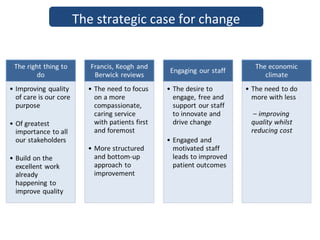
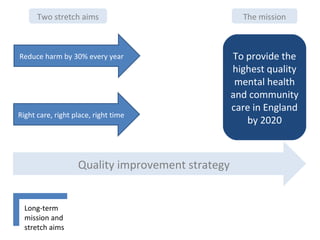
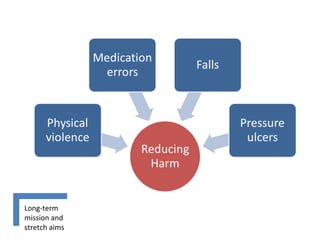
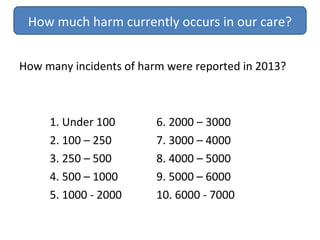
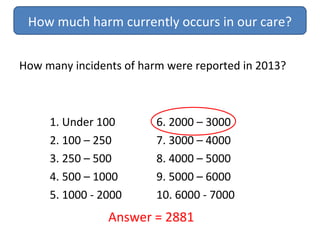
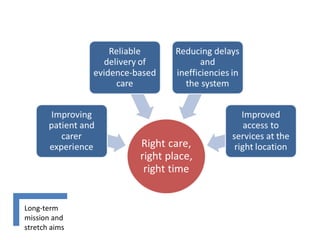
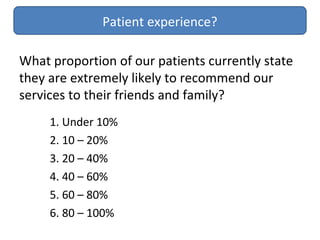
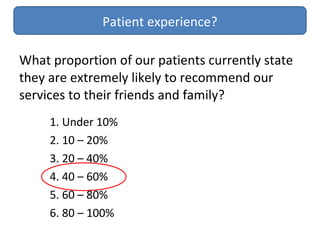
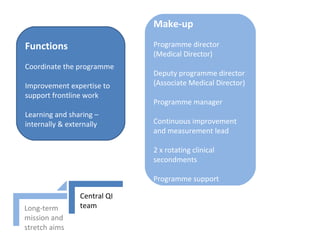
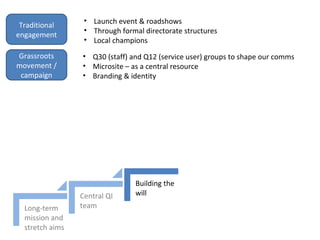
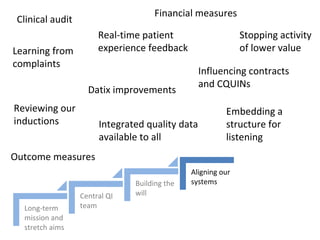
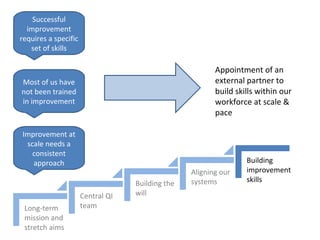
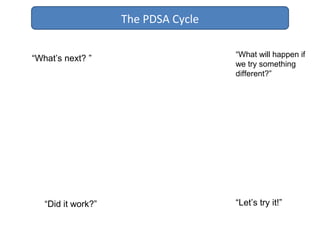
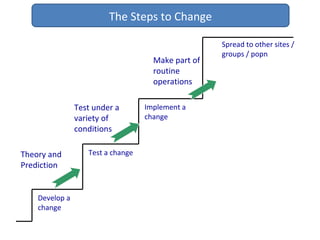
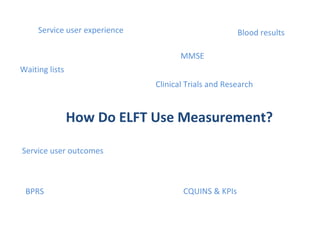
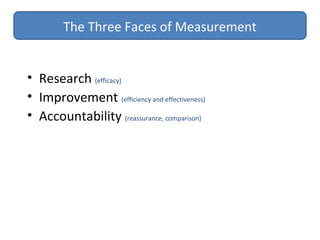
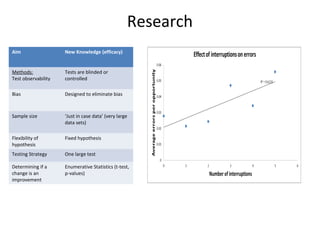
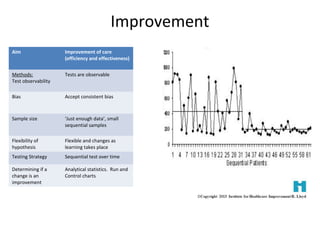
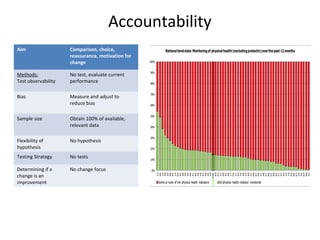
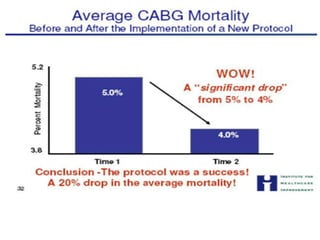
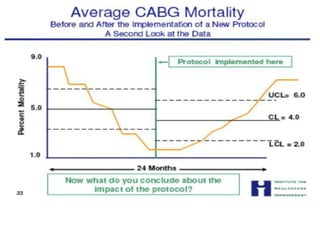
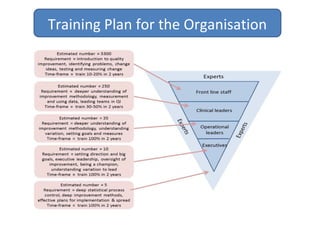
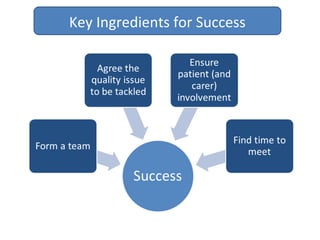
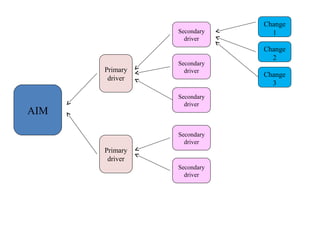
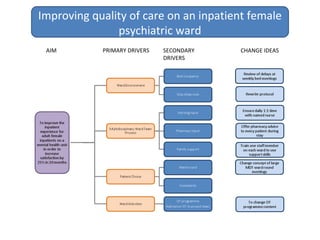
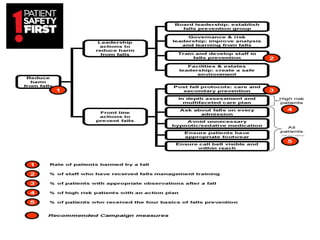
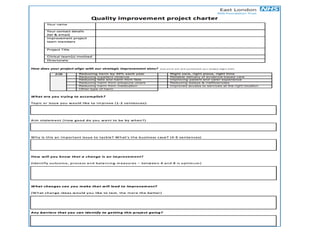
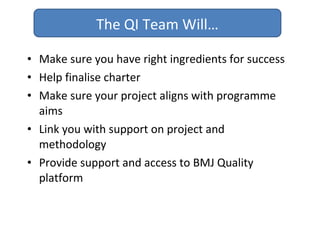
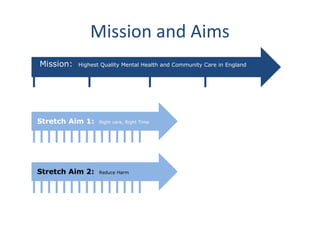
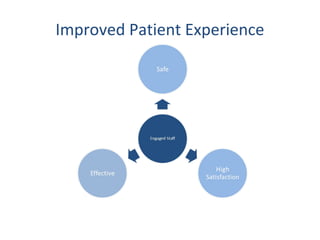
The document outlines a quality improvement program for a mental health and community care organization. It discusses establishing a long-term mission to provide the highest quality care in England and sets stretch aims to reduce harm and ensure right care at the right time. It describes forming a central QI team to coordinate the program and build improvement skills through training and an external partner. The program will use measurement and data to track progress, and will involve staff, patients, and carers through local champions and feedback groups. Projects will follow the Model for Improvement using PDSA cycles to test changes aimed at meeting the program's mission and aims.