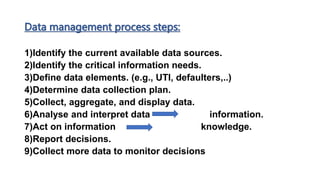
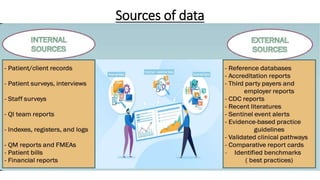
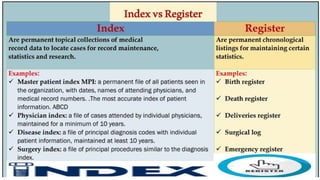
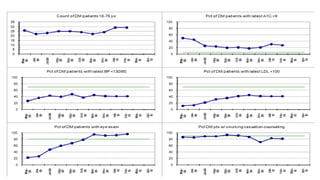
This document discusses information management and using data to measure performance improvement. It defines data and information, explaining that data must be analyzed and interpreted to become useful information. The goal of information management is to support decision making to improve patient outcomes, safety, documentation, and performance. It outlines the steps of data management, including collecting, tracking, analyzing, and acting on data. Performance measures are discussed, including different types like process, outcome, and balancing measures. Choosing good performance measures and tracking data over time to monitor improvement is also covered.