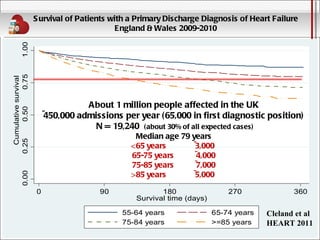
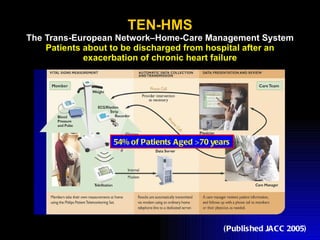
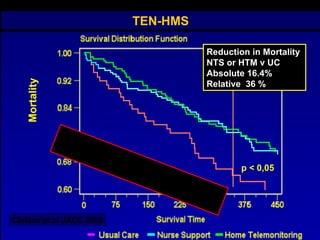
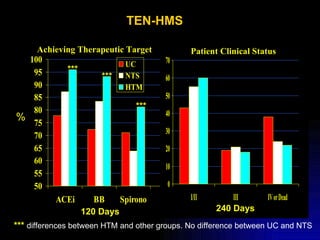
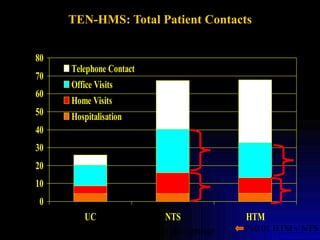
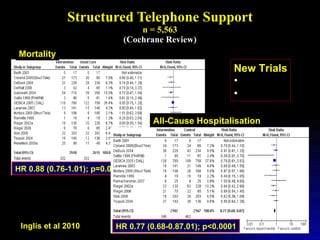
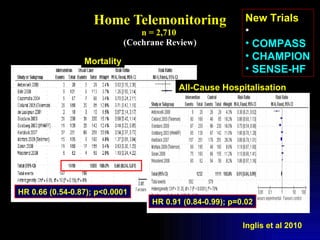
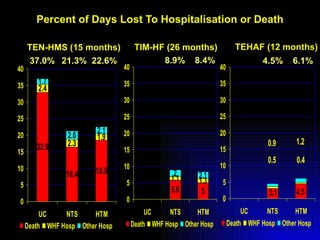
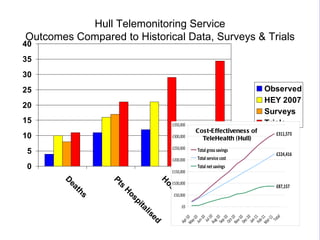
- Telemonitoring for heart failure patients has been shown to reduce mortality rates by up to 36% and decrease hospitalization rates in studies such as TEN-HMS and the Cochrane review.
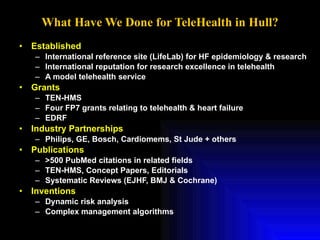
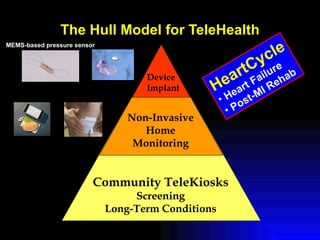
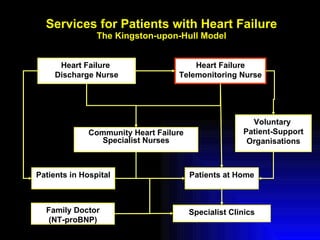
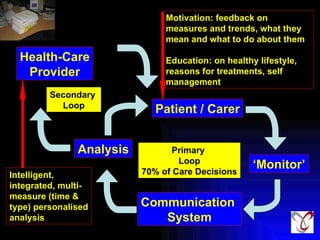
- The Hull model of telemonitoring in the UK involves a comprehensive system of care including home monitoring devices, community kiosks, and support from nurses and specialist clinics to closely manage heart failure patients.
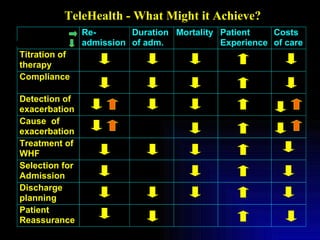
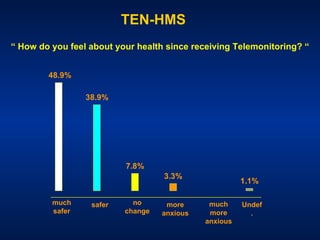
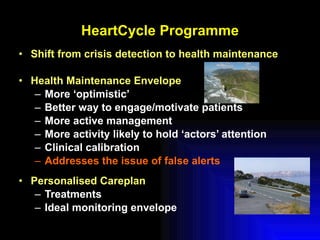
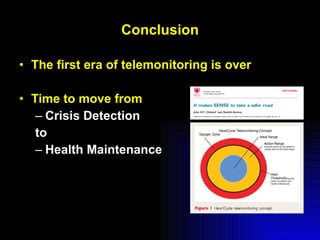
- Further research and investment in telemonitoring technologies could help shift care from crisis management to proactive health maintenance and empowering patients to better self-manage their condition.