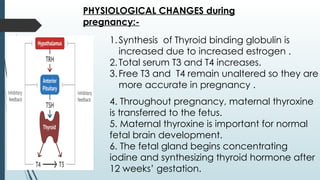
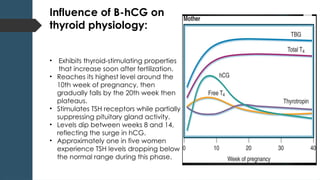
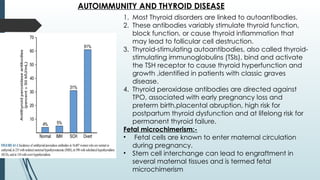
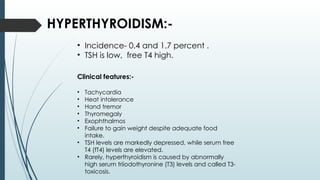
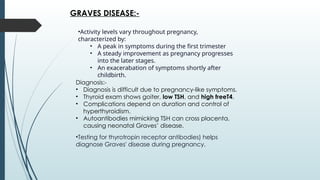
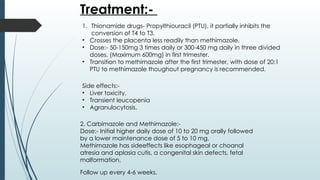
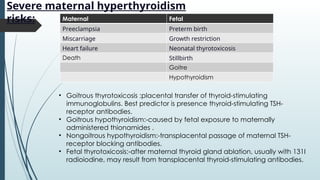
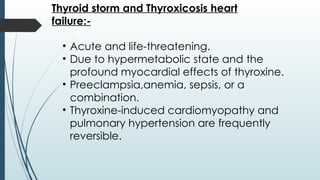
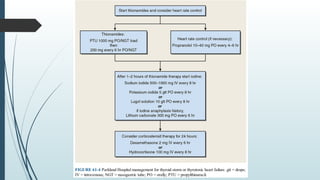
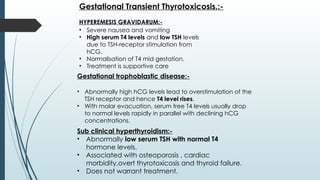
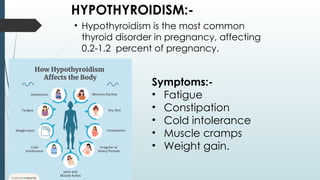
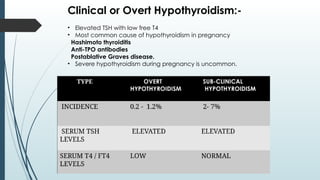
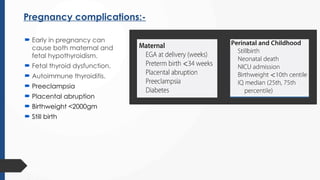
This presentation provides a comprehensive overview of thyroid disorders in pregnancy, covering hypothyroidism, hyperthyroidism, subclinical thyroid dysfunction, and their maternal-fetal outcomes. It highlights the pathophysiology, diagnosis, clinical features, complications, and management guidelines based on standard references. Special emphasis is given to screening, treatment protocols, and the impact of thyroid hormones on pregnancy and fetal development. This resource is ideal for medical students, residents, gynecologists, endocrinologists, and healthcare professionals preparing for exams, lectures, or clinical practice.