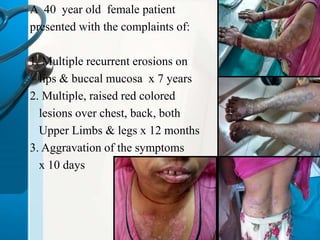
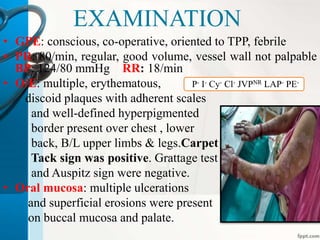
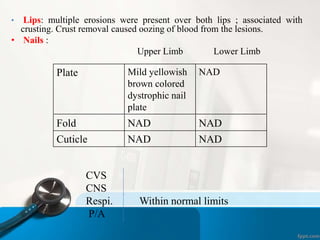
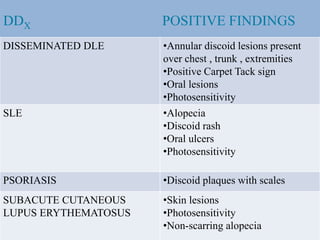
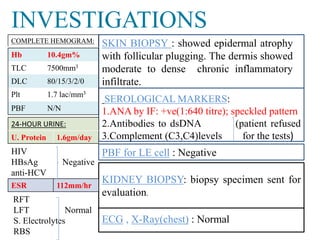
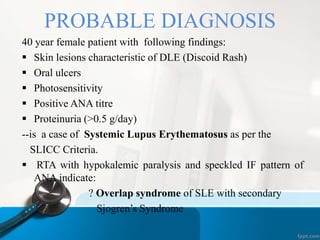
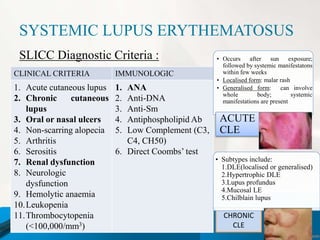
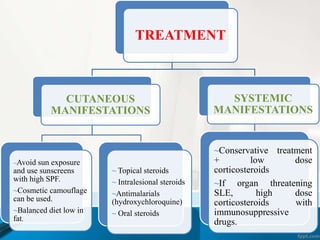
A 40-year-old female presented with recurrent oral erosions for 7 years and raised red skin lesions over her body for 1 year. Examination found discoid skin plaques and oral ulcers. Laboratory tests showed positive ANA, low complement levels, and proteinuria. A skin biopsy demonstrated findings consistent with a connective tissue disease. She was diagnosed with systemic lupus erythematosus based on her skin and oral lesions, photosensitivity, positive serologies, and proteinuria. Her symptoms of renal tubular acidosis and hypokalemic paralysis also indicate an overlap with secondary Sjogren's syndrome.