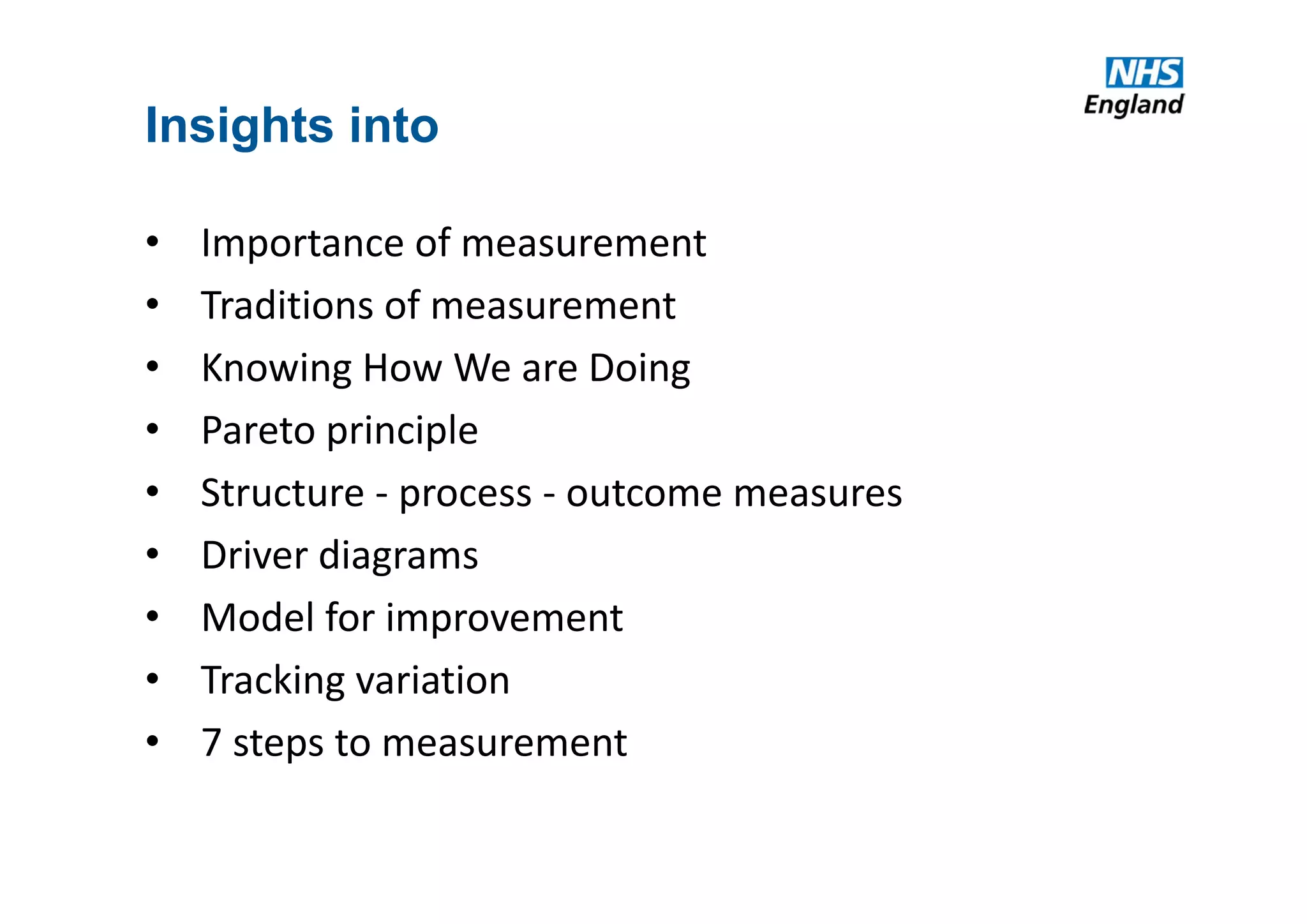
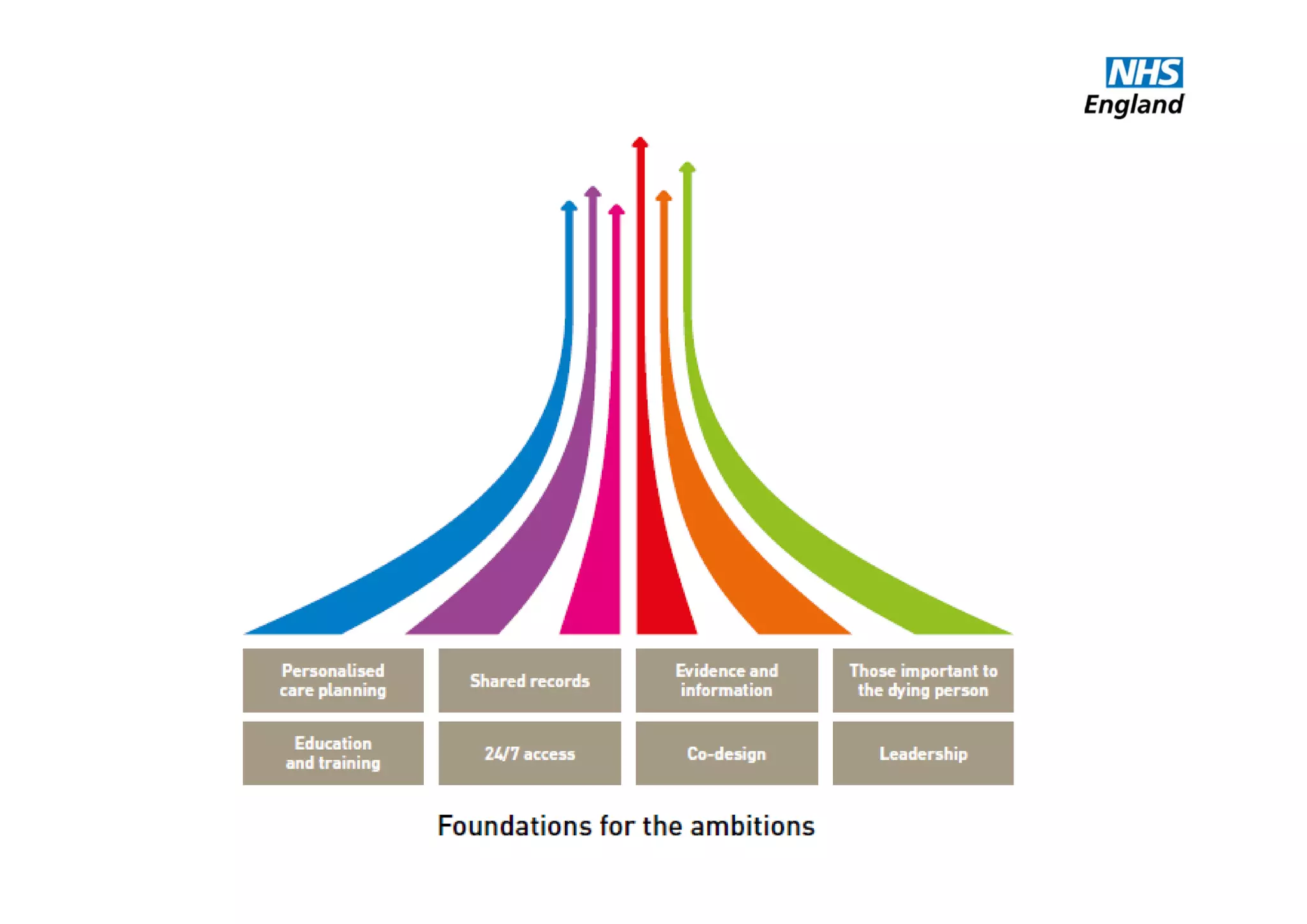
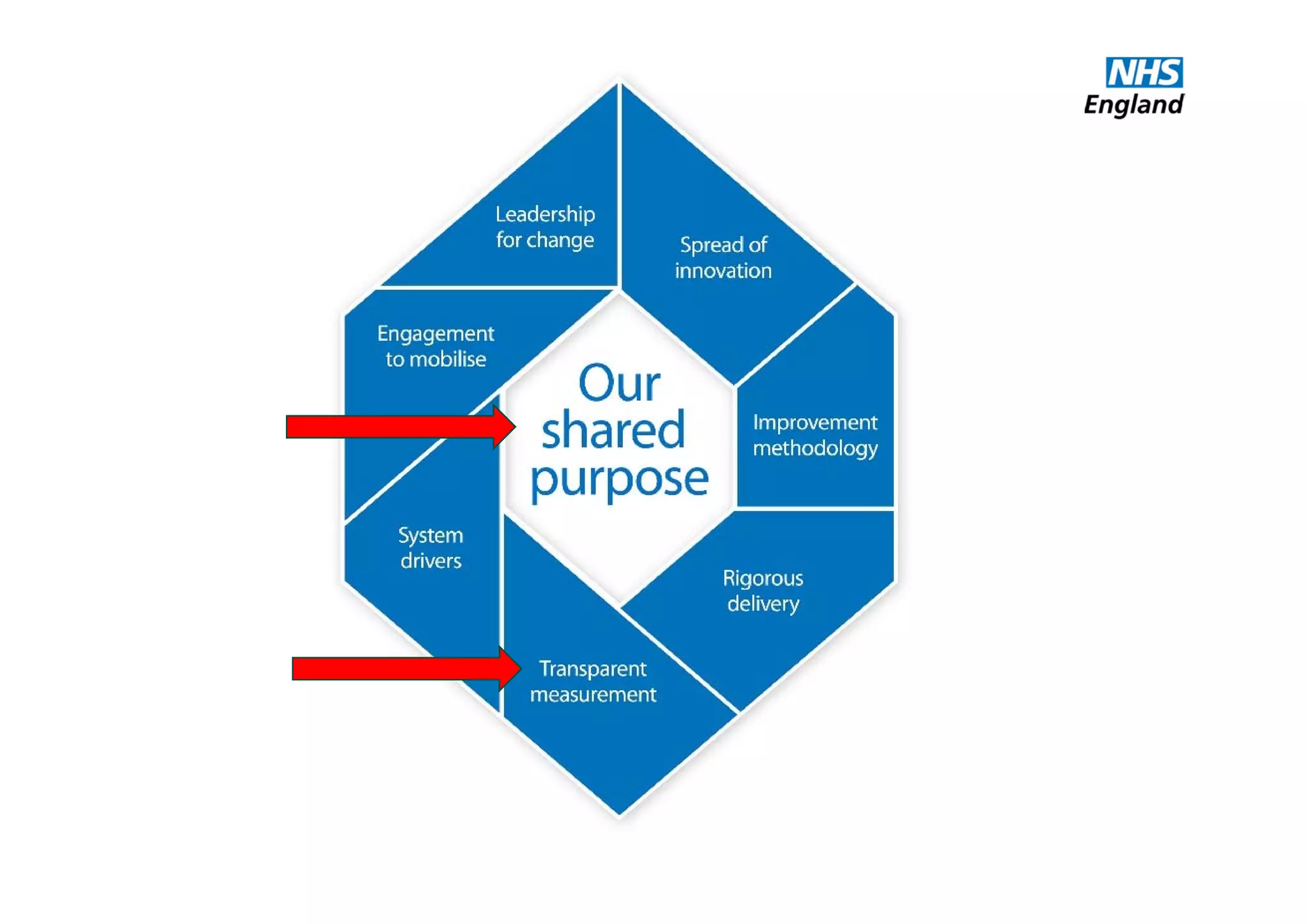
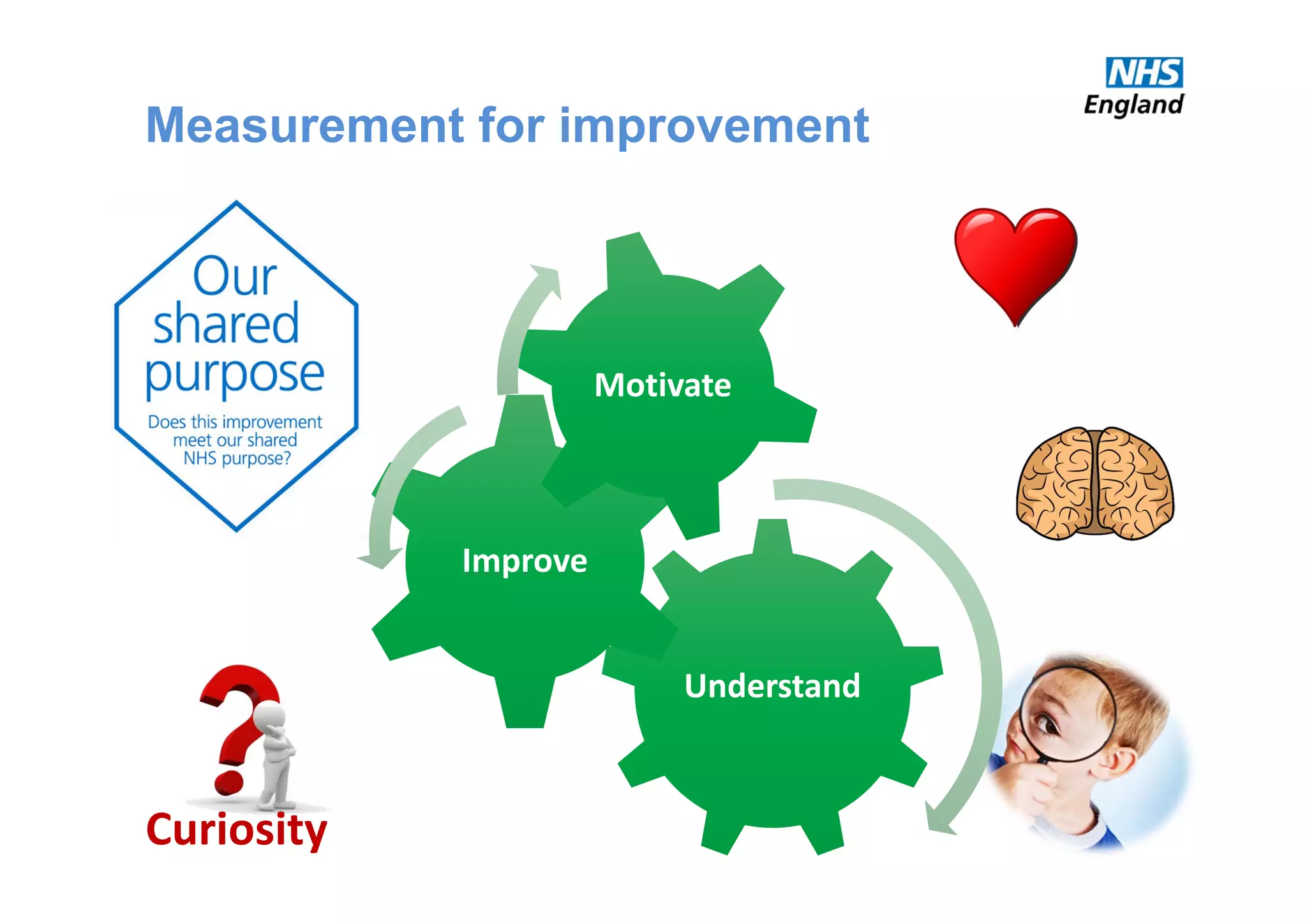
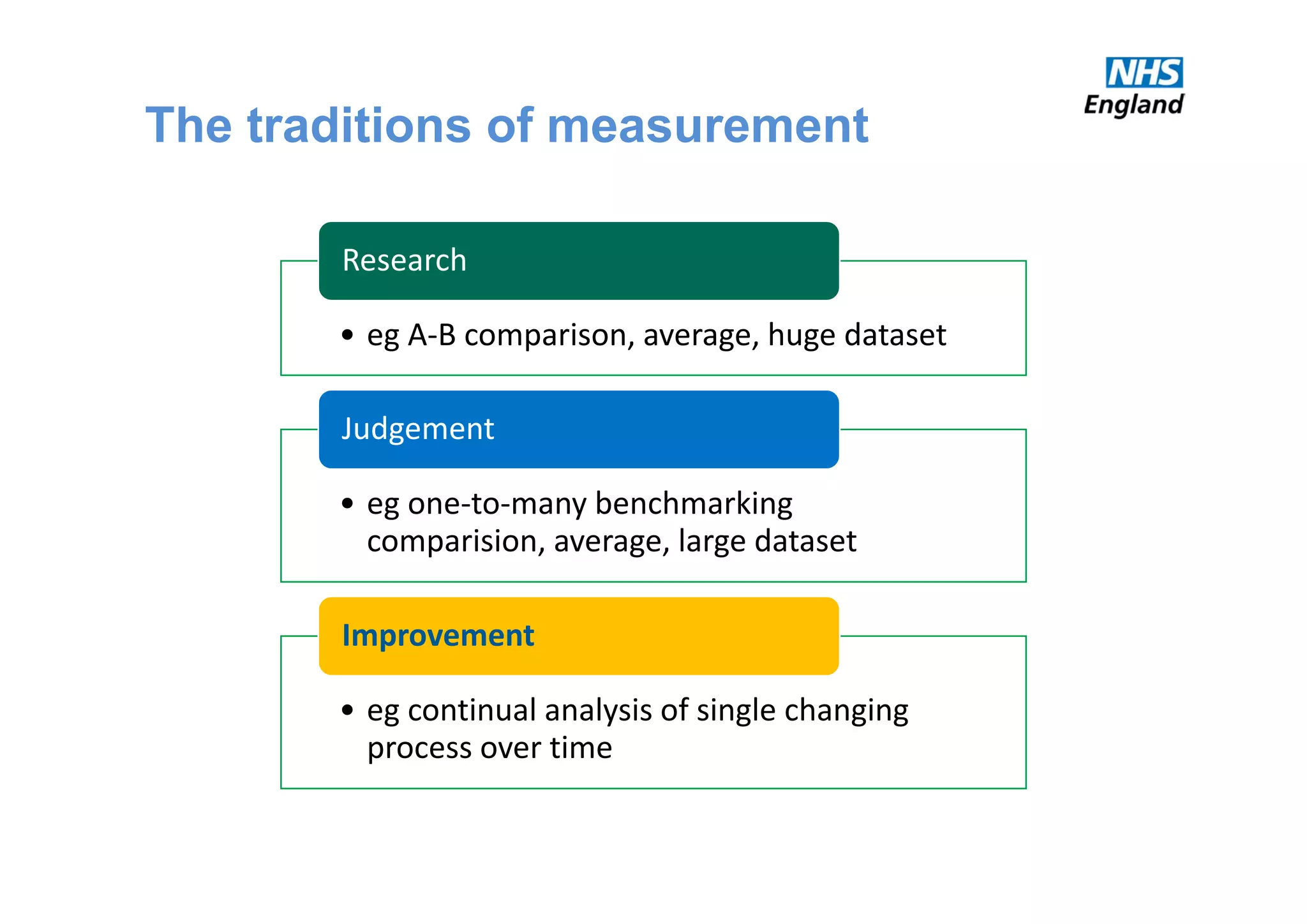
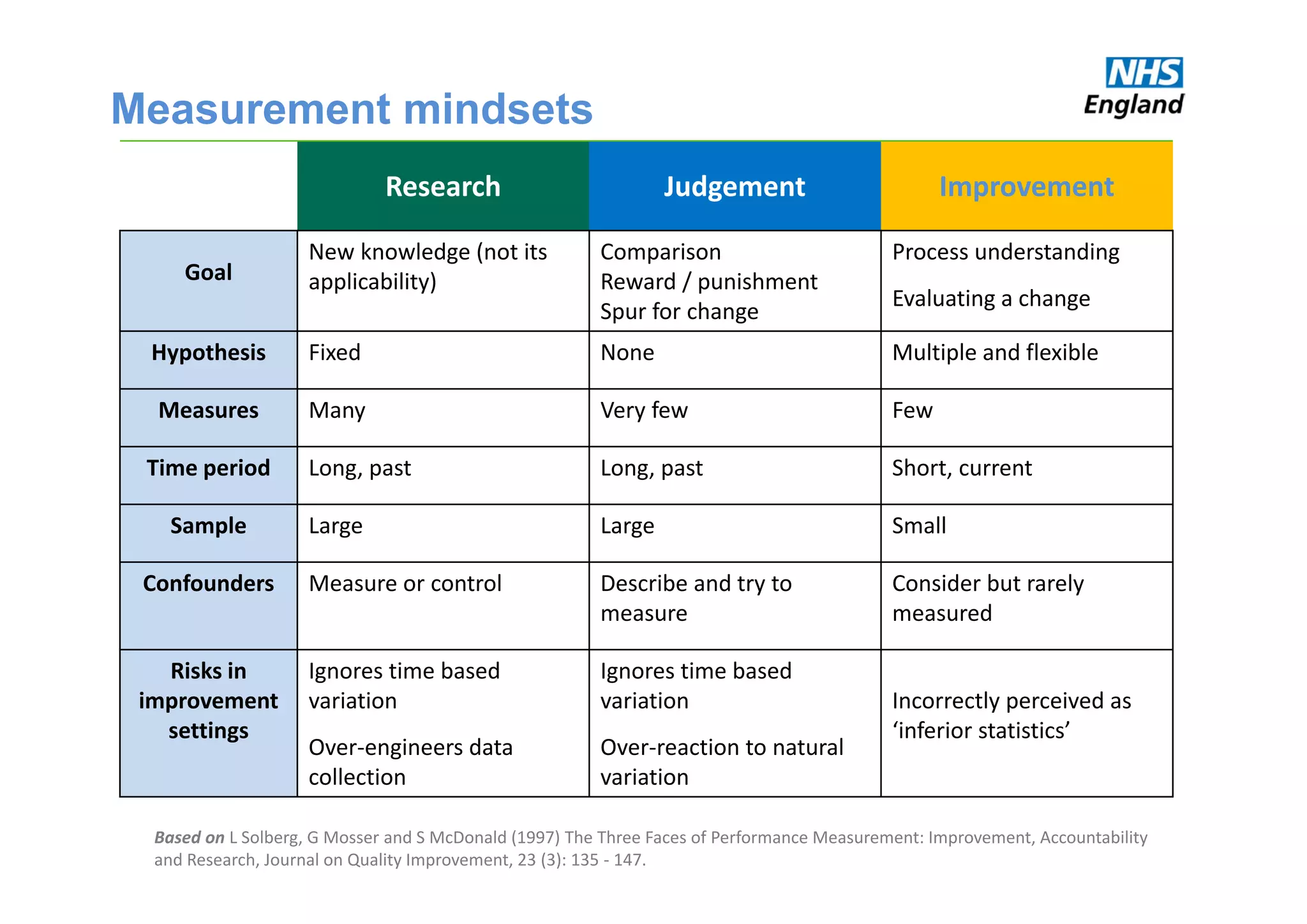
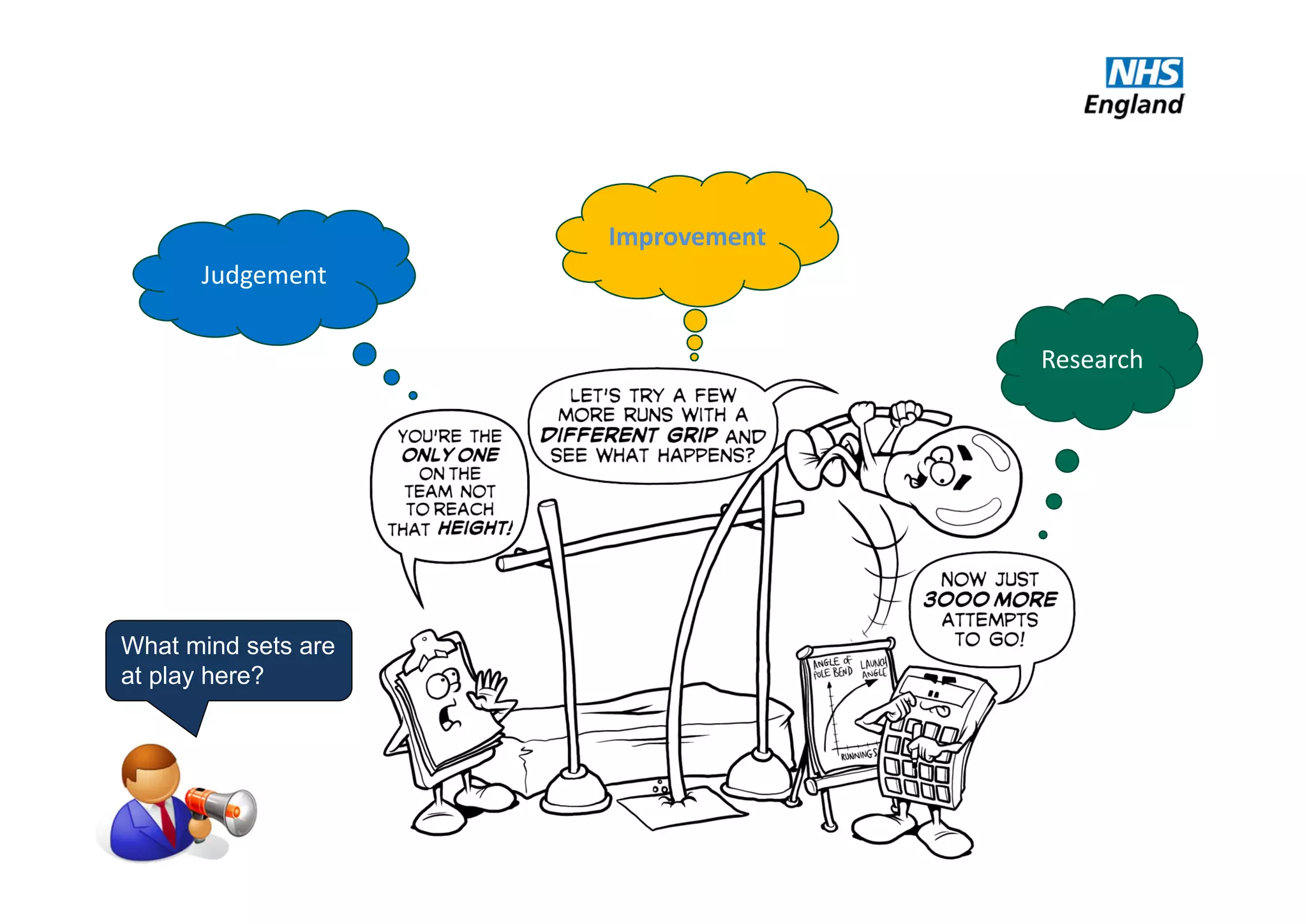
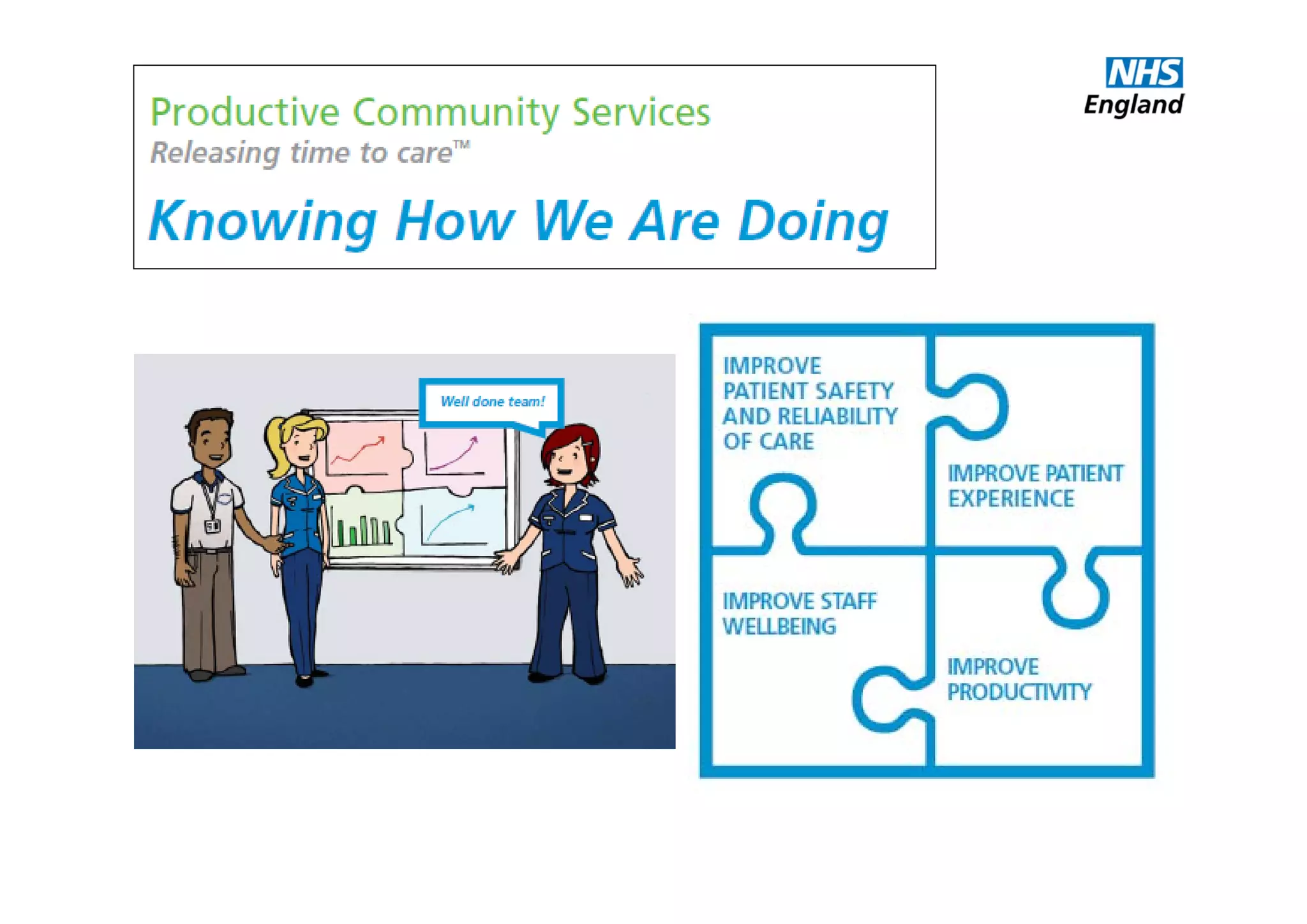
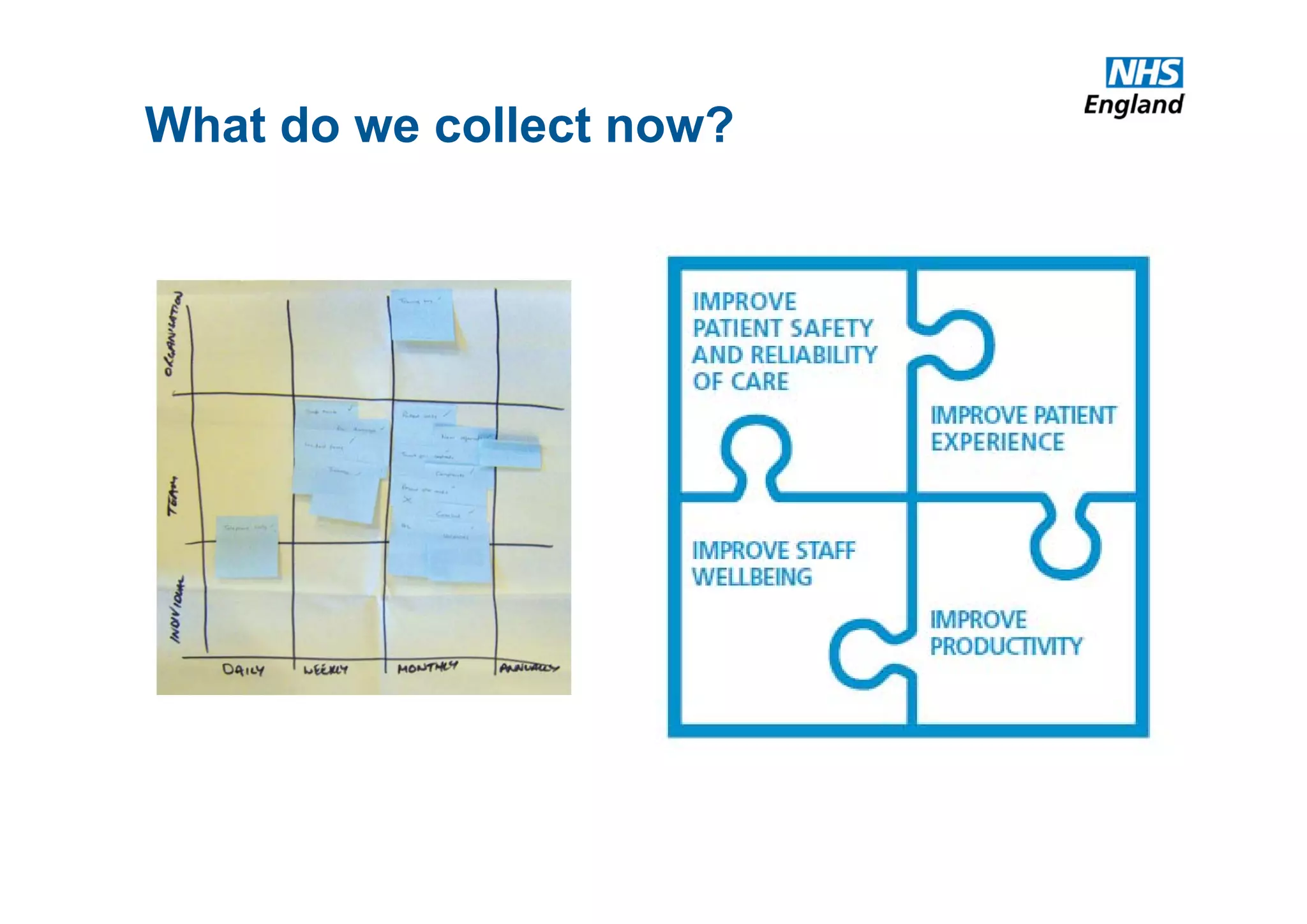
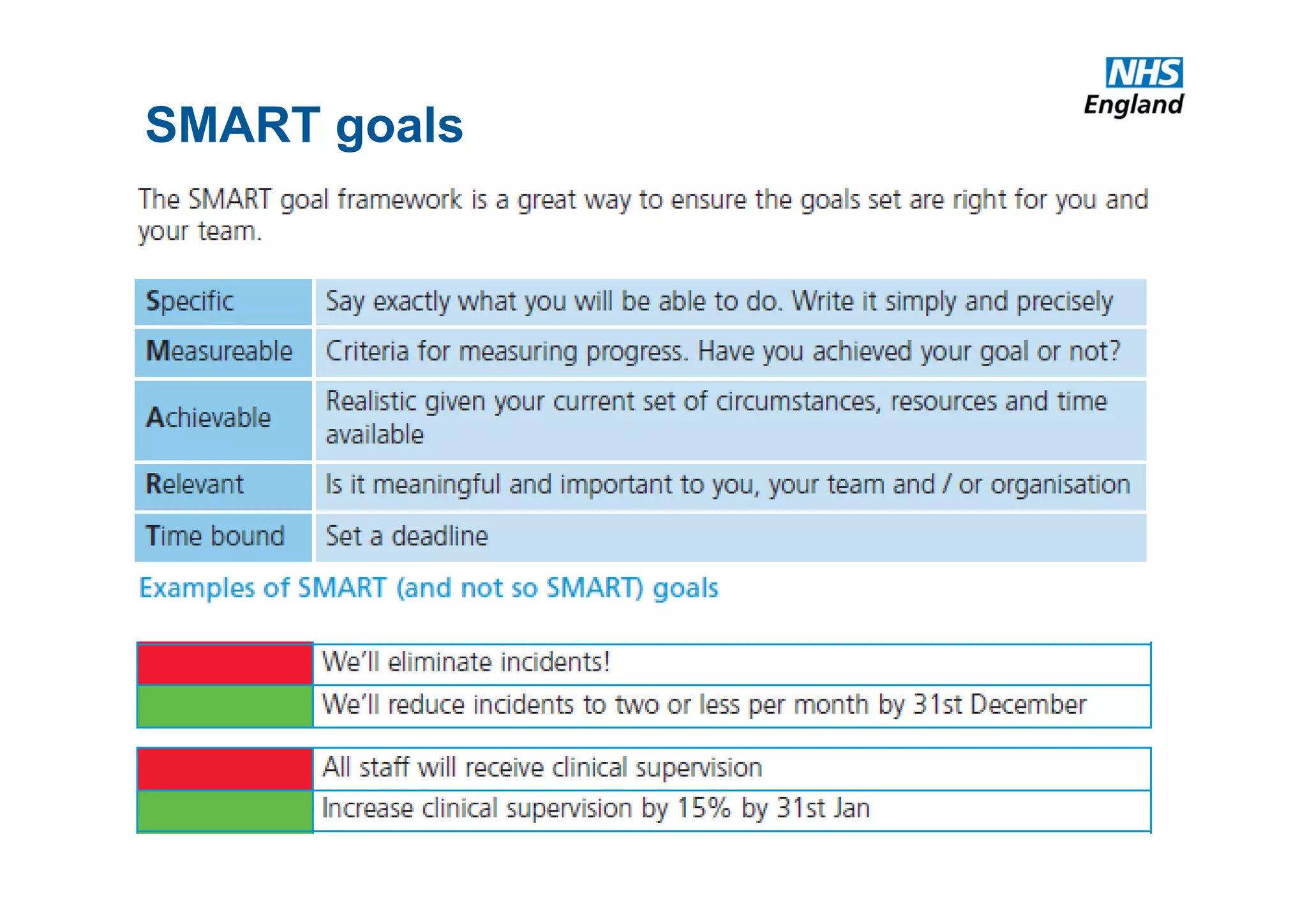
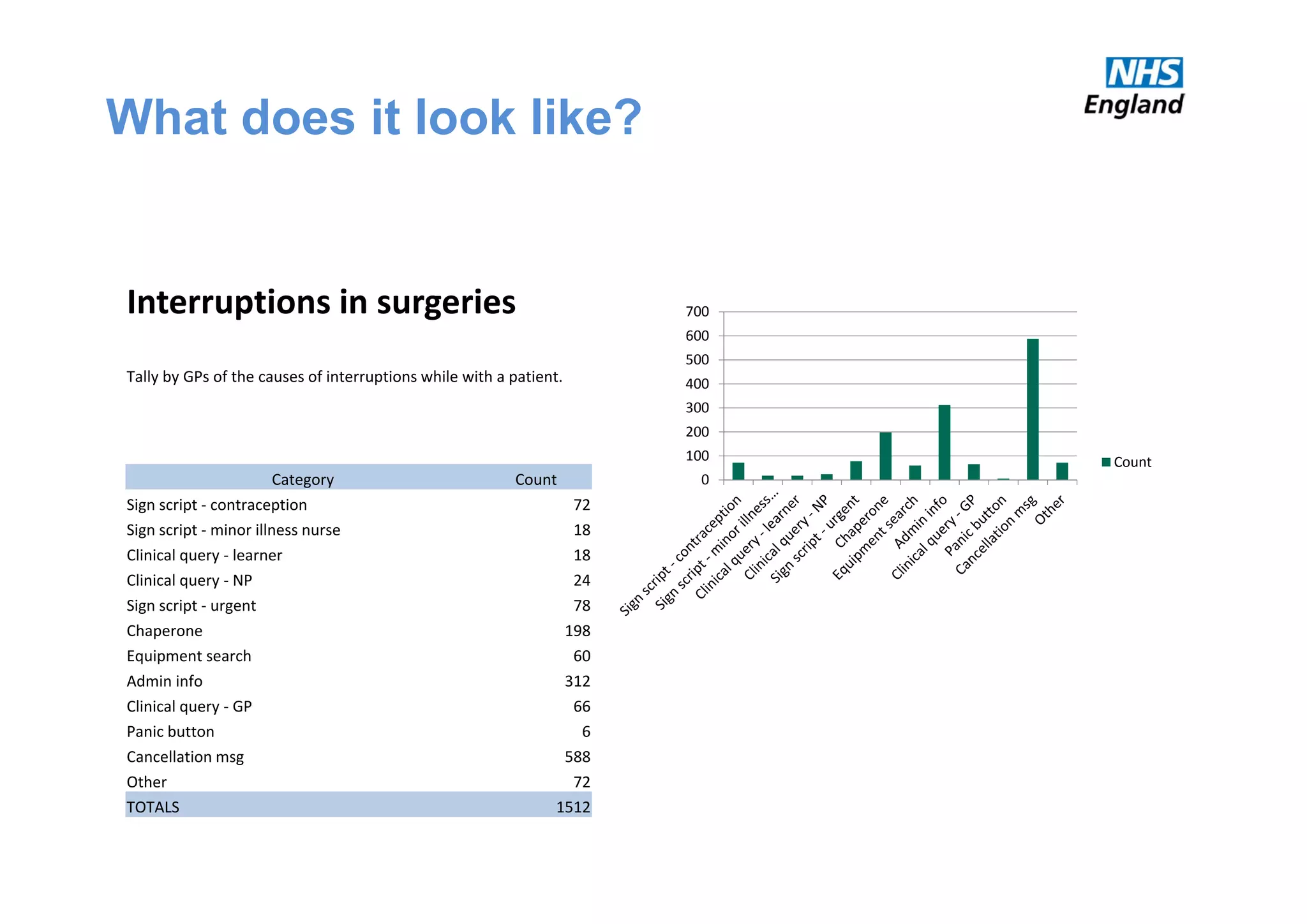
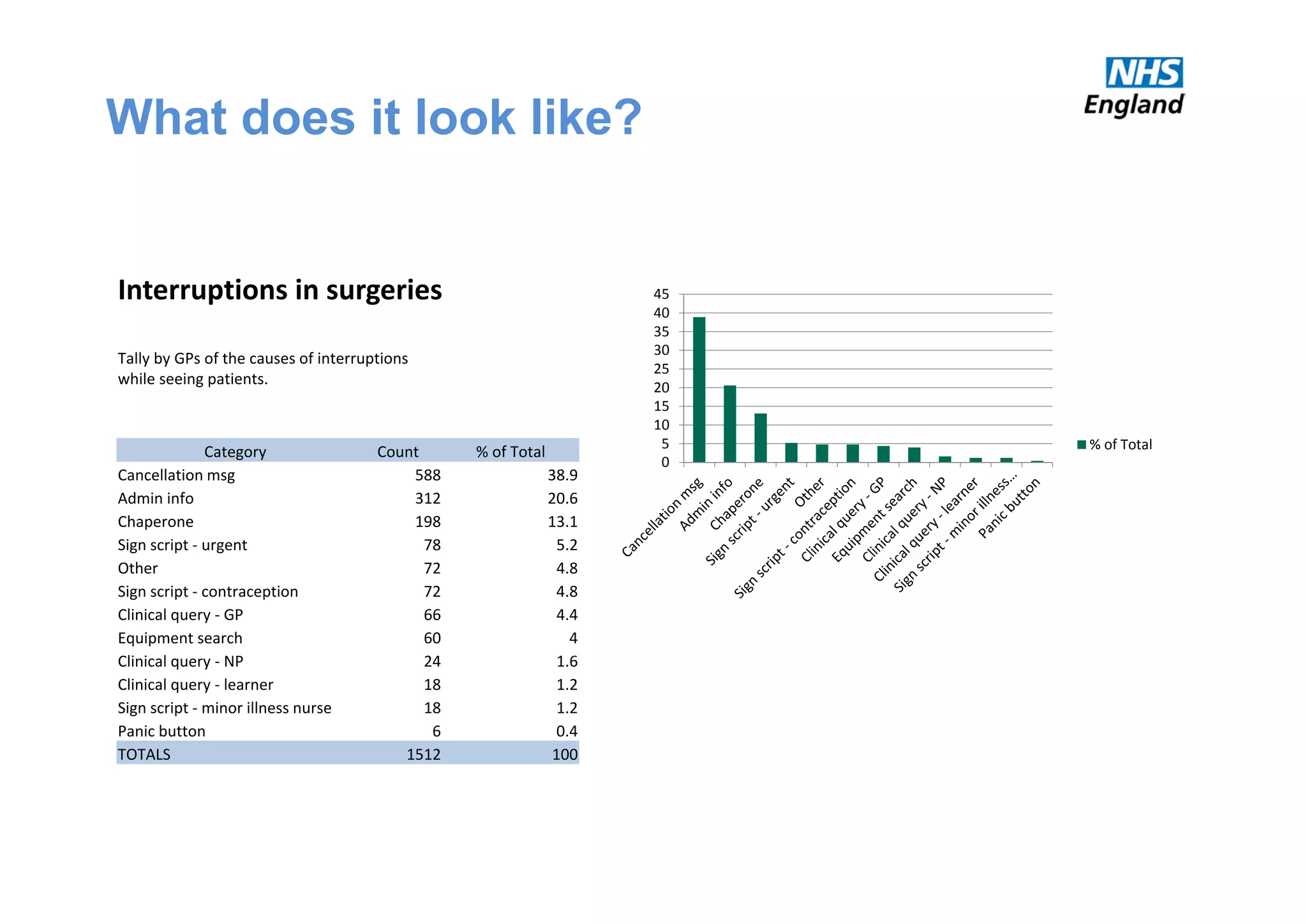
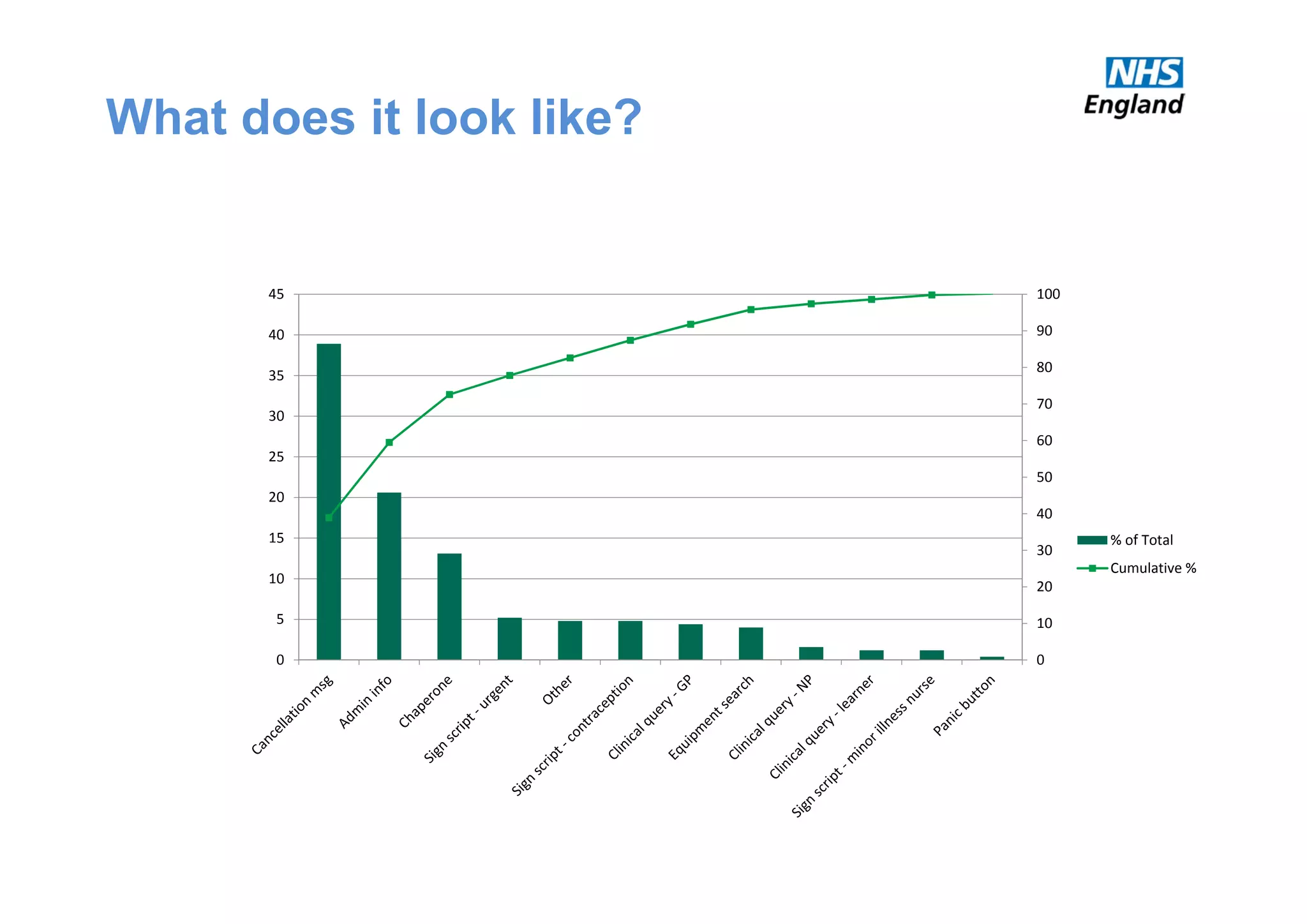
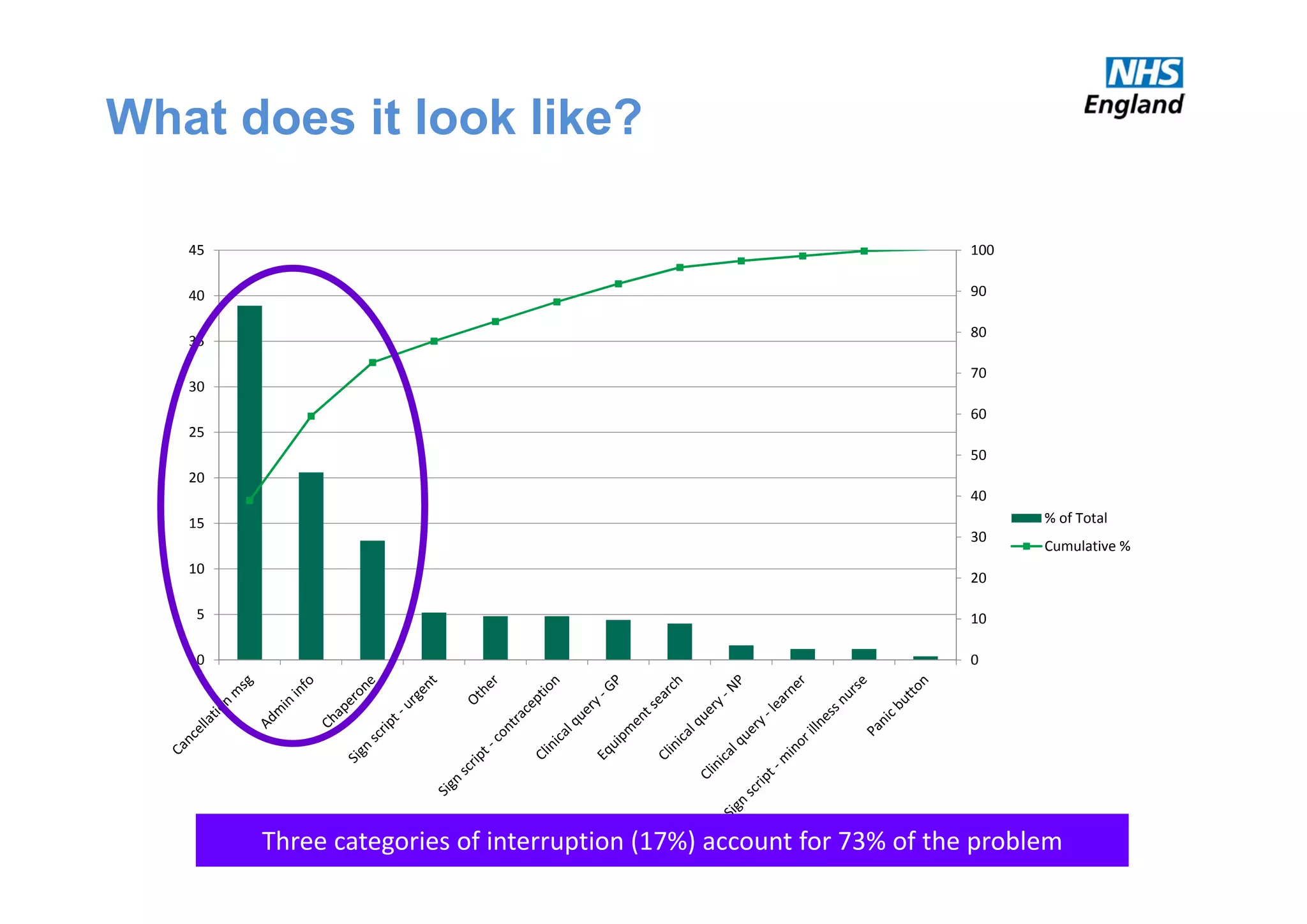
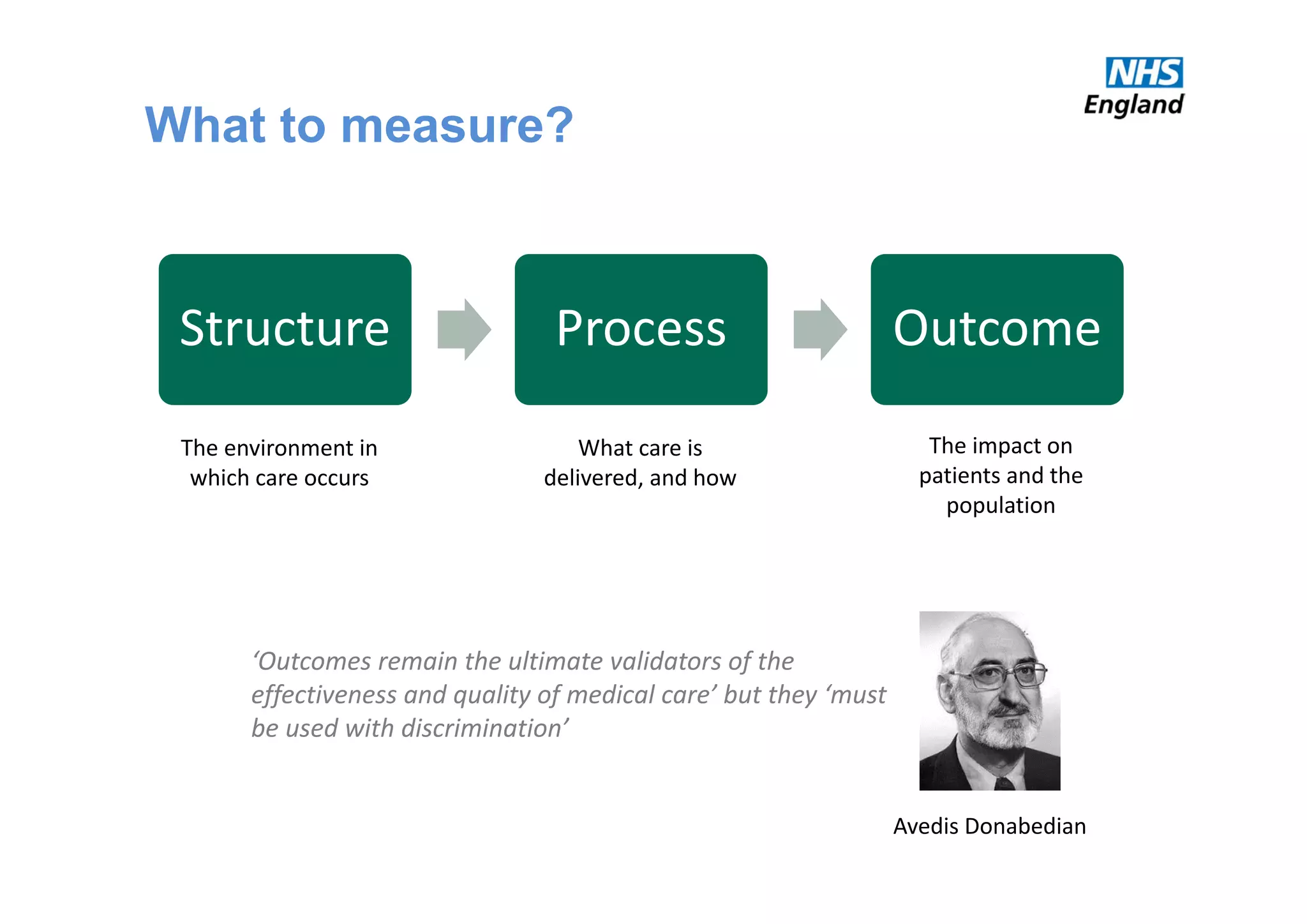
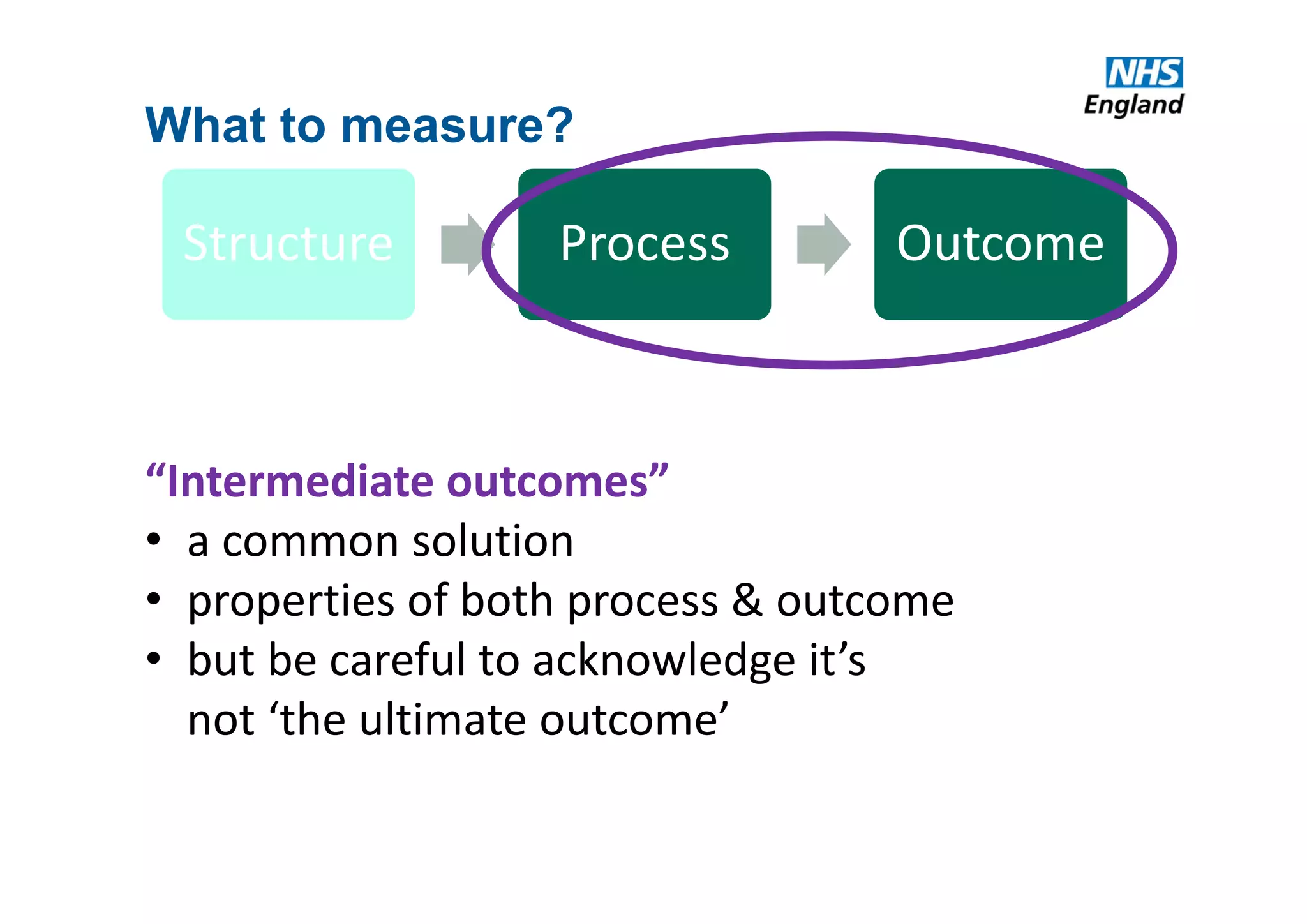
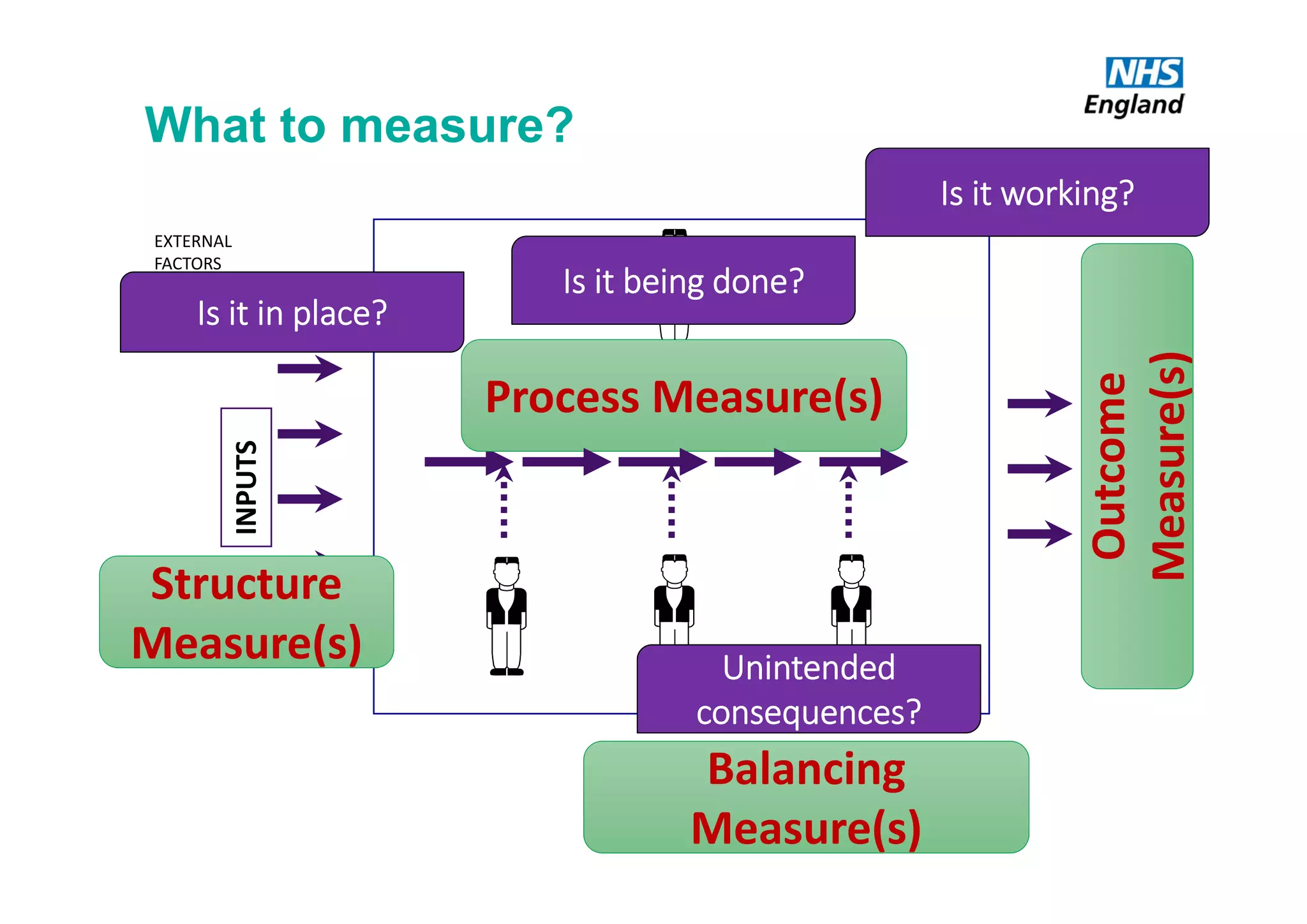
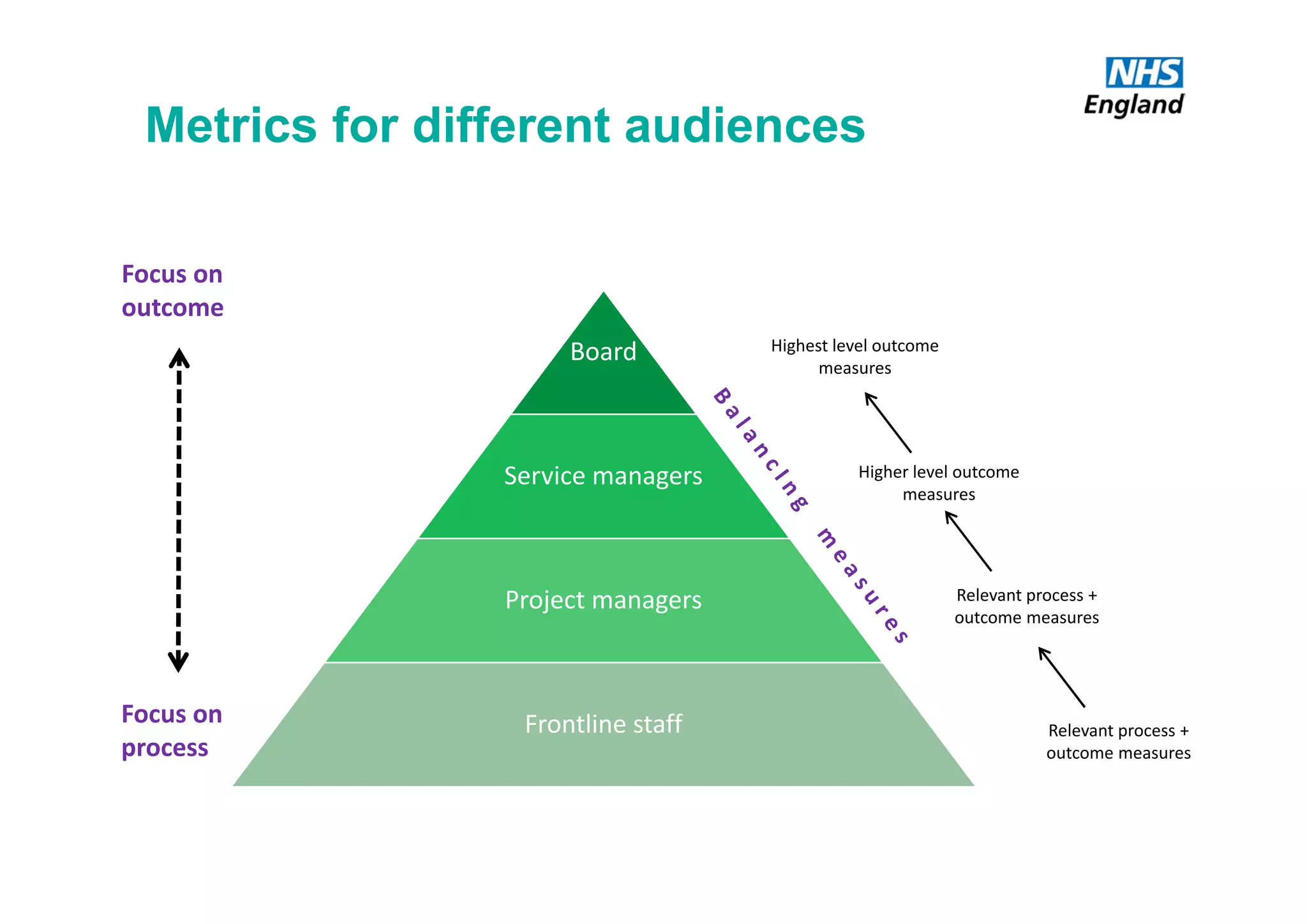
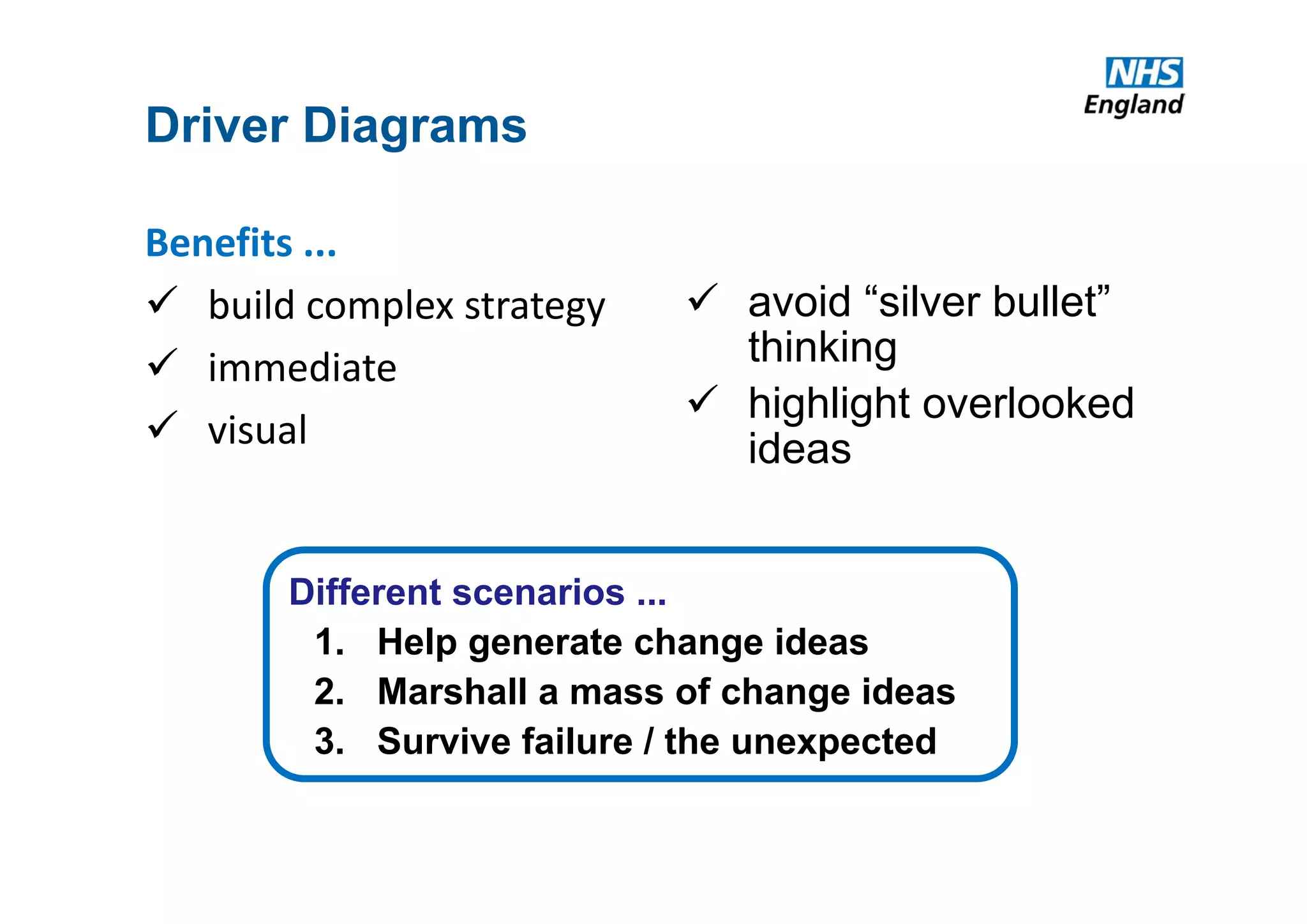
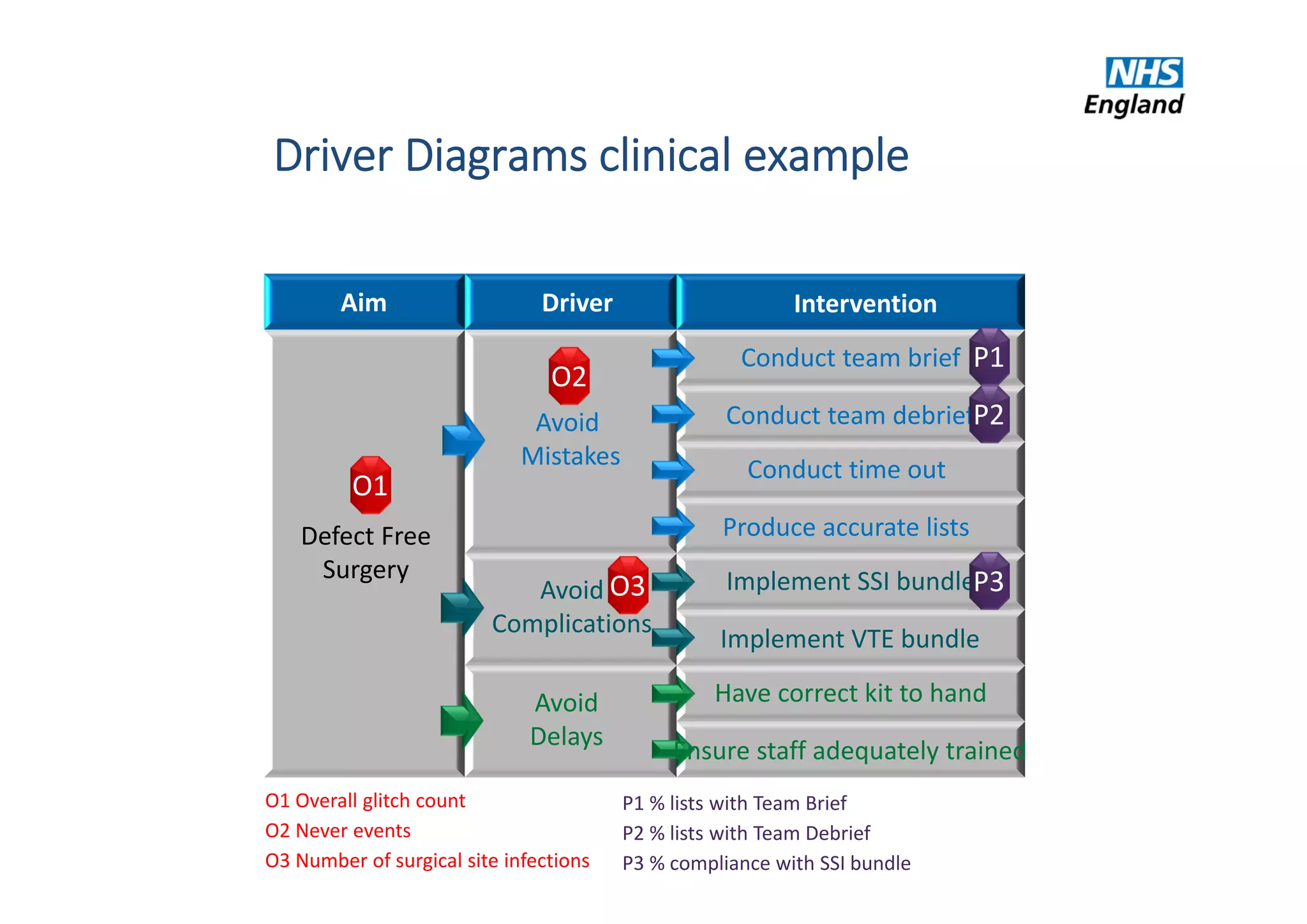
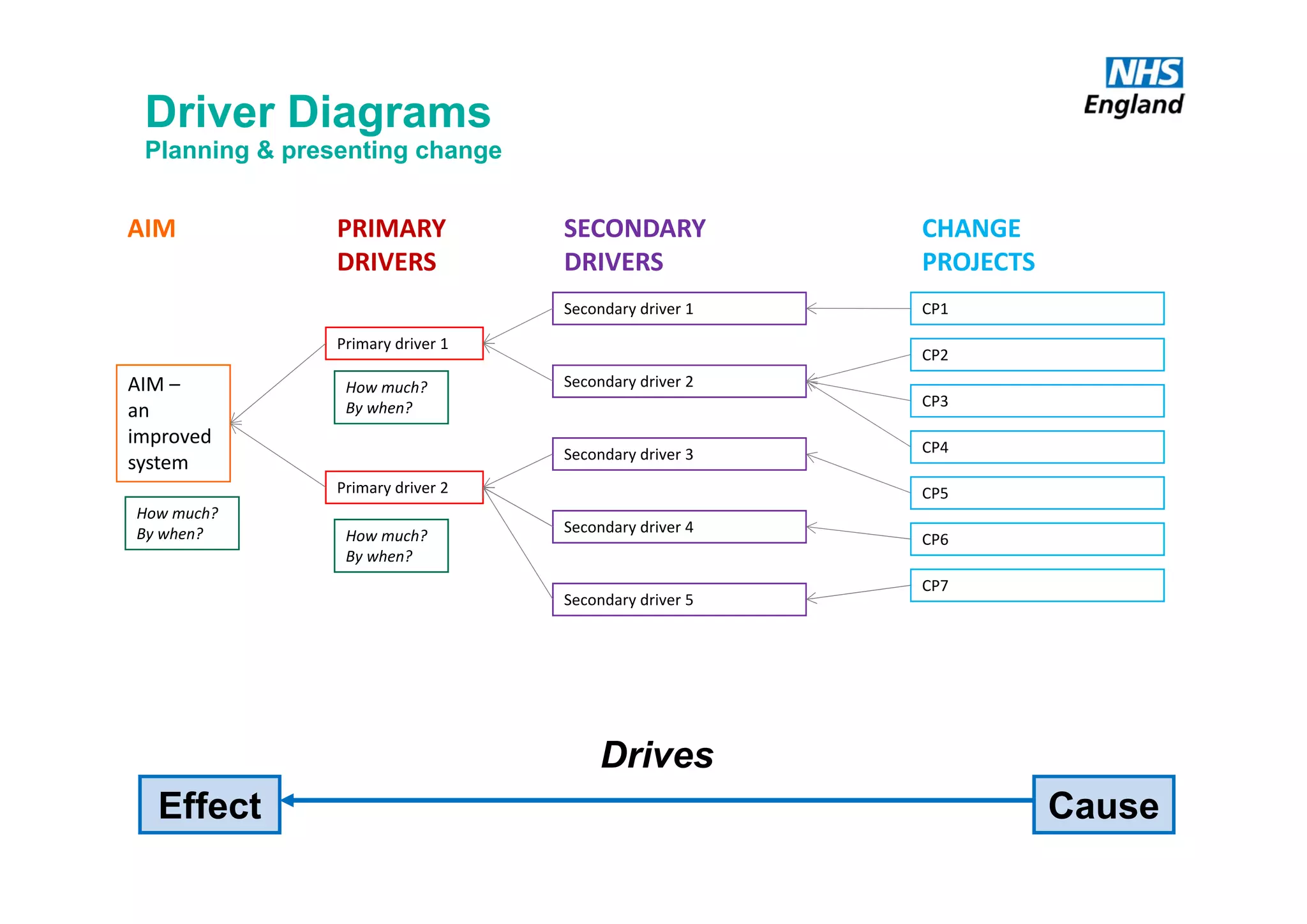
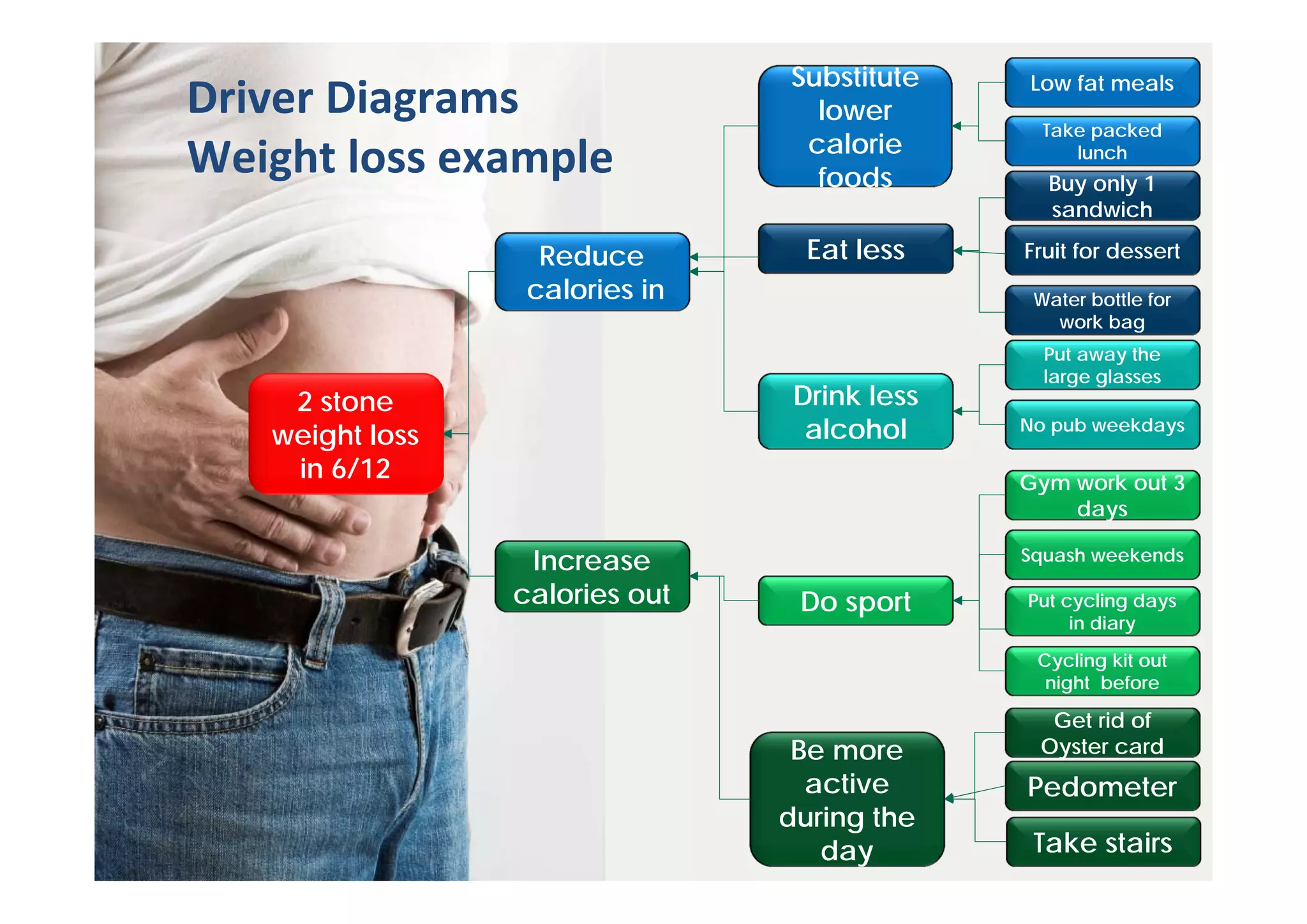
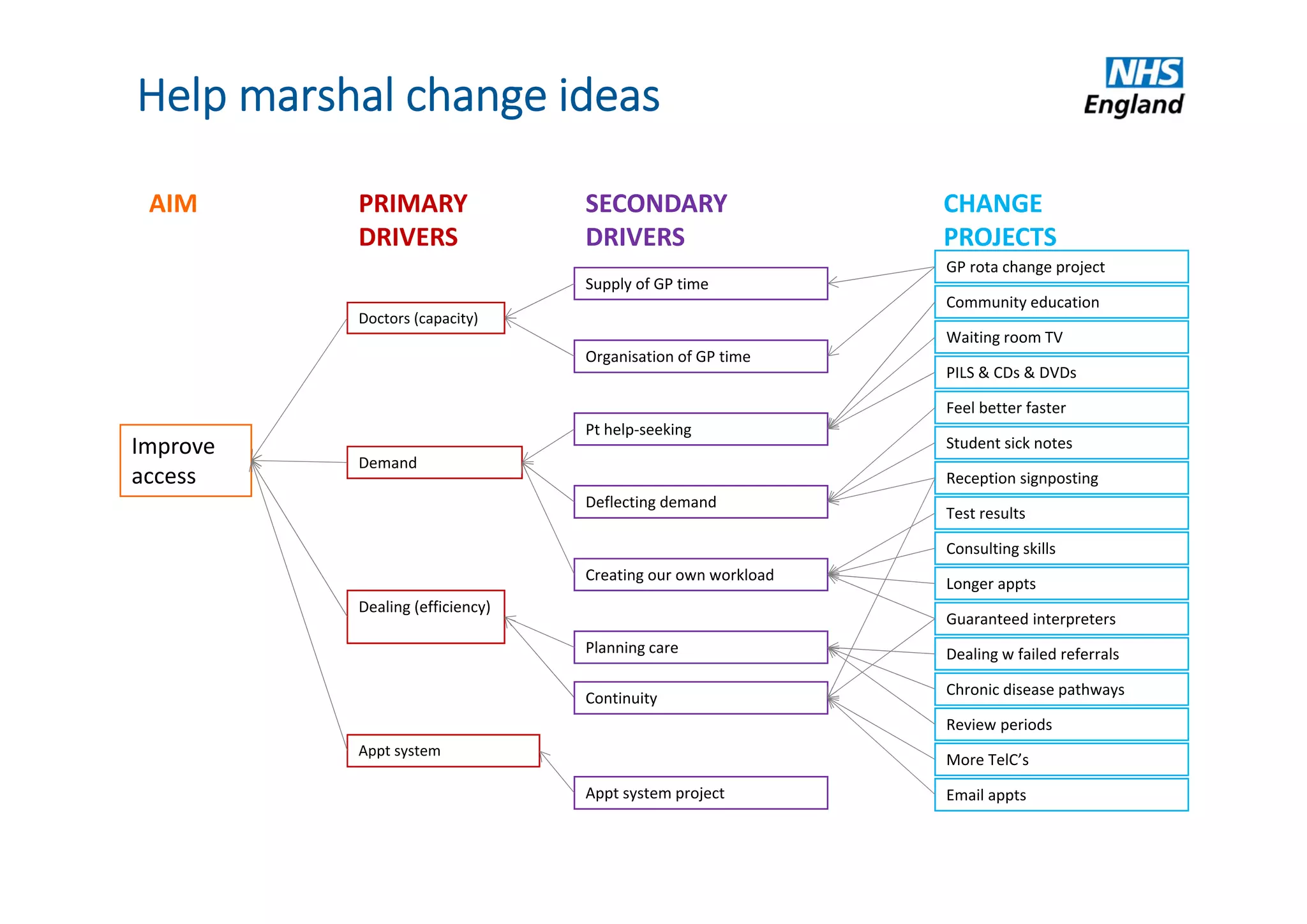
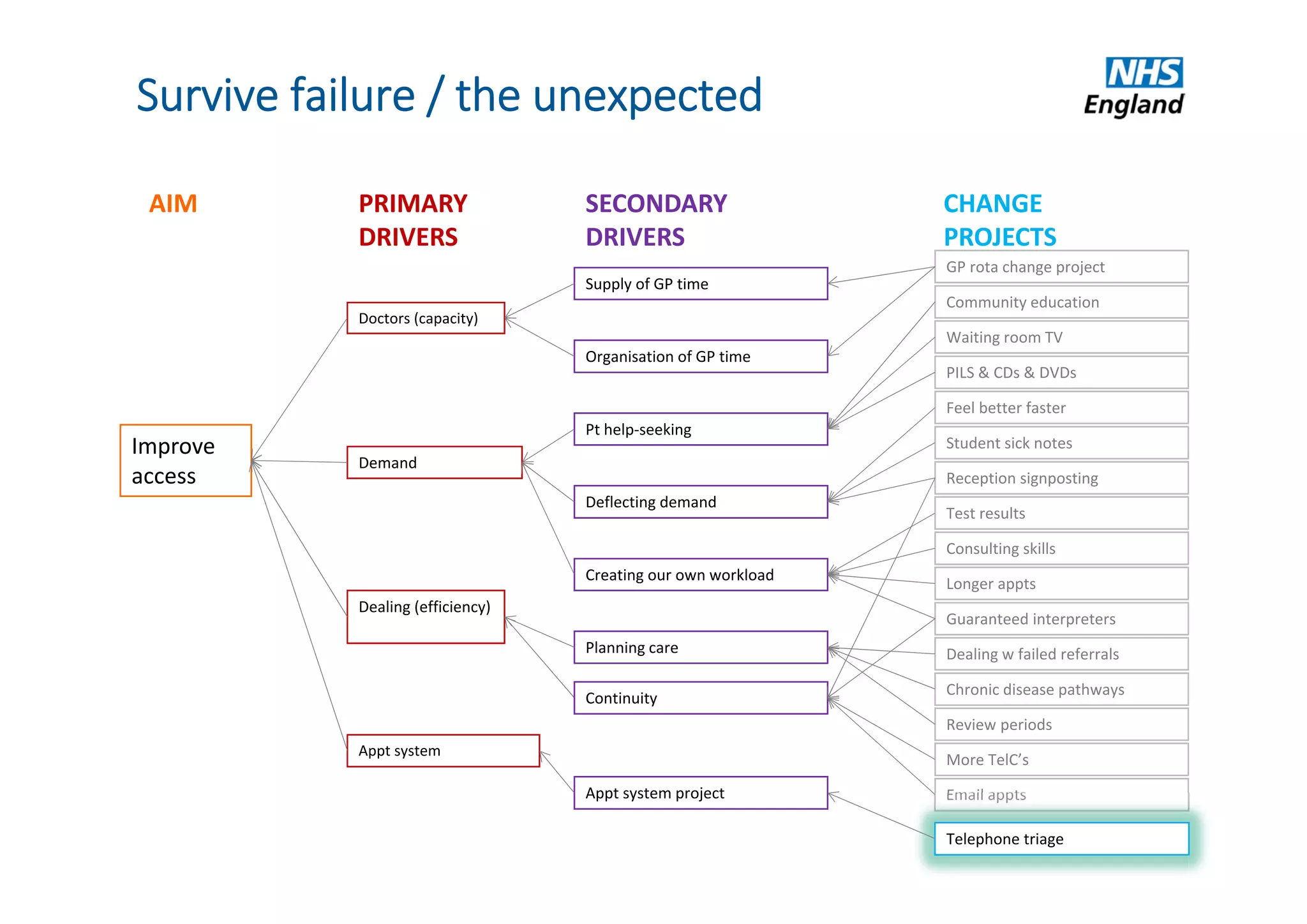
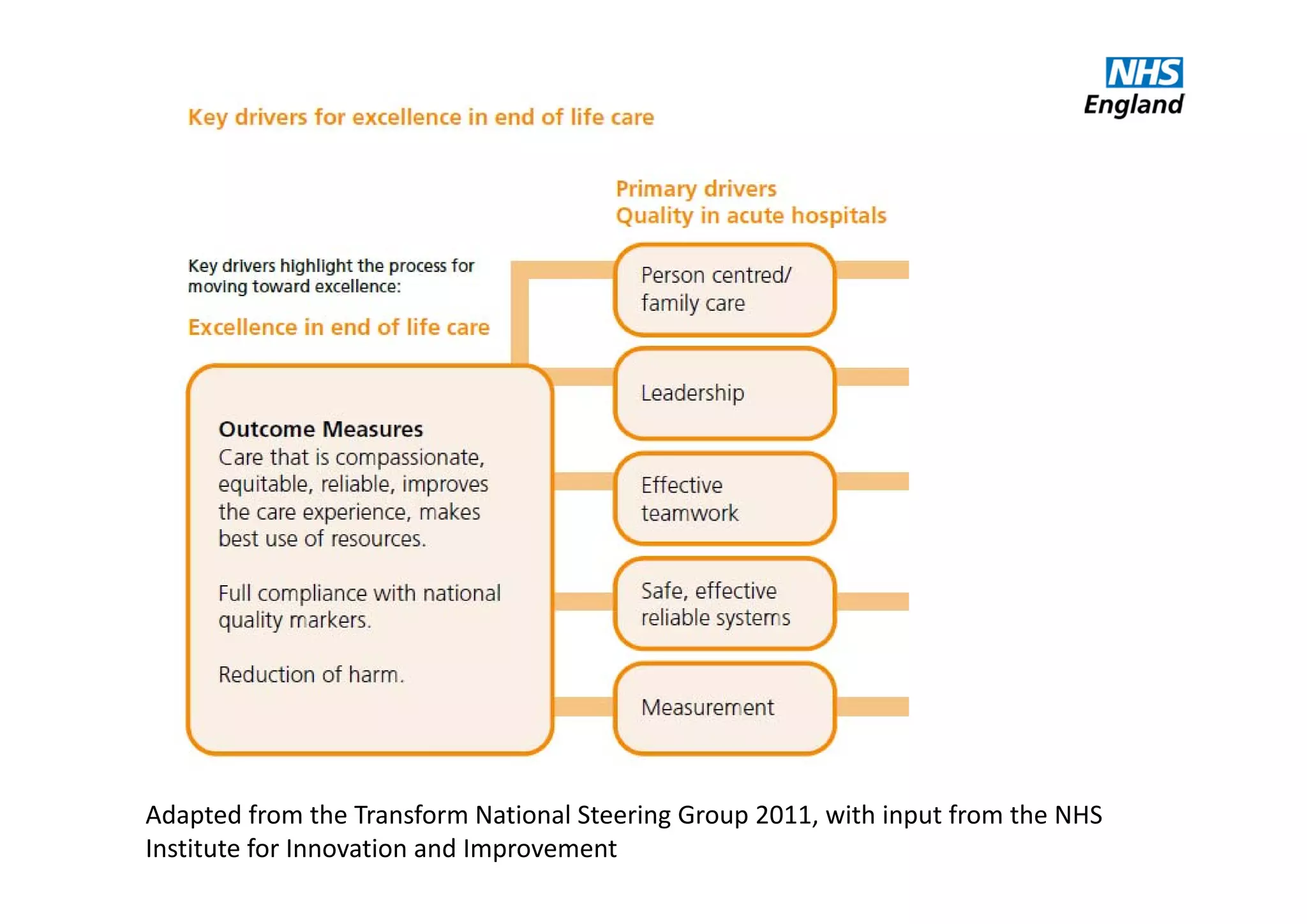
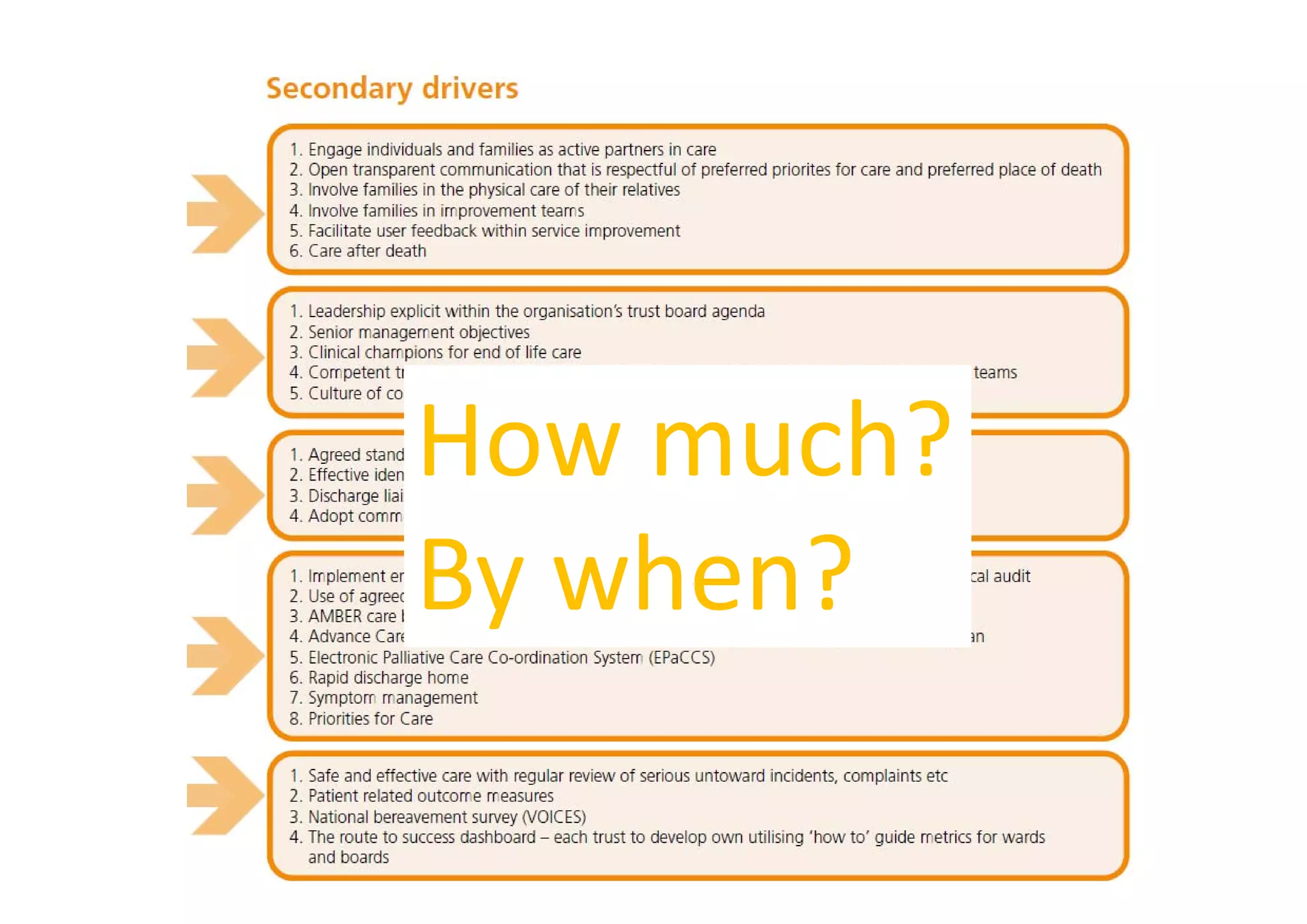
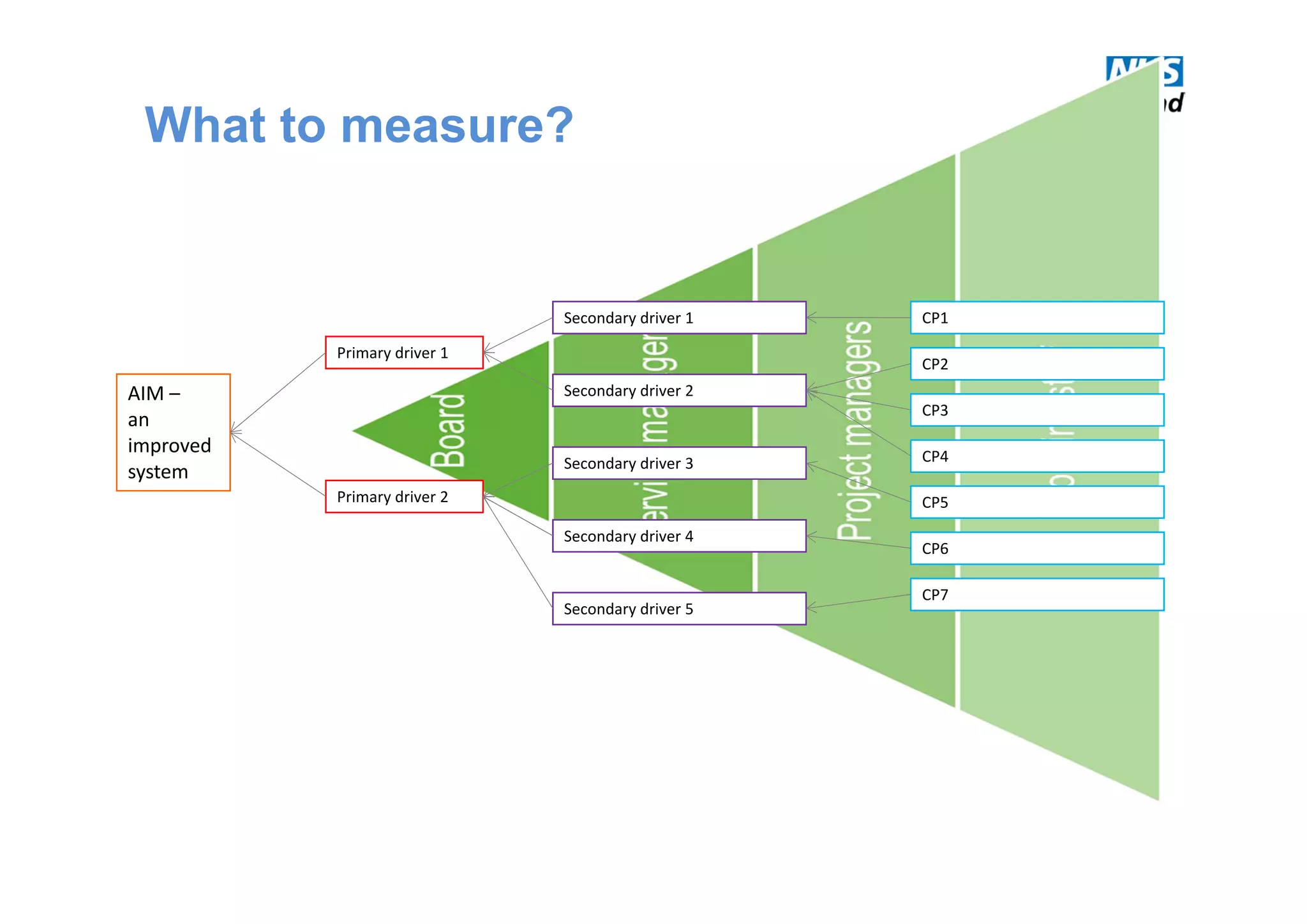
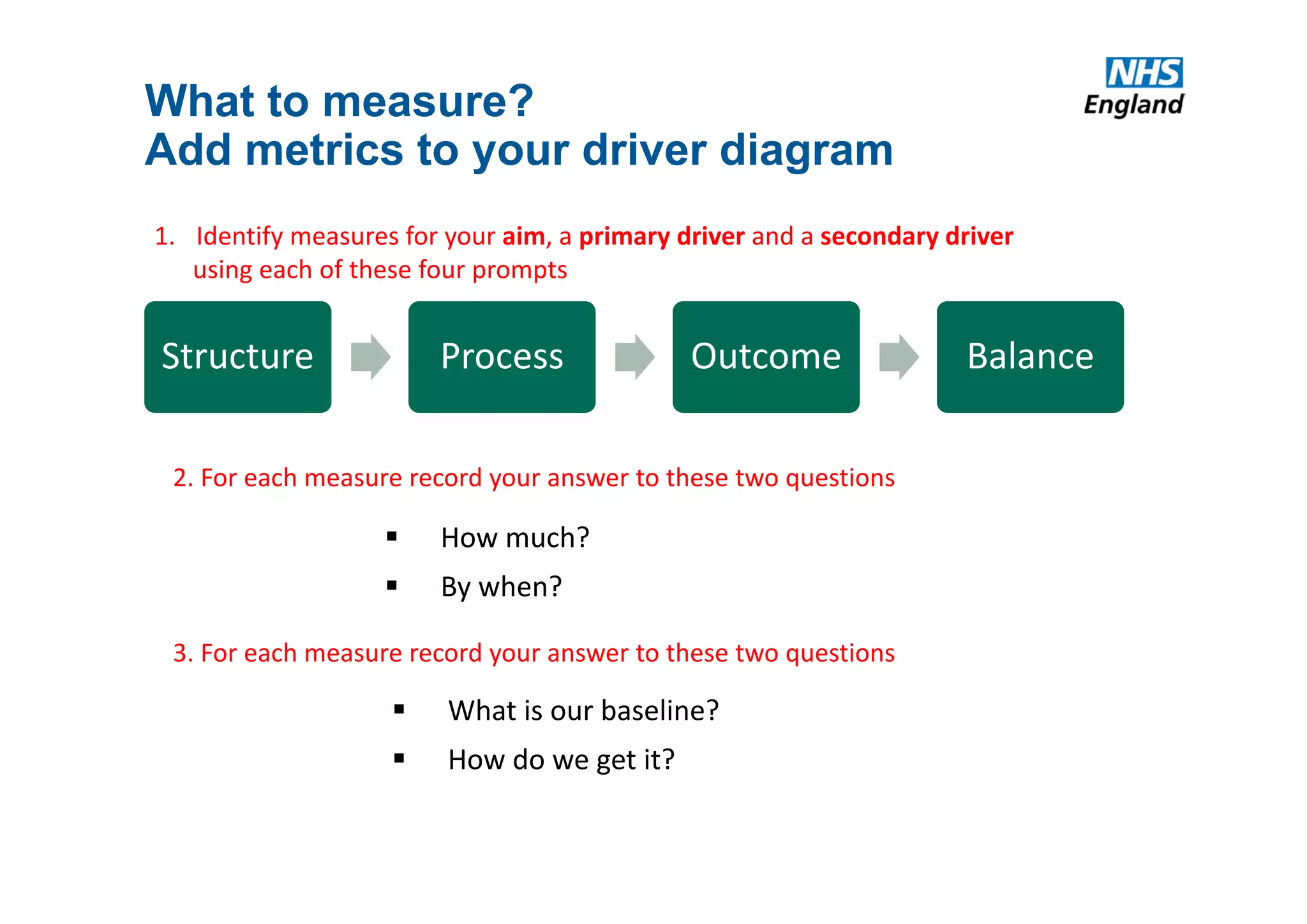
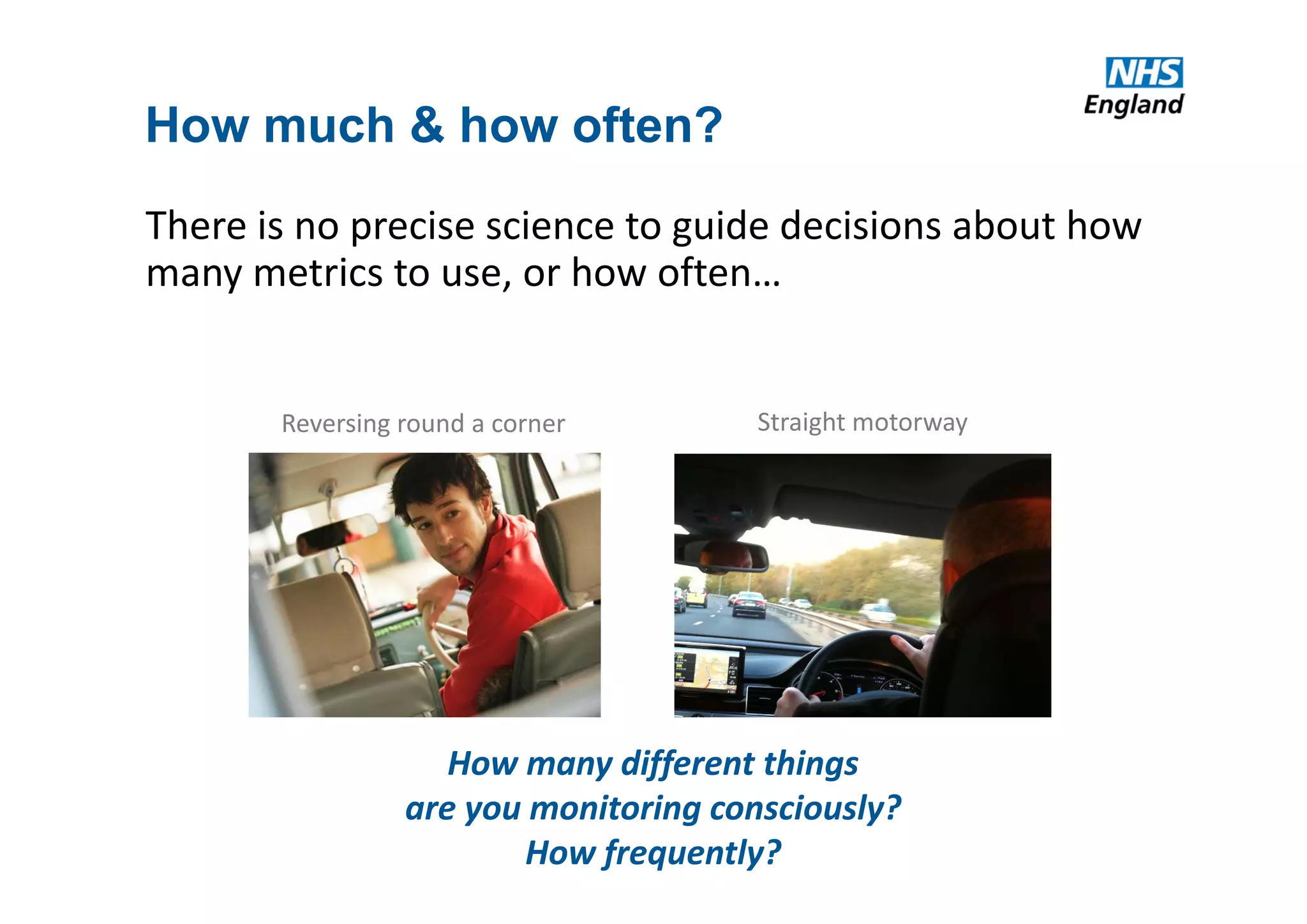
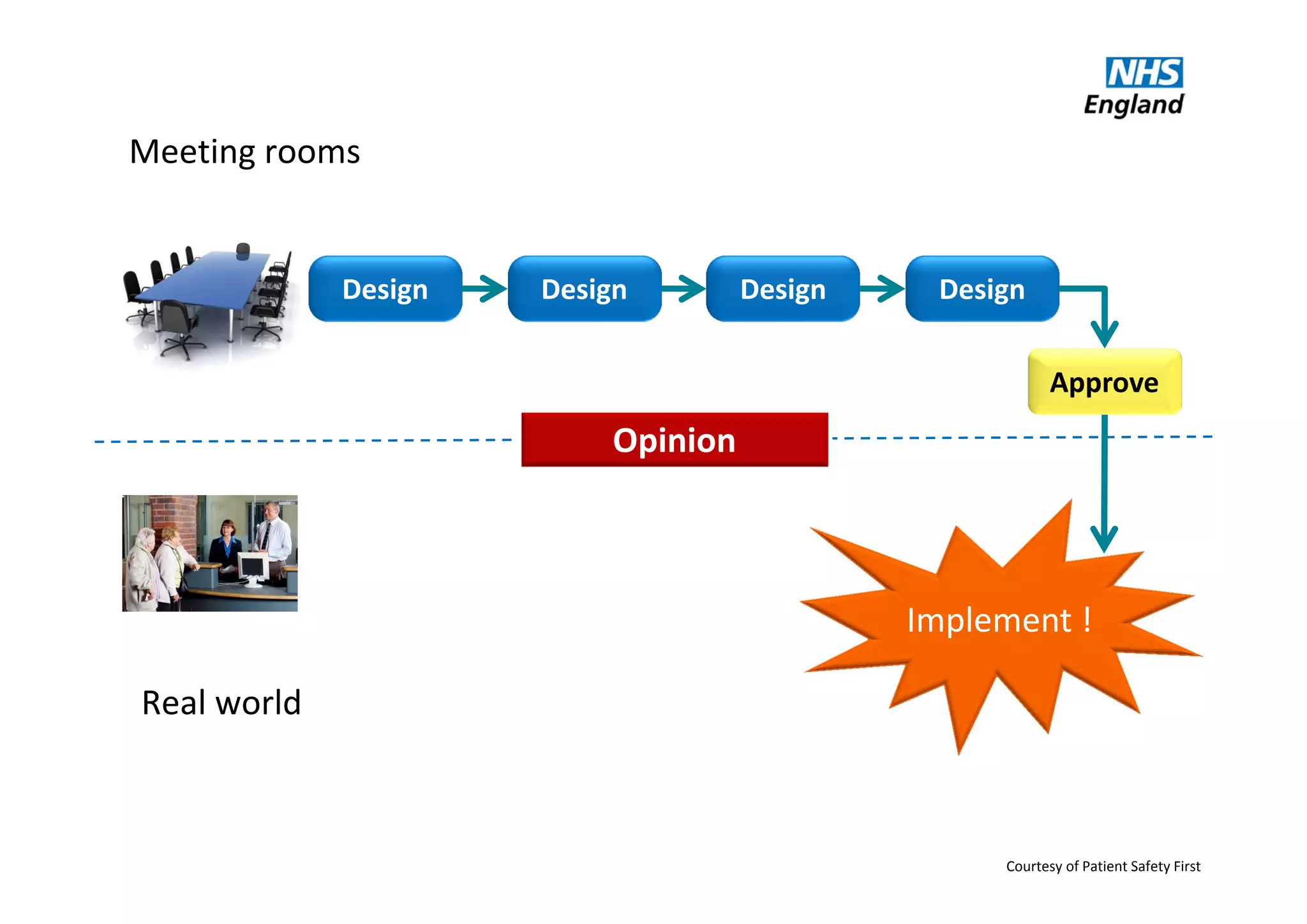
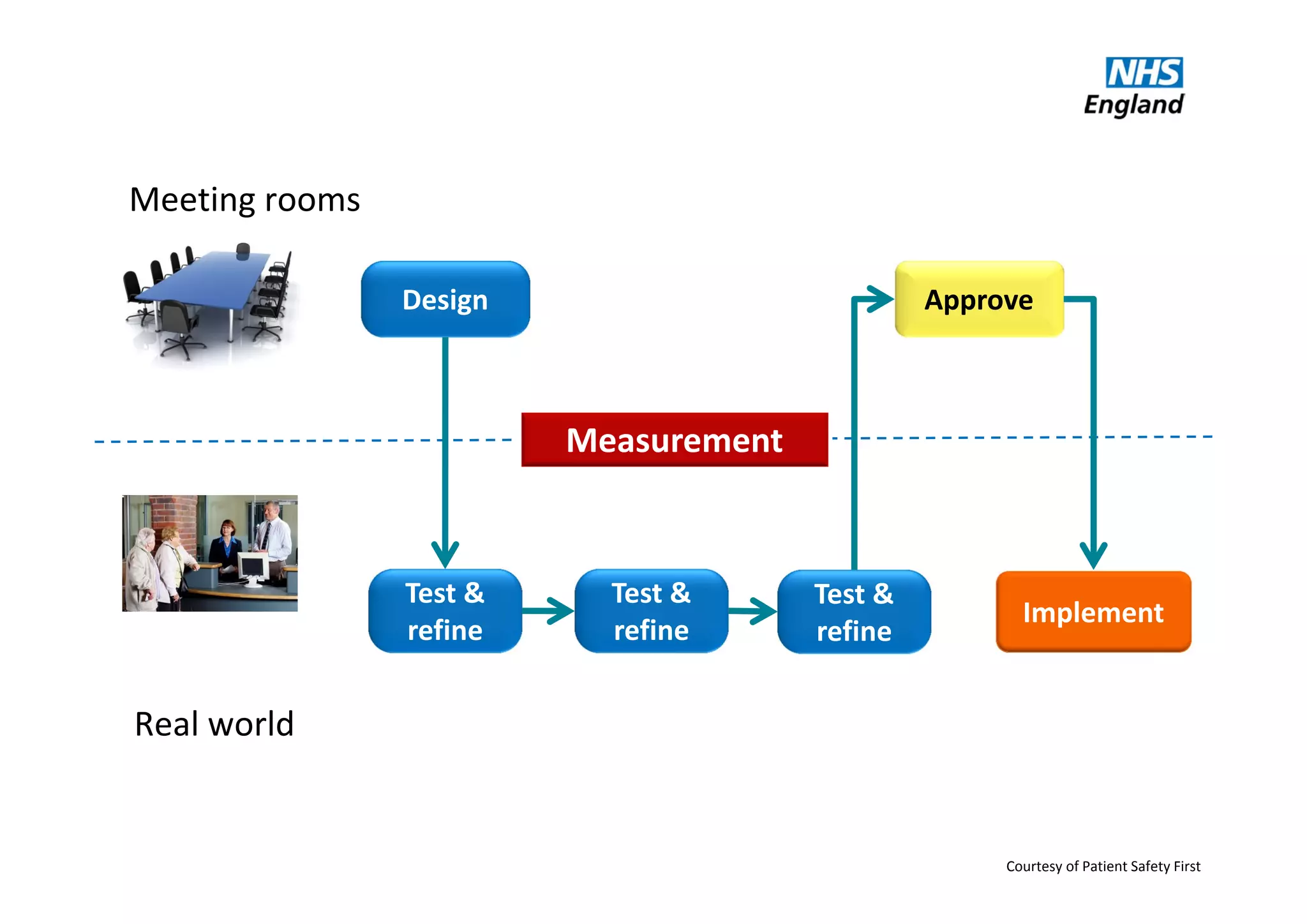
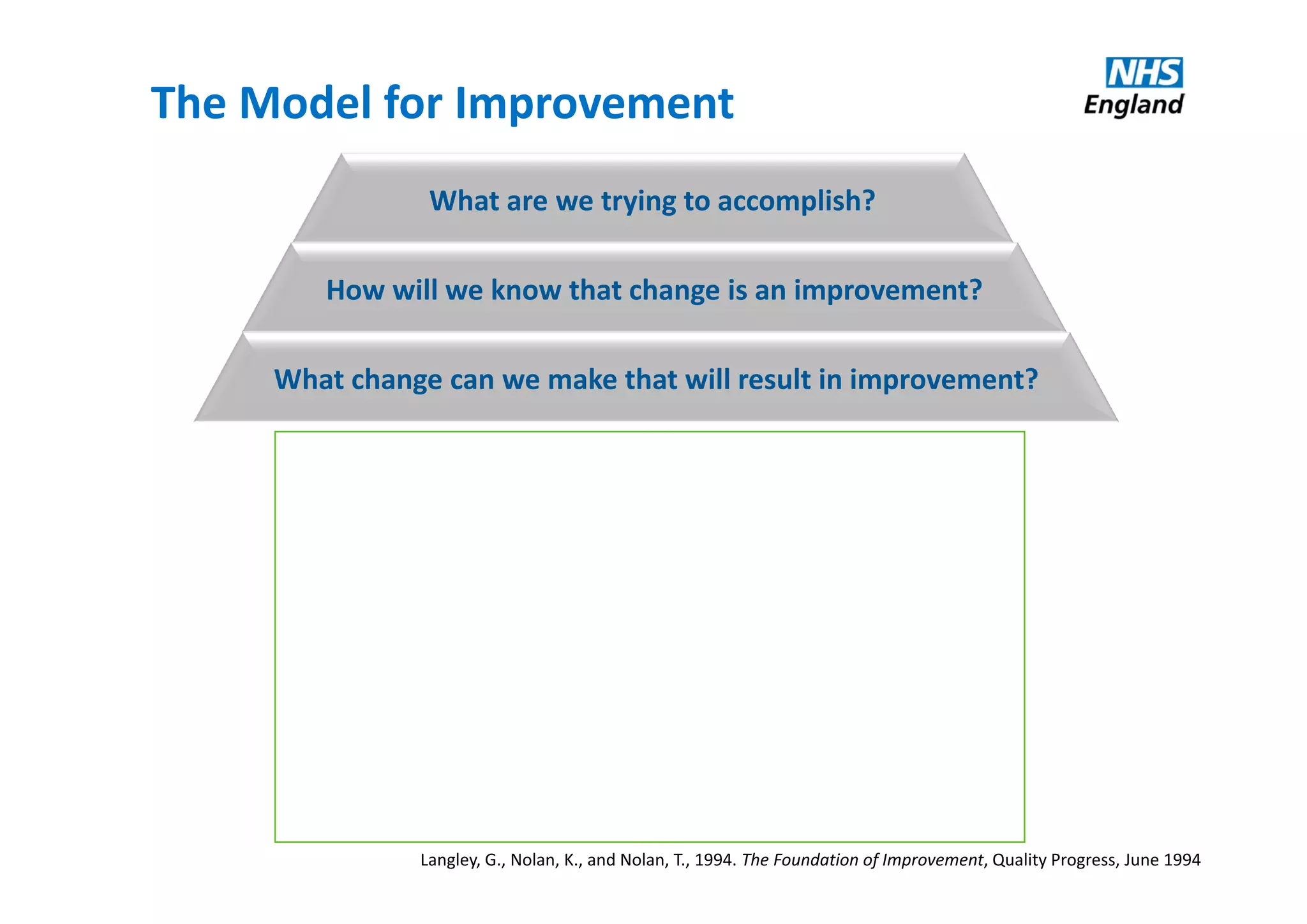
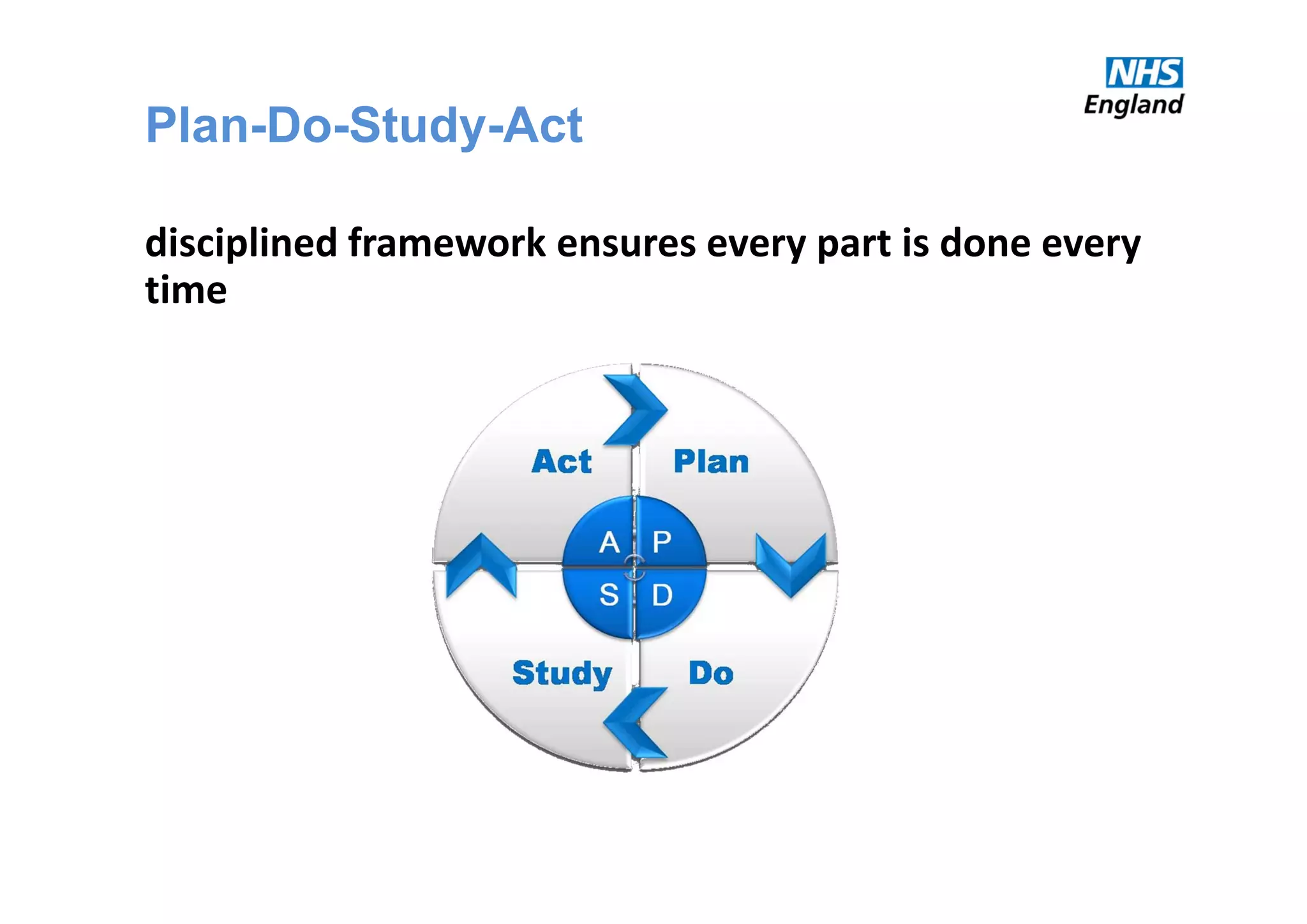
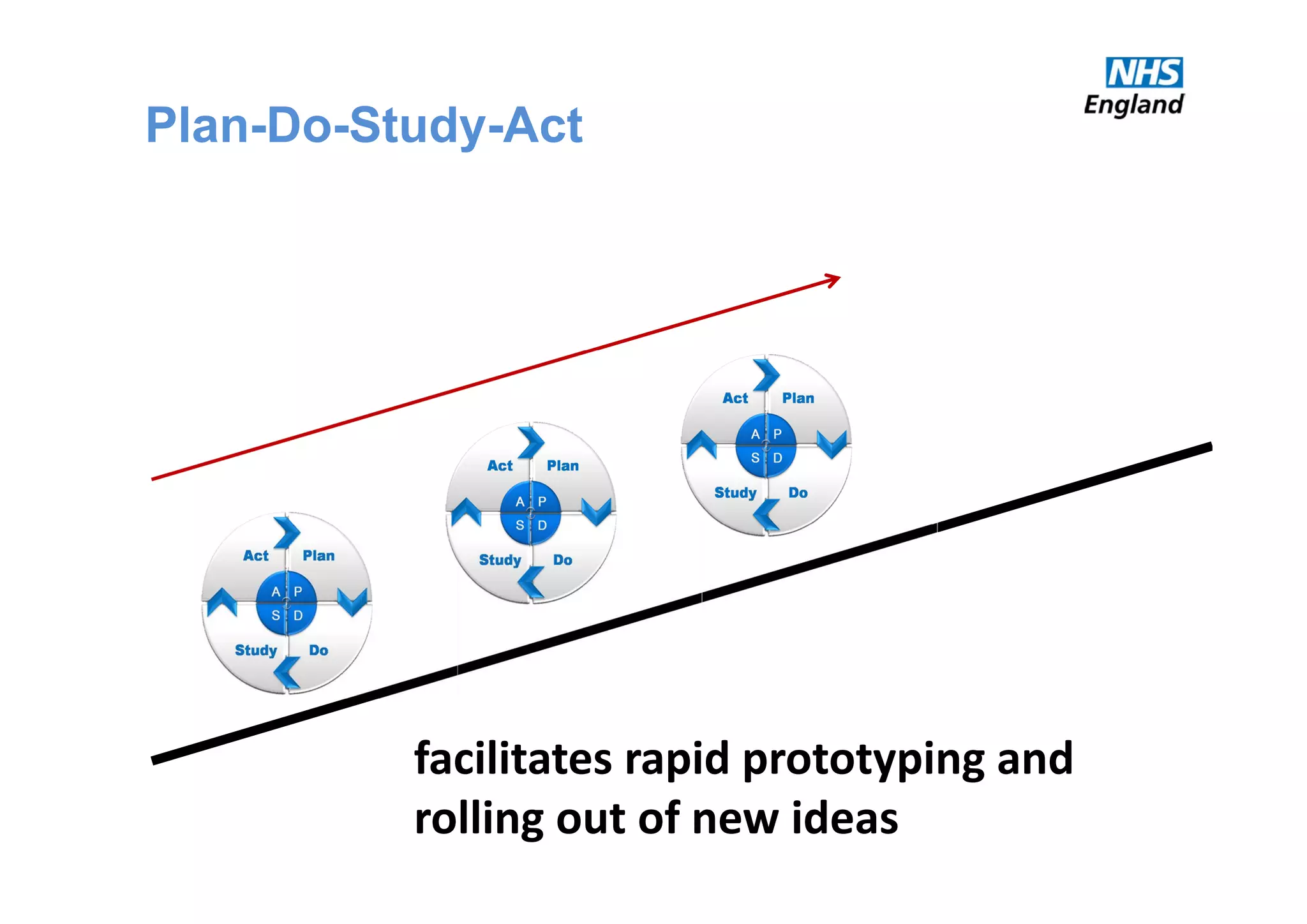
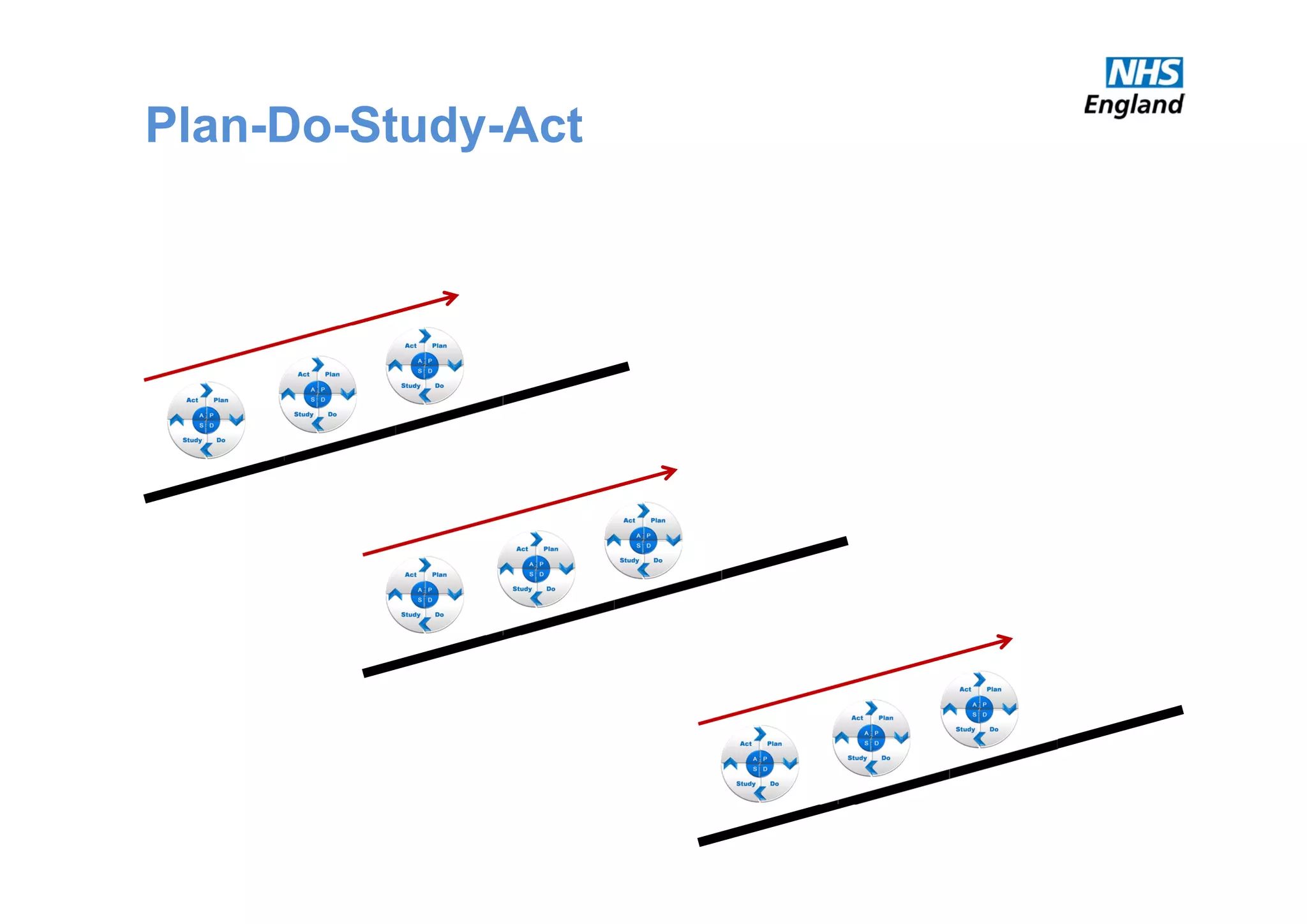
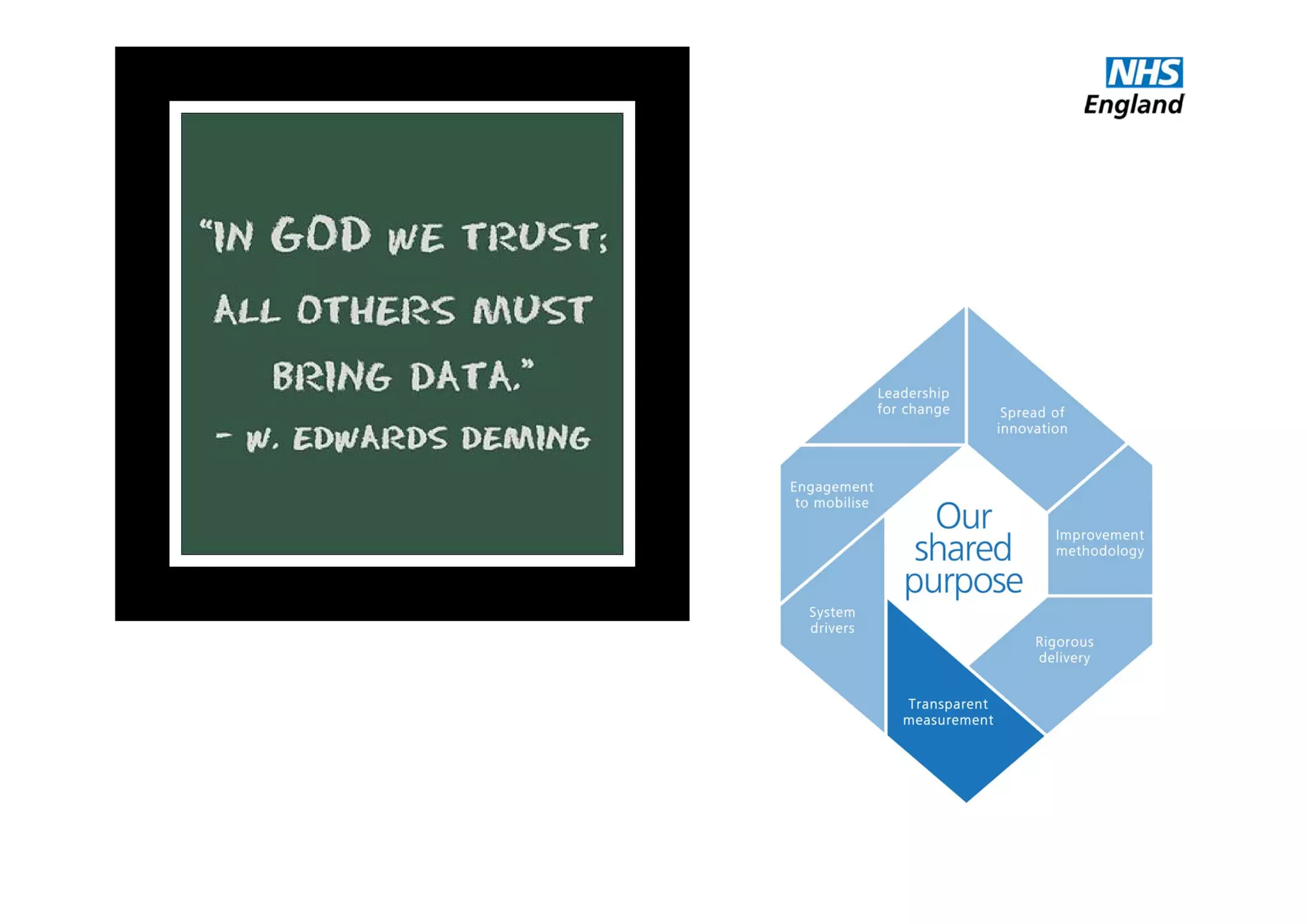
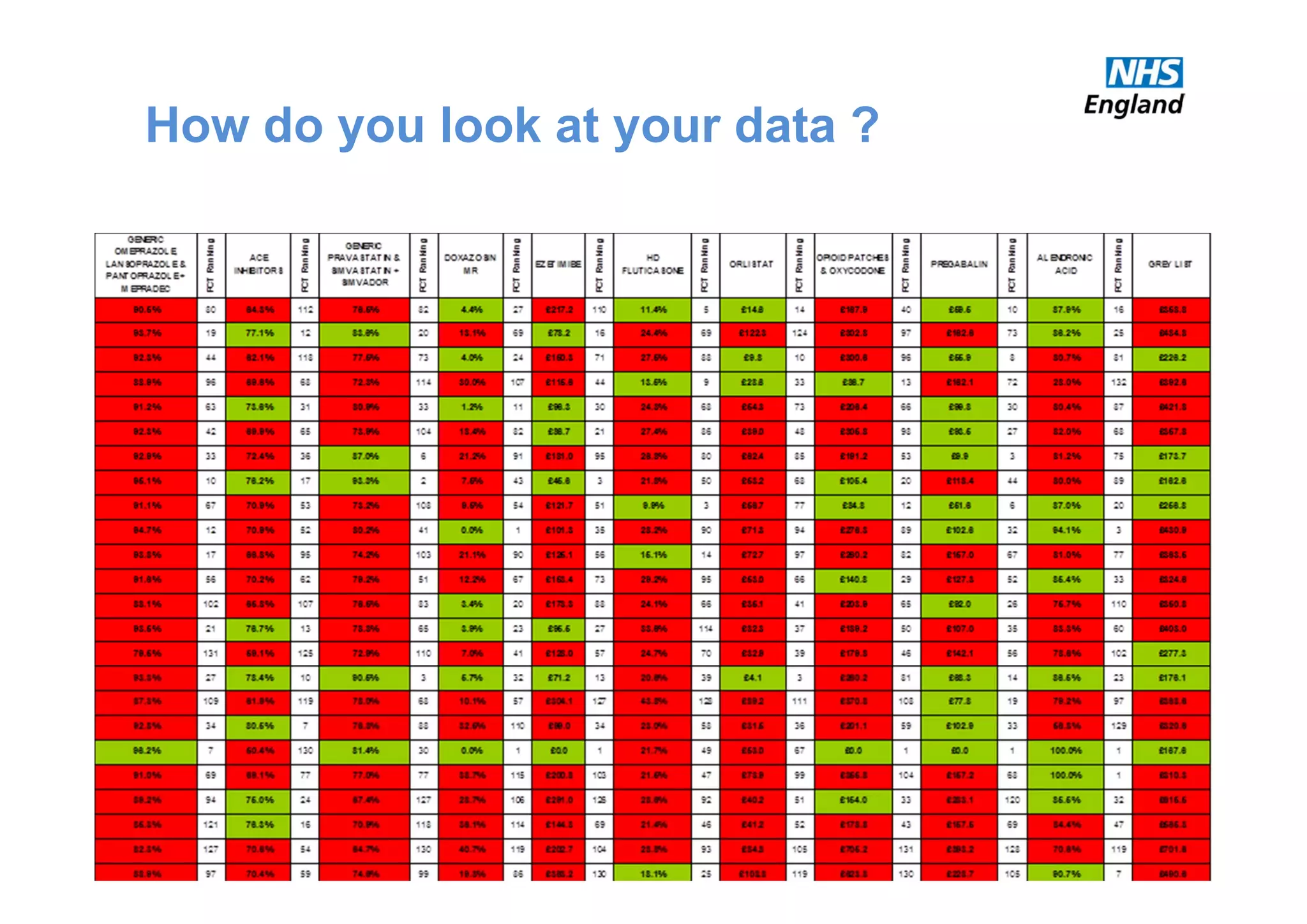
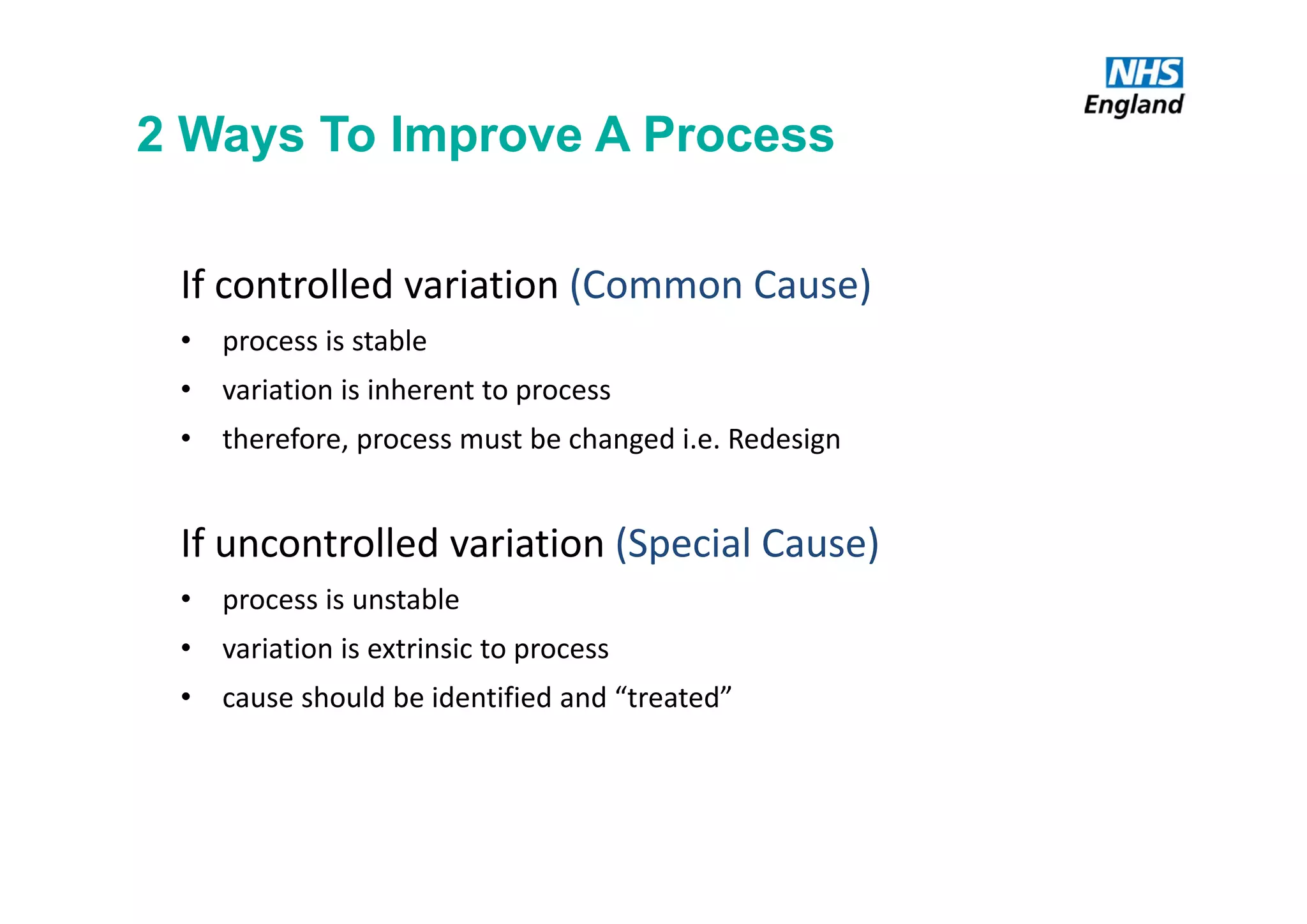
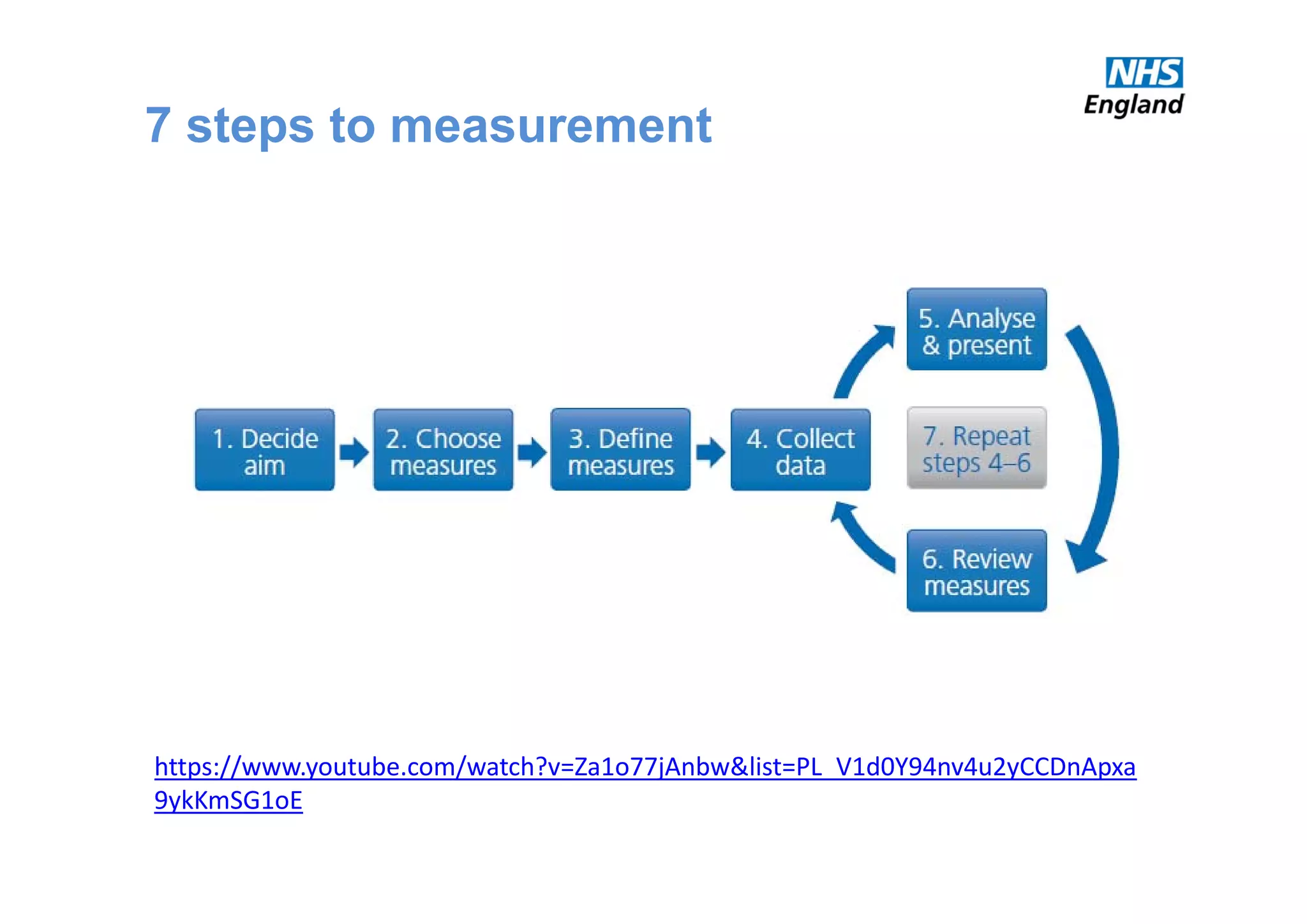
The document discusses the transformation of end-of-life care in acute hospitals through effective measurement and improvement strategies. It highlights the significance of meaningful data collection, the use of various measurement traditions, and focuses on prioritizing critical issues to enhance patient care. Additionally, it outlines a structured approach to measurement, including the use of driver diagrams and the model for improvement to facilitate change in healthcare settings.