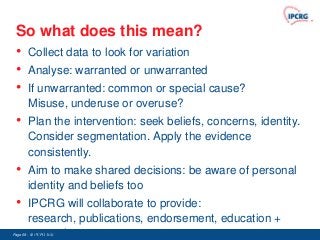
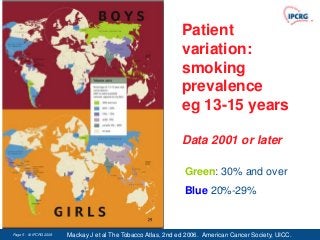
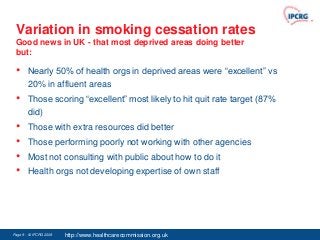
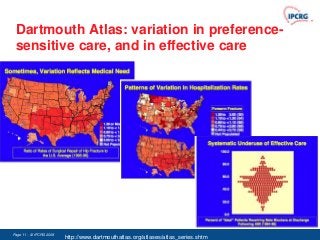
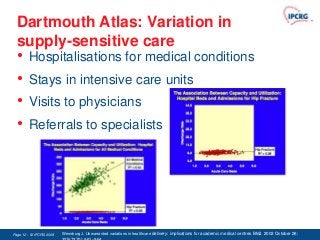
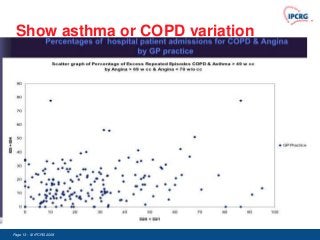
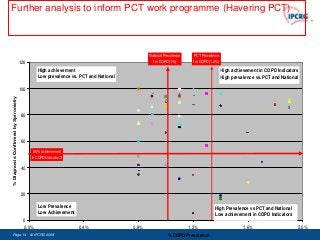
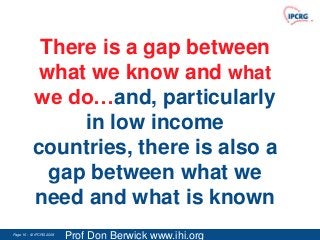
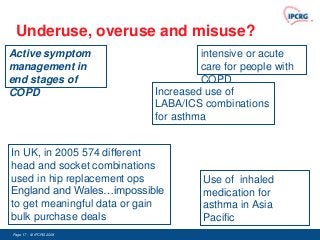
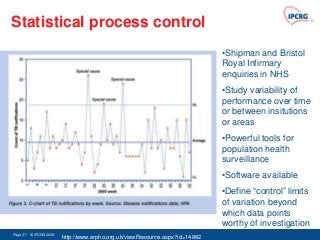
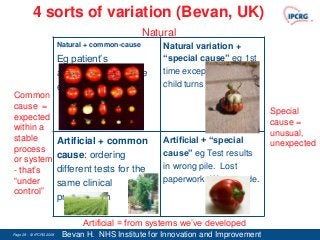
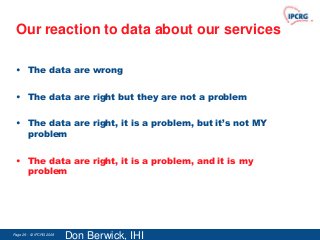
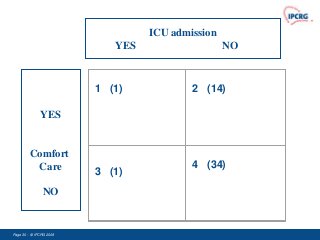
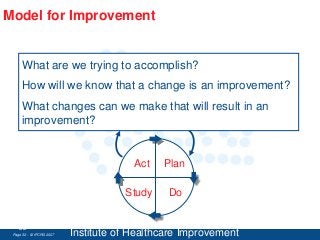
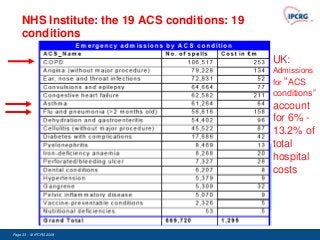
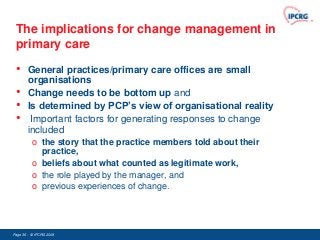
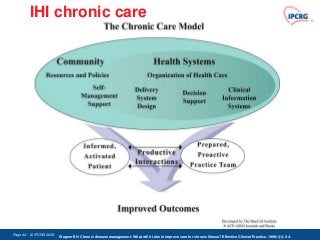
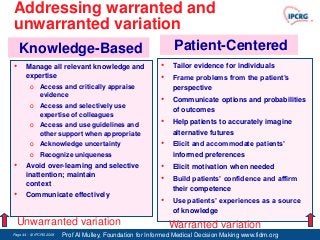
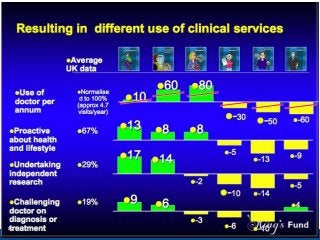
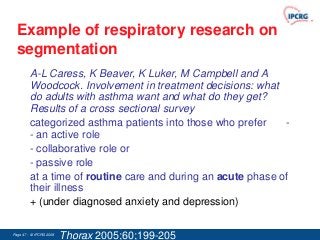
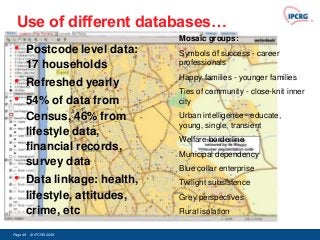
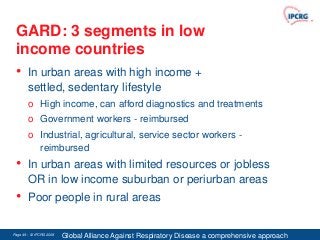
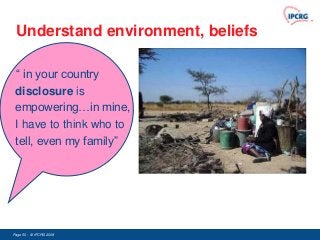
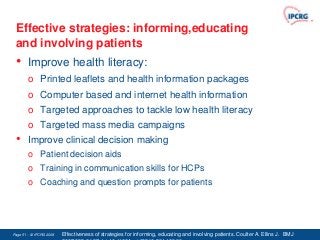
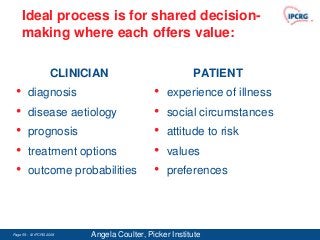
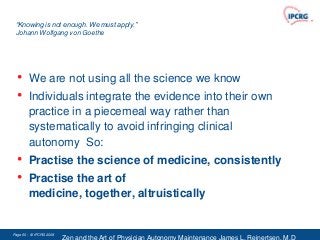
This document discusses variation in healthcare and chronic disease management. It covers what variation is, why it matters, and how it should be analyzed. It notes there are warranted and unwarranted sources of variation. The document recommends addressing unwarranted variation by managing knowledge and expertise, tailoring evidence to individuals, and communicating options from the patient's perspective.








![Reliability science [René Amalberti IHI]
No limit on discretion Increasing safety margins
Excessive autonomy of actors Becoming team player
Agreeing to become
Craftmanship attitude
« equivalent actors »
Accepting the residual
Ego-centered safety protections, vertical conflicts risk
Accepting that
Loss of visibility of risk, freezing actions changes can be
destructive
Blood transfusion
Fatal Iatrogenic
No system beyond
adverse events Anesthesiology
ASA1
this point
Cardiac Surgery Medical risk (total)
Patient ASA 3-5
Himalaya Chartered Flight
mountaineering Civil Aviation
Microlight or Road Safety Railways (France)
helicopters spreading
activity Chemical Industry (total) Nuclear Industry
10-2 10-3 10-4 10-5 10-6 Fatal
Very unsafe Ultra safe Risk](https://image.slidesharecdn.com/20130207152133372-130207152815-phpapp02/85/Variation-60-320.jpg)