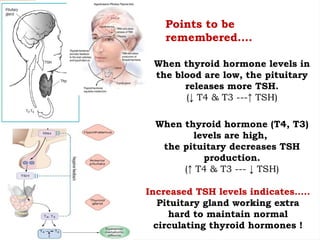
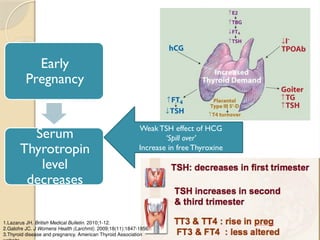
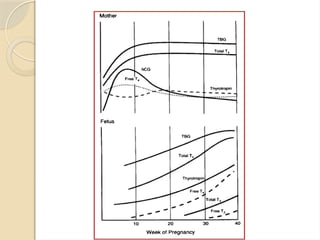
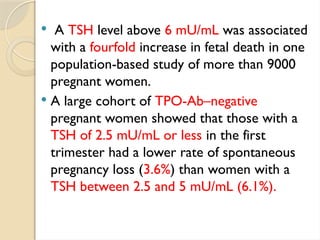
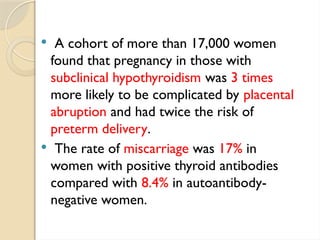
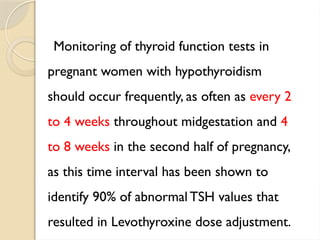
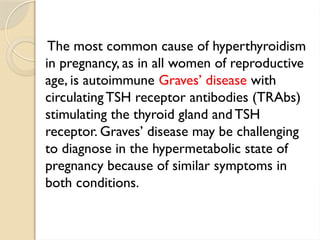
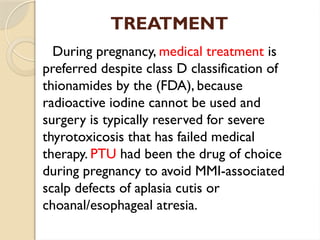
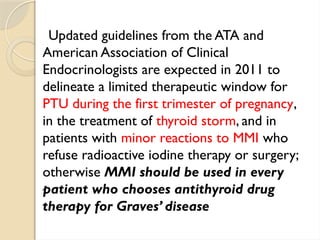
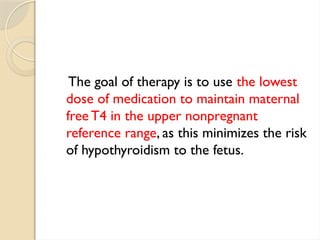
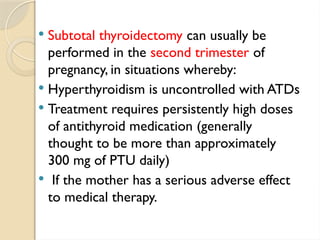
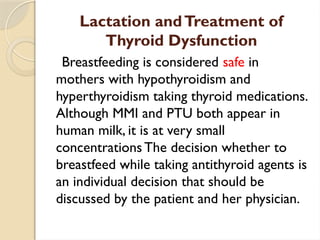
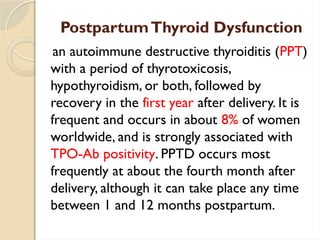
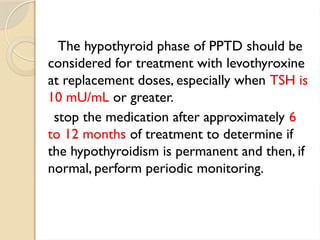
The document discusses thyroid disorders during pregnancy, emphasizing the importance of thyroid hormones in fetal development and the risks associated with maternal hypothyroidism, which can lead to severe developmental delays in children. It outlines the prevalence of thyroid conditions in pregnant women and recommendations for monitoring and treatment, including the adjustment of levothyroxine dosages as needed. The document also highlights postpartum thyroid dysfunction and the need for screening for thyroid issues in women with certain risk factors following childbirth.