
- 56. Sarcoidosis of the Peritoneum Sarcoidosis rarely affects the peritoneum. The most frequent clinical presentation is exudative ascites, multiple granulomatous nodules studding the peritoneum or a single peritoneal lesion. Peritoneal biopsy is required due to close gross visual resemblance, to rule out carcinomatosis, tuberculosis and fungal infections. Enlarged lymph nodes are detected in approximately 30% of patients particularly in the porta hepatis, para-aortic region, and celiac axis. Lymph nodes are typically smaller (less than 2 cm in diameter) and more discrete (rather than confluent) and less commonly involve the retro-crural area in sarcoidosis than lymphoma. CT scan of a 55-year-old female demonstrates multiple enlarged lymph-nodes located in mediastinum, especially in right and left hilum (a), and in abdomen - in celiac axis (b), in para-aortic and para caval region (c) and in the mesentery (d).
- 57. a. Axial contrast enhanced CT image shows peri cecal multiple enlarged lymph nodes b. Subsequent CT examination demonstrates wall thickening of the ileocecal area, heterogeneous hyperdensity of the omentum and also the mesenteric free fluid. c. Barium small bowel enema shows mucosal irregularity, nodularity and angulation of terminal ileum and ileocecal area. d. Coronal reformatted CT image shows multiple lymph nodes in the mesenteric root of the same region.
- 58. Contrast-enhanced abdominal CT of a 38-year-old male suffering from cough and abdominal pain. Enlarged lymph nodes in the mesenteric root (a, arrows), a markedly enlarged appendix with thickening of the wall (b, c, arrows) and thickening of the coecal apex (c, open arrow) are seen. Bronchoscopic and Colonoscopic biopsies revealed chronic granulomatous inflammation confirming the diagnosis of pulmonary and gastrointestinal sarcoidosis.
- 59. Sarcoidosis of the Pancreas Pancreatic sarcoidosis has been detected on autopsy in 1-3% of cases with systemic disease but it is rarely symptomatic during life. Typical symptoms of pancreatic involvement are due to direct tissue infiltration, duct obstruction, or constrictive peripancreatic lymphadenopathy. Sarcoidosis. Contrast-enhanced CT of the abdomen (a) shows enlarged lobulated pancreas. Ill- defined multiple small hypodense lesions are detected in the pancreatic head and body (b, arrows).
- 60. Sarcoidosis of the Kidney Nephrocalcinosis, nephrolithiasis, and interstitial calcium deposition have been reported in sarcoidosis and may lead to renal failure. Interstitial nephritis is a possible manifestation, and may demonstrate a striated nephrogram on contrast-enhanced CT. Glomerular nephritis from direct infiltration may also occur. Nephrocalcinosis is the most frequent effect of sarcoidosis on the kidney. It is in consequence of hypercalcemia or hypercalciuria secondary to granulomatous production of calcitriol. These granulomata are typically extra renal. Direct granulomatous involvement of the kidneys is rarely observed and is indistinguishable from lymphoma or metastasis Renal sarcoidosis.
- 61. Hepatic, splenic, and renal sarcoidosis. Contrast-enhanced CT of the abdomen (a, b) shows multiple hypodense granulomas infiltrating the liver and spleen. Small hypodense granulomas are also detected in both kidneys (a, b, arrows). Contour irregularity of the shrinking liver became prominent (c, dashed arrows) and contour irregularity of the right kidney at the site of granuloma occurred (d, dashed arrow) at five-month follow-up
- 62. Sarcoidosis of the Genital Tract The most common site of involvement of the female reproductive system is the uterus. It is usually detected during the investigation of abnormal uterine bleeding in patients with a previous history of sarcoidosis at other anatomic sites. Ovarian sarcoidosis is extremely rare and known to mimic ovarian malignancy with soft tissue nodules. There are no specific radiological findings in the literature to describe ovarian sarcoidosis. Sarcoidosis involving the male reproductive tract has rarely been reported. The epididymis, testis, and prostate gland, with only rare involvement of the spermatic cord, scrotum, and penis are reported in order of decreasing frequency. The lesions exhibit enhancement on gadolinium- based intravenous contrast administration T1-weighted images and low signal intensity on T2-weighted images. Testicular and scrotal sarcoidosis.
- 63. Testicular sarcoidosis proven by partial removal of the testis. B-mode and color Doppler US shows scrotal swelling and hypoechoic nodular areas in the left testis (arrows).
- 64. A 30-year-old male with biopsy-proven sarcoidosis. B-mode and color Doppler US of the testis shows nodular thickening of the tunica vaginalis (a, arrow) and of the head of the epidydimis (b).
- 65. Extra-testicular sarcoidosis proven by biopsy. US shows infiltration around the vas deferens (arrows), at the lower pole of the scrotum, which disappeared after treatment. The patient also had neurosarcoidosis.
- 66. Sarcoidosis with bilateral adnexal cystic masses are demonstrated (black arrows). The cyst wall on the right side is thick and irregular. There is marked thickening of the mesorectal fascia (long white arrow). Multiple prominent nodes are demonstrated along the pelvic sidewalls, which are very high in signal intensity on T2W (short white arrows).
- 67. MRI axial T2W image of the pelvis following treatment for sarcoidosis. The left adnexal cyst has resolved. There is a small residual cyst on the right (black arrow). There is marked decrease in the thickening of the mesorectal fascia (white arrow). The lymph nodes appear normal (short white arrows).
- 68. Neurosarcoidosis: Neurosarcoidosis affects about 27-37% of patients at autopsy, but it is diagnosed ante mortem only in less than 10% of cases, because the clinical presentation depends on the site of the lesions. The lesions are usually located in the base of the brain and sometimes also the optic and facial nerve are involved. Sarcoidal nodules can be solitary or multiple with a ringlike appearance, showing enhancement after contrast injection in the activity phase. This appearance can simulate glioblastoma or metastases. Typically, in the periventricular and deep white matter, they are also visible as hyperintense lesions in T2-weighted images, simulating multiple sclerosis. Leptomeningeal localizations are visible better after contrast injection, showing a diffuse enhancement. In spinal cord, especially in cervical and thoracic regions, lesions appear hypointense in T2-weighted MRI sequences with hyperintensity of the associated edema. They show enhancement on T1-weighted images after contrast injection.
- 69. Neurosarcoidosis is an uncommon condition with protean manifestations. Magnetic resonance imaging (MRI) is often used in the diagnostic evaluation and follow-up of patients with neurosarcoidosis. Therefore, familiarity with the variety of MRI appearances is important. The neurosarcoidosis include intracranial and spine leptomeningeal involvement, cortical and cerebral white matter lesions, corpus callosum involvement, sellar and suprasellar involvement, periventricular involvement, cranial nerve involvement, cavernous sinus involvement, hydrocephalus, dural involvement, ischemic lesions, perivascular involvement, orbit lesions, osseous involvement, nerve root involvement, and spinal cord intramedullary involvement. Neurosarcoidosis is apparent clinically in only about 5% of patients with sarcoidosis. However, less than 1% of patients have isolated central nervous system involvement. Cranial neuropathy, particularly facial nerve palsy, is the most common presentation. Other presentations of neurosarcoidosis include encephalopathy, peripheral neuropathy, meningitis, seizure, spinal cord dysfunction, and myopathy.
- 70. Leptomeningeal involvement occurs in 40% of patients with neurosarcoidosis. The basilar meninges are most frequently involved. Gadolinium enhancement can be diffuse or nodular on post-contrast T1-weighted magnetic resonance imaging (MRI).Perivascular spread can be encountered, producing enhancing foci that are remote from the brain surface. Leptomeningeal Involvement. (a) Pre-contrast T1, and (b) post-contrast axial, and (c) coronal sequences show widespread leptomeningeal thickening and enhancement along the convexities of the brain (arrowheads). Both diffuse and nodular patterns are evident.
- 71. Sarcoidosis, Meningeal involvement in a 32-year-old man who presented with blurred vision in his right eye, with subsequent weight loss, CSF lymphocytosis and protein >2 g/l. a and b show sagittal and coronal T1W gadolinium-enhanced brain MRI with extensive leptomeningeal enhancement, especially in the basal meninges, and including the optic chiasm (arrowed) and the upper cervical meninges.
- 72. Leptomeningeal sarcoidosis of brain. T1-weighted axial images from caudal to cranial (A, B), obtained after contrast administration shows enhancement involving basilar cisterns, Sylvian fissures and cortical sulci (white arrows).
- 73. Neurosarcoidosis in a 28-year-old man. On MRI, axial T1WI demonstrates isointense lesions in typical locations, which demonstrates enhancement on contrast-enhanced T1WI (arrows), a finding that suggests biological activity.
- 74. Intraparenchymal mass lesions: Parenchymal mass lesions or granulomas are a fairly common manifestation of neurosarcoidosis, with 35% of cases presenting as multiple supratentorial and/or infratentorial masses and 15% as solitary masses. These lesions are often intimately associated with leptomeningeal involvement and may represent centripetal spread of the disease. Intraparenchymal masses typically show enhancement. Initially, the lesions can be hypointense on T2, but are otherwise hyperintense. Central necrosis is rare. (a) Axial T2 and (b) post-contrast T1sequences show numerous cortical and subcortical white matter lesions in the bilateral cerebral hemispheres, which are hyperintense on T2 (arrows) and demonstrate enhancement.
- 75. Sarcoidosis, a and b, axial T2W and gadolinium-enhanced T1W brain images with multiple, extensive white-matter periventricular and subcortical enhancing lesions, some of which are large (arrowed).
- 76. Pituitary and hypophyseal involvement: The pituitary gland, infundibulum, or hypothalamus are affected in 18% of patients with neurosarcoidosis. Cystic masses, enhancing masses, or thickening and enhancement of the infundibulum can be encountered on imaging. These findings may occur in isolation or in combination with basilar leptomeningeal involvement. (a) Sagittal and (b) coronal images of pituitary and hypothalamus Involvement. There is extensive enhancement of the pituitary gland (arrow) and stalk (arrowhead), which is markedly enlarged.
- 77. Mid sagittal contrast-enhanced T1-weighted brain magnetic resonance image demonstrating a gadolinium-enhancing mass of the floor of the third ventricle and hypothalamus (arrow).
- 78. Sarcoidosis, T1W gadolinium-enhanced coronal MRI showing a thickening and enhancement of the dural sheath of the right optic nerve (a, arrowed). Widespread dural enhancement with focal thickening of the meninges over the convexity and the left temporal region is also seen (b, arrowed).
- 79. Cavernous sinus involvement: The cavernous sinus is rarely involved in neurosarcoidosis. These lesions can produce cavernous sinus syndrome, which include painful ophthalmoplegia. Lesions enhance and may have a dural tail. Cavernous Sinus Involvement. (a) Axial T2 magnetic resonance imaging (MRI) scan shows a hypointense lesion in the right cavernous sinus (arrowheads). (b) Axial and (c) coronal post-contrast T1-weighted sequences show that the enhancing mass in the right cavernous sinus (arrowheads). The carotid artery is patent.
- 80. Hydrocephalus: Hydrocephalus occurs in 5% to 12% of patients with neurosarcoidosis. The hydrocephalus is usually communicating secondary to leptomeningeal/dural involvement. However, obstructive hydrocephalus can result secondary to ventricular system adhesions or loculations, which may cause trapped ventricles. There may be altered signal intensities of the cerebrospinal fluid in the isolated ventricle due to elevated protein concentrations. Hydrocephalus. Axial T2-weighted sequences at the level of the (a) fourth ventricle and (b) lateral ventricles show dilatation of these structures.
- 81. Dural involvement: Dural involvement occurs in 34% of patients with neurosarcoidosis. The posterior fossa is most commonly involved. Lesions are usually hypointense or isointense on T2. There can be strong enhancement of the thickened dura. Dural Involvement. There is (a) hypointense T2 and (b) isointense T1signal in the (c) symmetrically thickened frontal lobe dura, which avidly enhance on post-contrast T1 MRI (arrowheads).
- 82. Cranial nerve involvement: Cranial nerves are affected in up to 50% of patients with neurosarcoidosis. There is poor correlation between imaging findings and clinical symptoms. While facial nerve deficits are most commonly found clinically, the optic nerve is the most common cranial nerve to appear abnormal on MRI. Affected cranial nerves show enhancement and thickening with or without associated leptomeningeal involvement. Cranial nerve involvement. (a) Coronal post-contrast T1-weighted MRI shows peripheral enhancement of the bilateral cisternal segments of cranial nerve II. (b) Axial post-contrast T1- weighted sequences at the level of cranial nerve V, (c) cranial nerves VII and VIII, and (d) cranial nerve IX show thickening and enhancement of multiple cranial nerves (arrowheads).
- 84. Spine intramedullary involvement: Intramedullary involvement occurs in up to 25% patients with of neurosarcoidosis. Lesions cause fusiform cord enlargement, mainly in the cervical and thoracic regions. Typically, there is low T1 signal, high T2 signal, and patchy enhancement on MRI. Intramedullary spinal cord involvement. (a) Sagittal T2, (b) sagittal T1 and (c) sagittal post- contrast T1 sequences is high T2 signal within the spinal cord (arrowheads). A portion of the lesion demonstrates intense enhancement (arrowhead). The cord is mildly expanded.
- 85. MR images show spinal cord involvement in a 54-year-old male. T2-weighted image (a) demonstrates an extensive area of edema in the spinal cord (white arrow); unenhanced T1-weighted image (b) only shows swelling of the spinal cord. On enhanced T1-weighted acquisitions, a peripheral enhancement (curved white arrow) can be depicted (c), suggesting meningeal involvement.
- 86. Sagittal T1-weighted magnetic resonance image of the spinal cord showing an intramedullary gadolinium-enhancing mass responsible for cordal enlargement (arrow).
- 87. Sarcoidosis, a T2W sagittal MRI showing focal area of abnormal high signal at C5–C6. b T1W gadolinium enhanced image shows focal contrast enhancement at that level (same area indicated by an arrow on each image).
- 88. Spinal leptomeningeal sarcoidosis. Contrast-enhanced sagittal T1-weighted image of the cervical spine shows linear and multiple nodular enhancing lesions along surface of spinal cord and on spinal nerve roots (thin white arrows). Post contrast axial T1-weighted image of the thoracic spine demonstrates nodular leptomeningeal deposits (thick white arrows) with enlarged subcarinal and left hilar lymph nodes (arrowheads) and bilateral pleural effusion (hollow white arrows).
- 89. Sarcoidosis, involving spinal cord and the brain.
- 90. Spine nerve root enhancement: Infiltration of spinal nerve roots is uncommon in neurosarcoidosis. These lesions can cause polyneuropathies. On MRI, nodularity or diffuse thickening of the affected nerve roots can be encountered. Nerve root enhancement is also a common feature. Spine nerve root involvement. (a) Sagittal T2 and (b) post-contrast T1 sequences demonstrate high T2 signal within the spinal cord (arrowheads). A portion of the lesion demonstrates intense enhancement (arrowhead). The cord is mildly expanded.
- 91. Orbital manifestations of sarcoidosis are common among patients with systemic sarcoidosis and can involve the lacrimal gland, the orbit, soft tissues of the orbit, and the optic nerve. Uveitis is by far the most common manifestation and is typically bilateral.
- 92. Lacrimal gland involvement: The lacrimal gland is rarely involved in sarcoidosis. Imaging features on computed tomography (CT) scan include bilateral, asymmetric enlargement with intense enhancement of the lacrimal gland. The gland maintains its anatomic configuration. A portion of the gland may extend medially along anterior border of the globe. MR demonstrates hypointense T1 and T2 signal within enlarged glands that also show intense enhancement. Lacrimal gland involvement. Coronal post-contrast T1-weighted MRI shows bilateral intensely enhancing enlarge lacrimal glands (arrowheads).
- 93. Sarcoidosis, Thin-section (3 mm), fat-suppressed, gadolinium-enhanced axial (a) and coronal (b, c) T1-weighted sequences, showing bilaterally symmetrical diffusely enlarged lacrimal glands showing intense homogenous enhancement.
- 94. Cranial nerve enhancement in sarcoidosis. A and B, Axial fat-suppressed T1 images show enhancement of the left optic nerve (thin arrow). Lacrimal and parotid glands are enlarged (thick arrows in A and B, respectively). C, Bilateral trigeminal nerve enhancement is seen in a different patient (arrows). D, Enhancement of bilateral seventh-eighth nerve complexes is seen in another patient (arrows).
- 95. Sarcoidosis, Axial image of the orbits/head, T1 weighted, post-contrast, with fat suppression - nodular enhancement of right and left optic nerves.
- 96. Ophthalmic manifestations of sarcoid. Four gadolinium-enhanced T1-weighted images demonstrate the typical MRI appearances of ophthalmic sarcoid in different patients: (a) marked enlargement and enhancement of the lacrimal glands (thick arrows) secondary to sarcoid in filtration; (b) expanded enhancing optic nerve (arrowhead) typical for sarcoid in filtration (the differential includes meningioma and lymphoma; (c) marked enhancement of the subarachnoid portion of the oculomotor nerve on the left (thin arrows) typical for sarcoid; (d) mass- like enlargement of the superior and lateral rectus muscles (curved arrow) in a patient with proptosis. Features are typical of sarcoid, but this is indistinguishable from lymphoma and orbital pseudotumor on imaging.
- 97. Discrete orbital sarcoidosis. A, Clinical photograph of an 83-year-old female patient with a 2-month history of puffiness around left eye. Note the superior displacement of the left eye. B, Magnetic resonance imaging scan shows a localized soft tissue mass in the left anterior inferior orbit (arrow). C, Axial computed tomographic scan of the same patient shows thickening around the left optic nerve (arrow). Diffuse orbital sarcoidosis. A, Clinical photograph of a 63-year-old male patient with a 5-week history of lid swelling in the right eye. B, Magnetic resonance imaging scan demonstrates a diffuse soft tissue mass involving the superior and medial quadrants and enveloping the globe.
- 98. Sarcoidosis, Axial (A) and coronal views (B) of T1-weighted MRI of the orbits show enlargement of multiple extraocular muscles with tendon involvement at the time of presentation. Clinical photographs before (C) and after (D) initiation of corticosteroid therapy show marked improvement in lid edema, chemosis, and conjunctival erythema.
- 99. Muscle-skeletal sarcoidosis The skeleton is affected in about 1-13% of patients with generalized disease, complaining of bone and joint pain. Sarcoidosis usually involves the phalanges of the hands and feet; conventional radiography, performed in symptomatic patients, demonstrate either "lacy" osteolytic or osteosclerotic multiple lesions, where the latter is less frequent. Large bones and axial skeleton involvement is uncommon. In large bones, lesions usually demonstrate a lytic appearance with indistinct or well-defined margins at conventional radiography. In the vertebrae, both osteolytic lesions with sclerotic borders and diffuse osteosclerotic localizations are possible [13, 19-20]. Lesions can be located in one or more contiguous or non- contiguous vertebrae and they can also affect the pedicles. Patients may complain of arthralgia in knees, ankles, elbows and wrists, but joint radiograms are usually negative or demonstrate non-specific signs of osteoporosis and soft-tissue swelling. These lesions usually demonstrate an uptake on bone scintigraphy, even before the lesions are visible at conventional radiograms. The use of CT and MRI is rare and it is usually performed to help differential diagnosis from other pathologies with skeletal involvement, such as osseous metastases, lymphoma, myeloma and tuberculosis. Sarcoidosis may also affect the muscles with myopathic or nodular type involvement. On MR, sarcoid nodules show hypo-intense fibrotic central areas, with marginal peripheral areas hyper-intense on T2-weighted images with enhancement after gadolinium. These appearances may mimic a soft-tissue tumor. In the myopathic type, the involved muscles demonstrate a high signal intensity on T2-weighted images.
- 100. Osseous involvement: Although osseous involvement occurs in up to 13% of patients, skull and vertebral involvement in neurosarcoidosis is very rare. The intervertebral body disc spaces can also be affected. Lesions are usually lytic with a punched-out appearance, but can also be sclerotic. The osseous lesions can also show increased activity on bone scans. On MRI, bone lesions are typically hyperintense on T2 and post-contrast T1. However, sclerotic lesions appear hypointense and may not enhance Vertebral involvement. (a) Sagittal T2 and (b) post-contrast T1 sequences show a hyperintense, enhancing focus on the posterior elements of the thoracic spine (arrowhead). There is also enhancement of the interpinous ligaments (*) and posterior extradural enhancement (arrow).
- 101. Skull Involvement. (a) Sagittal post-contrast T1-weigthed MRI shows multiple non- enhancing hypointense intraosseous skull lesions (arrowheads). (b) The corresponding axial CT image shows that the lesions are sclerotic (arrowheads).
- 102. Axial skeleton involvement of a 49 year-old female. Axial CT images (a, b and c) show multiple diffuse osteosclerotic lesions in cervical, lumbar and sacral vertebrae; sagittal (d) and coronal (e) reconstructions demonstrate lesions in contiguous and noncontiguous vertebrae.
- 103. Bone sarcoidosis in a 25-year-old man who presented with bilateral thumb pain. Close-up views from radiograph of the both hands reveals radiolucent lesions in the middle phalanx of the fifth finger of right hand and in the distal and middle phalanges of the left hand, this one involving the joint. The lesions have a "lace-like" appearance.
- 104. Small bone sarcoidosis. Close-up view from a postero-anterior radiograph of the finger shows sarcoidosis with the classic lacy lytic pattern involving the middle phalanx. The articular surface is spared.
- 105. Small bone sarcoidosis in a 53-year-old woman with a 12-year history of painful swelling of the digits. (a) Axial T2-weighted MR image (repetition time msec/echo time msec = 4,000/85) demonstrates swelling of the fifth finger with destruction of the cortex of the proximal phalanx. Periosseous extension of presumed sarcoidosis nodules with intermediate signal intensity is also seen (arrow). (b) Axial fat-saturated proton-density-weighted MR image (1,200/20) of the digits reveals a conglomerate nodular mass with bright signal intensity infiltrating the fifth proximal phalanx and destroying the cortex. (c) Coronal T1-weighted MR image (500/20) demonstrates a low-signal-intensity intramedullary mass of the fifth digit with fine perpendicular lines extending from the ghost of the cortex. Although this finding resembles periosteal reaction, it may represent periosseous extension of granulomas separated by fibroblasts and collagen. (d) Coronal fat- saturated proton-density-weighted MR image (2,000/22) also demonstrates fine perpendicular lines extending from the intramedullary lesion.
- 106. Large bone sarcoidosis in a 48-year-old man with left hip pain. (a) Anteroposterior radiograph shows the normal pelvis. (b, c) Coronal T1- weighted (450/8) (b) and fat-saturated intermediate-density-weighted (2,000/15) (c) MR images demonstrate numerous discrete round lesions within the lumbar vertebrae, the pelvis, and both proximal femurs. As seen here, these lesions typically have low signal intensity on T1- weighted images and bright signal intensity on fat-saturated proton-density-weighted images.
- 107. Large bone sarcoidosis in a 53-year-old woman with bilateral heel pain. The patient’s medical history was unknown. (a) Sagittal T1- weighted MR image (450/10) demonstrates a round, low-signal- intensity lesion that involves the plantar aspect of the calcaneous. Biopsy of a lesion of the contralateral calcaneous (not shown) revealed non caseating granulomas and led to further clinical evaluation, results of which confirmed systemic sarcoidosis. (b) Lateral radiograph of the ankle reveals a faint area of increased opacity in the area of the lesion seen at MR imaging, with no radiographic evidence of trabecular or cortical disruption. The radiograph was interpreted as normal. (c) Sagittal fat-saturated T1-weighted MR image (650/8) obtained after the intravenous administration of gadopentetate dimeglumine shows an indistinctly marginated area of enhancement with a central area of spared marrow in the contralateral calcaneous (arrow).
- 108. Sarcoidal arthropathy Left ankle demonstrates tenosynovitis of the peroneal tendon sheath (left arrow) and tendinosis of the Achilles tendon (right arrow). A subtle focus of abnormal marrow signal intensity is noted in the distal fibula. Sarcoidal arthropathy On an axial contrast-enhanced fat- saturated T1-weighted MR image (500/10) of the distal forearm, the extensor tendon sheath is distended with fluid and shows synovial enhancement. Synovial biopsy revealed non- caseating granulomas.
- 109. Sarcoidosis of the muscle.
- 110. Breast sarcoidosis is rare and usually presents in patients with known sarcoid involving other organ systems. In the breast, sarcoidosis may mimic malignancy which must be excluded by core biopsy. Sarcoidosis. 72 years old with skin biopsy and chest radiograph consistent with sarcoidosis. US guided biopsy of a spiculated mass in the left breast was consistent with sarcoidosis. Fungal and acid fast bacilli stains were negative. A. (Right) and B. (Left) CC and CC Magnification: Multiple spiculated masses in both breasts, which were stable for 5 years.
- 111. Breast sarcoidosis in a 62-year-old woman. Cranio-caudal and medio-lateral views show a background mammographic pattern of scattered fibroglandular densities throughout both breasts, in a woman who had developed new nodular lesions diffusely distributed, predominantly in the right breast. All of them show rounded shape and partial ill-defined margins.
- 112. Sarcoidosis of the breast.
- 113. Sarcoidosis, Bilateral diagnostic mammogram with (a) MLO and (b) CC views demonstrates new spiculated masses throughout both breasts (arrows) which were all initially suspicious for carcinoma.
- 114. Axial MRI T1WI post contrast fat saturation subtracted images of the bilateral breasts (a) Breast sarcoidosis presents as multiple patchy bilateral areas of non-mass enhancement (arrows)
- 115. (Clockwise from top left – CT image, PET image, whole body maximum intensity projection PET image, CT/PET fusion image) Hypermetabolic primary breast malignancy and hypermetabolic skin thickening (arrows)
- 116. Cutaneous Sarcoidosis is a granulomatous disease characterized by the presence of noncaseating granulomas in organ tissue. Skin involvement is common, and a variety of therapeutic interventions have been utilized for the treatment of cutaneous disease. However, scientific support for most treatments for cutaneous sarcoidosis is limited to observational studies, uncontrolled prospective studies, small case series, individual case reports, and opinions of respected authorities. When managing patients with cutaneous sarcoidosis, clinicians must first consider whether treatment is indicated. The options available for the treatment of skin lesions include both local and systemic therapies.
- 120. Sarcoidosis most commonly affects the salivary glands are rarely involved and usually manifests in a variety of clinical patterns. They commonly presents as major salivary gland enlargement with only histopathological involvement of the minor salivary glands. The second clinical pattern is characterized by the absence of clinical salivary gland swelling with only histopathological involvement of minor salivary glands. Parotid gland involvement occurs in 0.5-15 % of patients of sarcoidosis and may manifest as unilateral or bilateral painless swelling.
- 121. The "panda sign" in radiogallium scintigraphy.
- 122. Sarcoidosis involving the parotid gland.
- 123. Sarcoidosis involving the parotid gland.
- 124. Cardiac sarcoidosis is a rare disease in which clusters of white blood cells, called granulomas, form in the tissue of the heart. Any part of the heart can be affected, though these cell clusters most often form in the heart muscle where they can interfere with the heart’s electrical system (conduction defects) and cause irregular heartbeats (arrhythmias). Cardiac sarcoidosis can also result in heart failure.
- 125. Cardiac sarcoidosis : A short-axis image of delayed-enhanced MRI reveals severe extent of hyper enhancement in septal, inferior, and anterolateral regions (white arrows). B and C, Cine MRI obtained at end diastole (B) and end systole (C) in a basal short-axis slice show wall motion abnormalities in septal and inferior walls (black arrows). Also see Movie I. D, A short-axis image of 201thallium single photon emission tomography demonstrates perfusion defects in septal and inferior regions (white arrows), where severe extent of enhancement is seen in a delayed enhanced MR image. E, A short-axis image of fasting FDG PET shows FDG accumulation in septal, inferior, and anterolateral walls (white arrows), corresponding to areas with late enhancement.
- 126. Gadolinium‐diethylenetriamine penta-acetic acid (DTPA) enhanced magnetic resonance imaging in the detection of cardiac sarcoidosis. Cardiac sarcoidosis produces zones of segmental wall thinning that enhances with gadolinium‐DTPA (arrow). The pattern of enhancement manifests mostly in the mid portion of the myocardium and is not typical of myocardial infarction.
- 127. Cardiac sarcoid in a 57-year-old woman who presented with 2nd degree heart block: (a) Short axis STIR image shows patchy areas of high signal intensity suggestive of myocardial edema, in the basal anterior and anteroseptal segments. (b) 2-chamber delayed enhancement image shows patchy areas of mid-myocardial enhancement in the mid-anterior segment, which is consistent with cardiac sarcoidosis. This was proven by endomyocardial biopsy
- 128. Sarcoid myopericarditis: 46-year-old male presented with chest pain and dyspnea. (a) Short axis T2-weighted image shows mild, diffuse circumferential pericardial thickening. (b) 2-chamber delayed enhancement image shows diffuse circumferential enhancement of the pericardium and subepicardial layer of the pericardium, which is consistent with a myopericarditis pattern, in this patient due to cardiac sarcoidosis.
- 129. Atypical presentation of cardiac sarcoid in a 62-year-old woman with history of heart block: (a) Short axis phase sensitive inversion recovery sequence show a full thickness transmural enhancement in the mid-part of antero- and inferoseptal segments. (b) Short axis phase-sensitive inversion recovery sequence shows wall thickening and transmural enhancement in the mid-inferolateral and inferior segments. Although the enhancement patterns are suggestive of an infarct, the patchy in a non-vascular distribution is suggestive of non-ischemic pattern of enhancement. Biopsy showed cardiac sarcoidosis
- 130. Unusual appearances of cardiac sarcoidosis in a 63-year-old man with biopsy confirmed pulmonary sarcoidosis: (a) Axial HASTE-MR image shows enlarged lymph nodes in the paratracheal and hilar regions. (b) 4-chamber delayed enhancement image shows near full thickness transmural enhancement in the basal lateral wall and patchy areas of enhancement in the septal segments. In addition, there is also patchy enhancement in the right ventricular myocardium. There is relatively low signal intensity in the blood pool. These appearances are suggestive of diffuse sarcoidosis
- 132. Cardiac MRI with T2-weighted STIR images (left panel) showing edema (arrow) and (middle and right panels) extensive patchy late gadolinium enhancement typical of sarcoid.
- 133. Diagnosis and treatment response evaluation of cardiac sarcoidosis using positron emission tomography/magnetic resonance imaging.
- 134. A to D, Imaging results from the 4 patients with probable cardiac sarcoidosis (ie, with high-degree atrioventricular block and findings in cardiac imaging typical for cardiac sarcoidosis despite negative endomyocardial biopsy findings. In each part, the top row of images shows a technetium-99m-tetrofosmin myocardial perfusion image, and the bottom row shows the corresponding 18F-2-deoxyglucose uptake. Every patient had a localized septal perfusion defect (*) with a super imposable hot spot on PET imaging suggestive of active inflammation. FDG F-18 indicates 18F-2-deoxyglucose; Tc, technetium-99m.
- 135. Thank You.