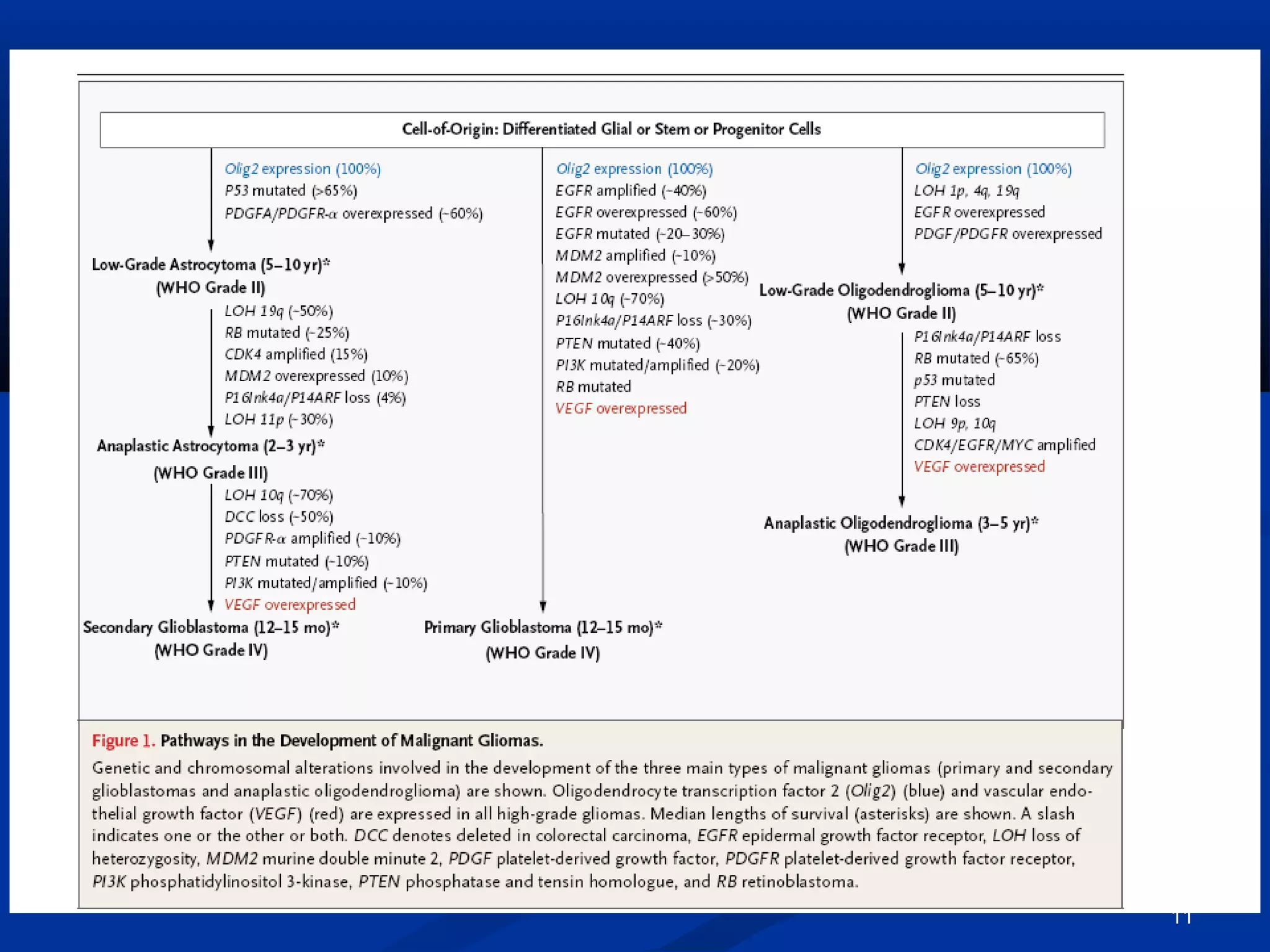
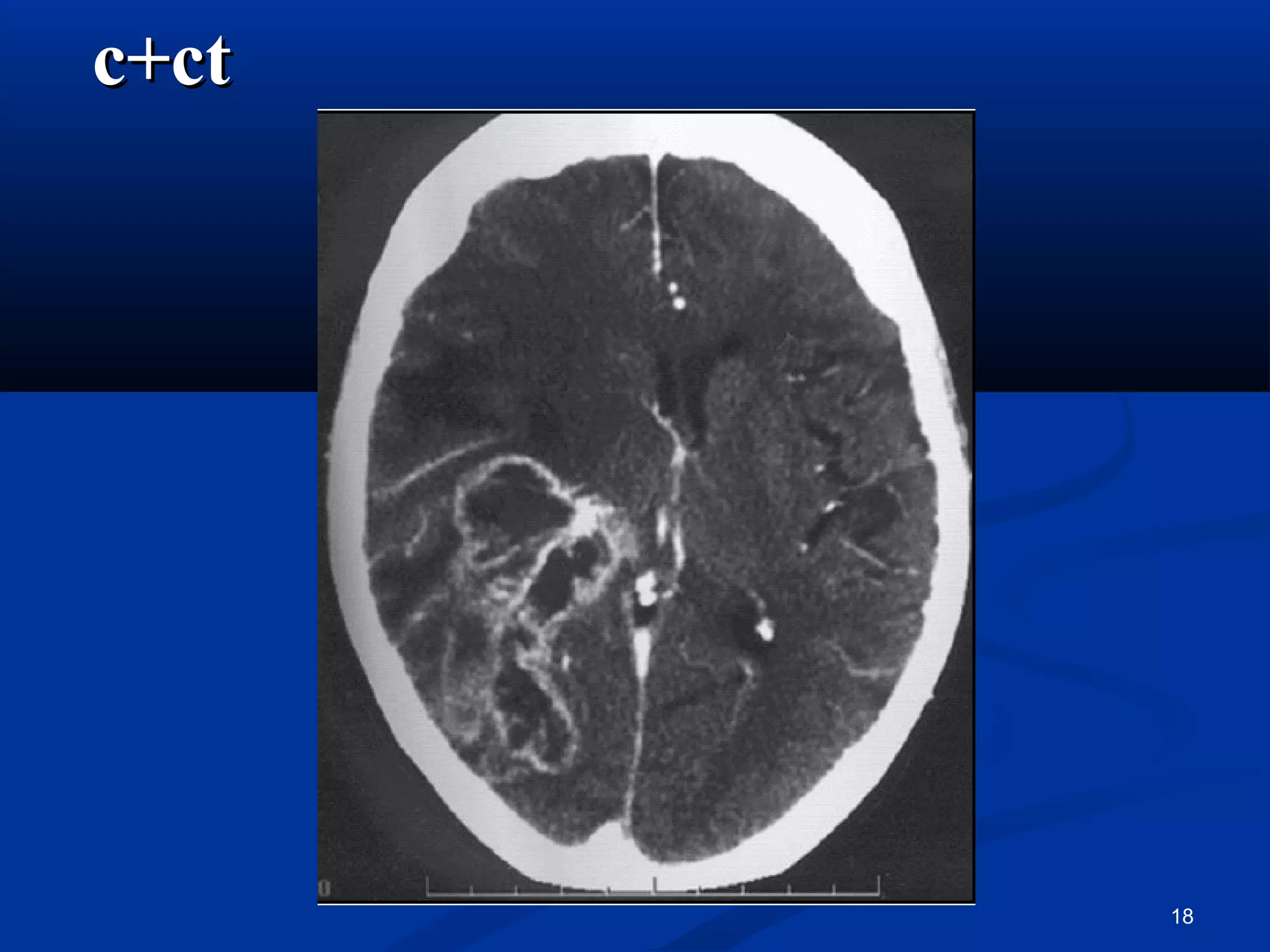
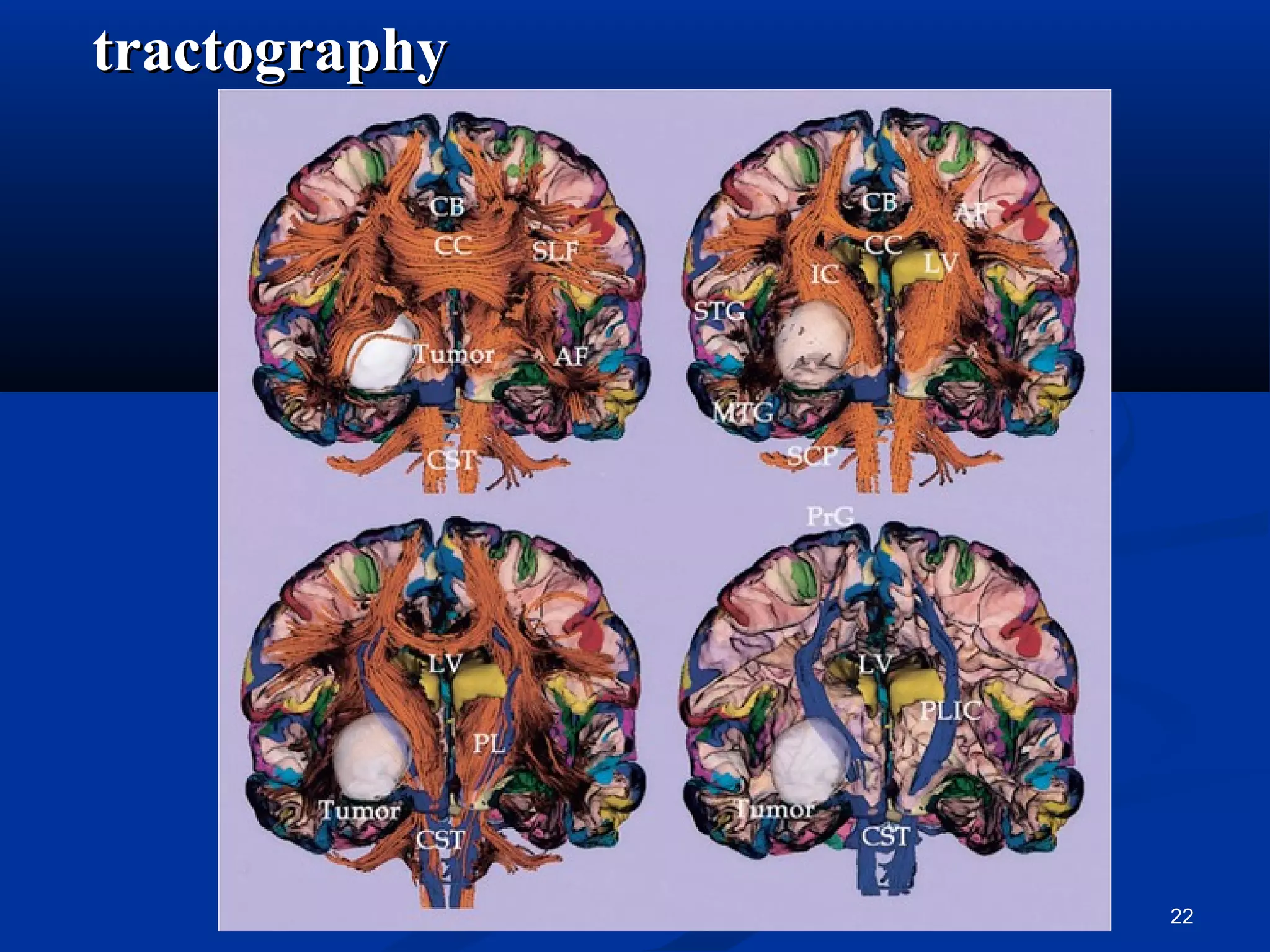
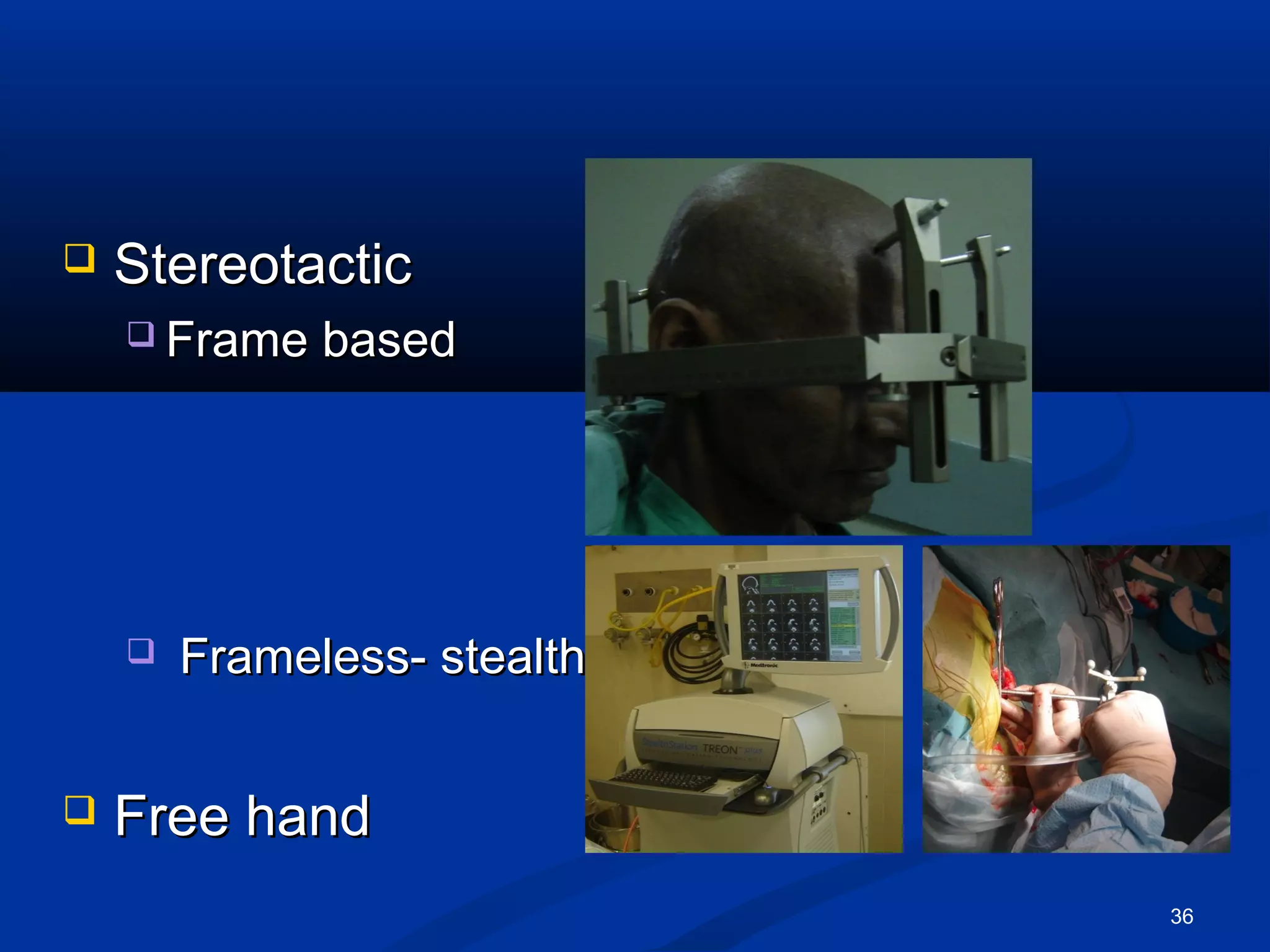
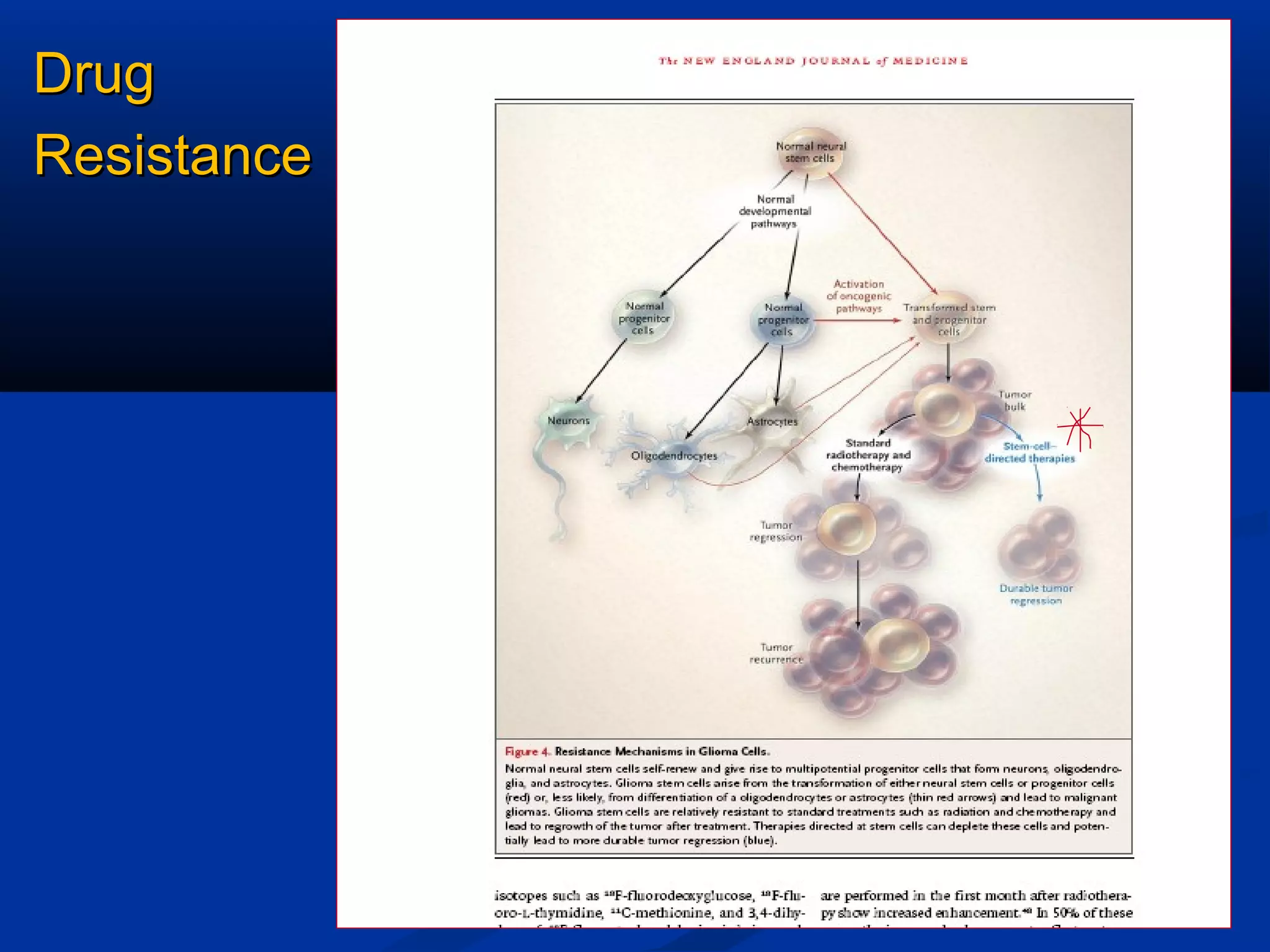
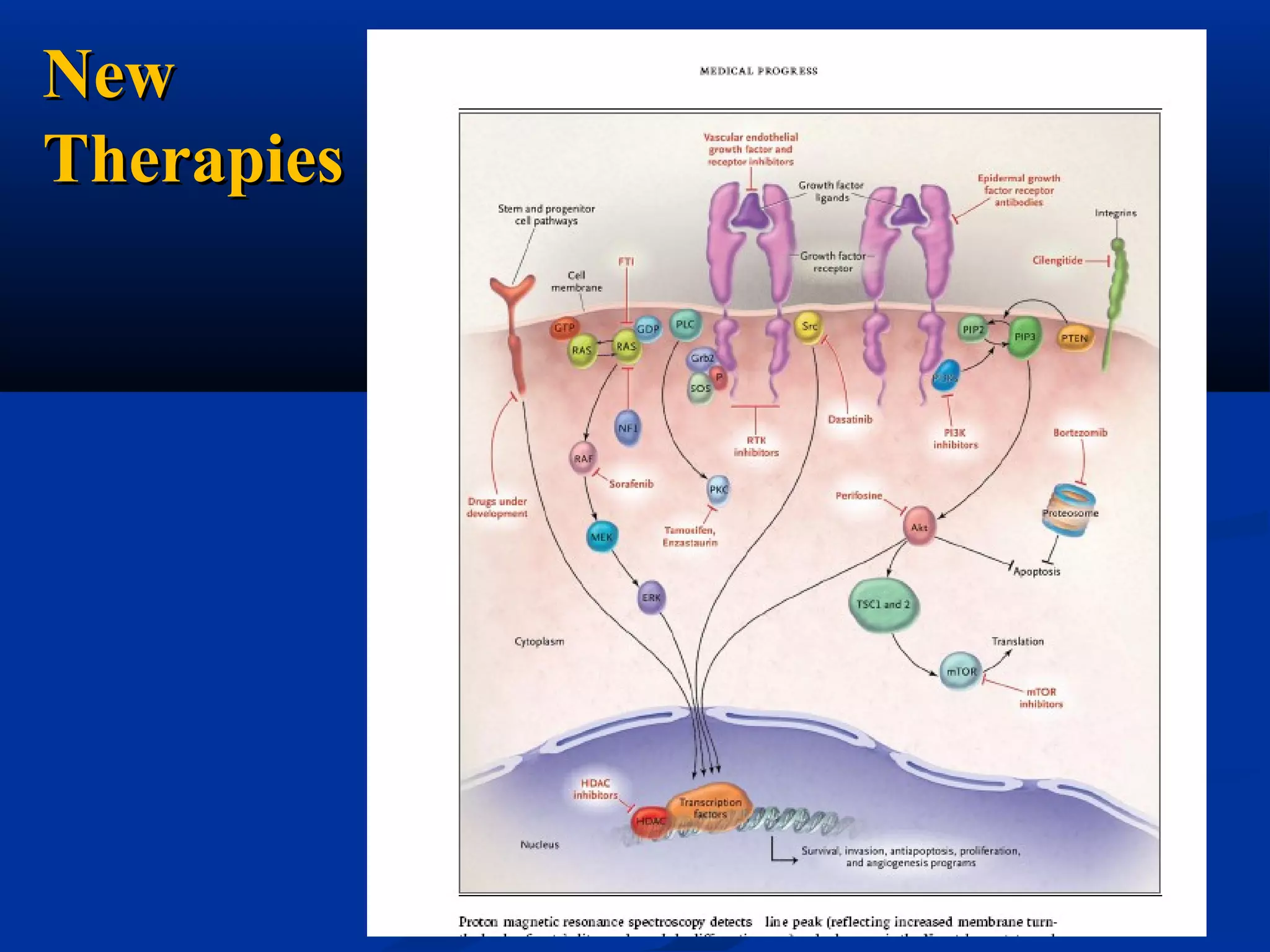
The document summarizes current management approaches for glioblastoma multiforme (GBM). It discusses the epidemiology, risk factors, clinical features, diagnostic testing, and treatment options including surgery, radiation, chemotherapy, and targeted therapies. The standard of care is maximal safe surgical resection followed by radiation therapy with concurrent and adjuvant temozolomide chemotherapy. Median survival remains approximately 12-15 months despite advances in multimodal management.