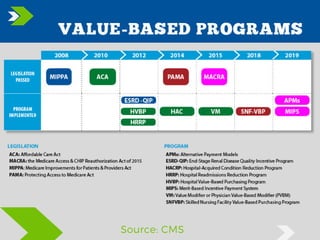
Value-based purchasing (VBP) is a healthcare payment reform method that rewards providers based on quality and efficiency rather than volume. This approach, which includes programs like Hospital Value-Based Purchasing (HVBP) and Skilled Nursing Facility Value-Based Purchasing (SNF-VBP), aims to align financial incentives with care quality and cost reduction. VBP is gaining momentum in healthcare, influencing the future of provider reimbursements and population health management.