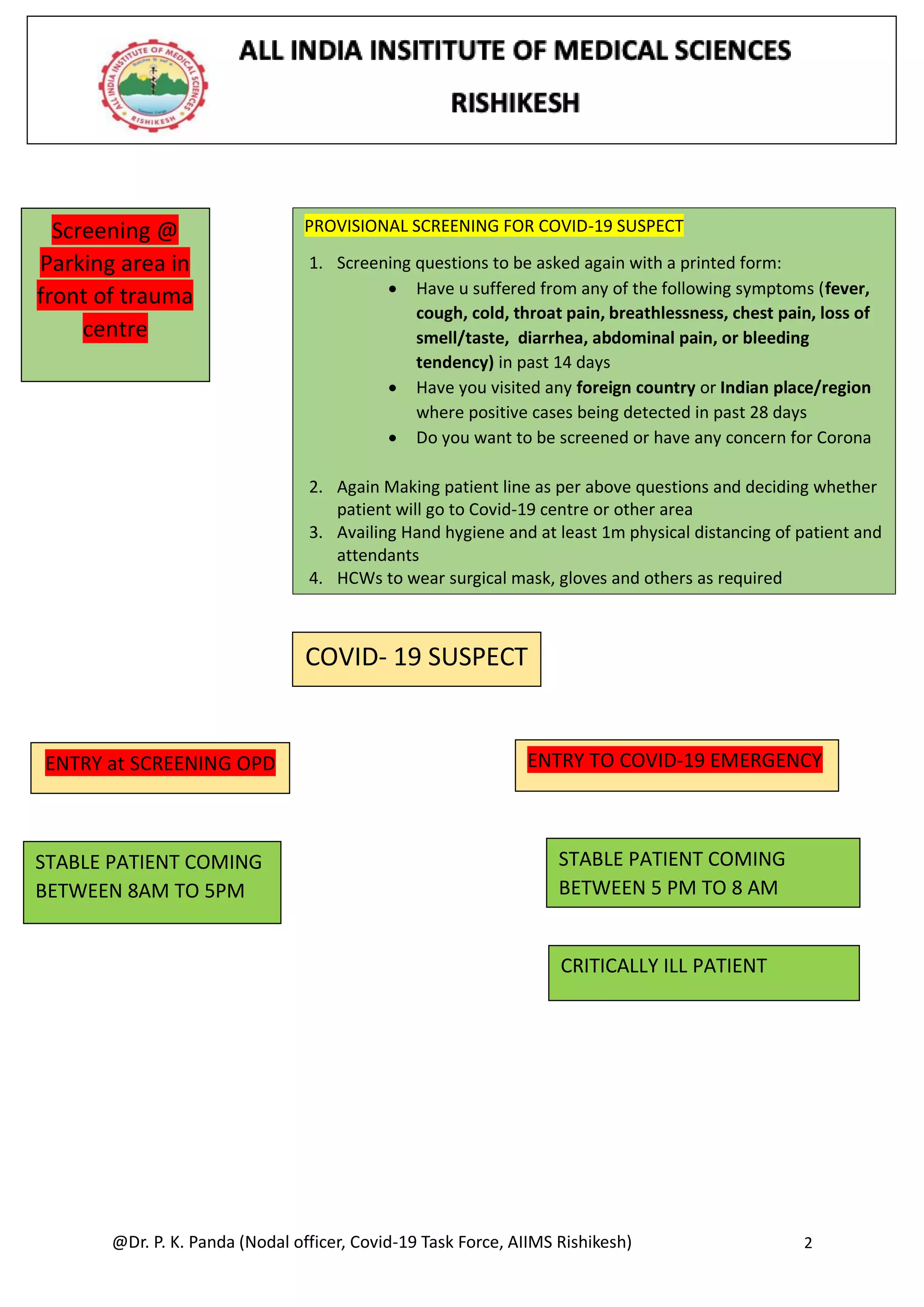
This document outlines clinical management protocols for COVID-19 patients at AIIMS Rishikesh. It details procedures for screening suspect cases, testing criteria, admission criteria, treatment approaches for suspect and confirmed patients, and quarantine policies. It also describes standard operating procedures for different areas of care including the screening OPD, emergency area, isolation ward, and responsibilities of healthcare workers in each area. Precautions and protocols are provided for sample collection, PPE use, patient flow and division of work between residents.

















![@Dr. P. K. Panda (Nodal officer, Covid-19 Task Force, AIIMS Rishikesh) 19
Management protocol for ARDS Patient
1. Implement mechanical ventilation using lower tidal volumes (4–8 ml/kg
predicted body weight, PBW) and lower inspiratory pressures (plateau pressure
2. Hypercapnia is permitted if meeting the pH goal of 7.30-7.45. Ventilator
protocols are available.
3. The use of deep sedation may be required to control respiratory drive and
achieve tidal volume targets
4. In patients with severe ARDS, prone ventilation for >12 hours per day is
recommended
5. Use a conservative fluid management strategy for ARDS patients without tissue
hypoperfusion.
6. In patients with moderate or severe ARDS, higher PEEP instead of lower PEEP is
suggested. Tables are available to guide PEEP titration based on the FiO2
required to maintain SpO2.
7. A related intervention of recruitment manoeuvres (RMs) is delivered as
episodic periods of high continuous positive airway pressure [30–40 cm H2O],
progressive incremental increases in PEEP with constant driving pressure, or
high driving pressure
8. In settings with access to expertise in extracorporeal life support (ECLS),
consider referral of patients with refractory hypoxemia despite lung protective
ventilation.
9. Avoid disconnecting the patient from the ventilator, which results in loss of
PEEP and atelectasis.
10. Use in-line catheters for airway suctioning and clamp endotracheal tube when
disconnection is required
11.Use of corticosteroid in selected patient is permitted only after consultation
with on-call faculty](https://image.slidesharecdn.com/updatedmanagementprotocolcovid-19aiimsrishikeshversion4-220306064706/75/Updated-management-protocol-covid-19-aiims-rishikesh_version-4-0-19-2048.jpg)
![@Dr. P. K. Panda (Nodal officer, Covid-19 Task Force, AIIMS Rishikesh) 20
Prevention of Complications
Anticipated
Outcome
Interventions
1. Reduce days of
invasive mechanical
ventilation
• Use weaning protocols that include daily assessment for
readiness to breathe spontaneously
• Minimize continuous or intermittent sedation, targeting
specific titration endpoints (light sedation unless
contraindicated) or with daily interruption of continuous
sedative infusions
2. Reduce incidence
of ventilator
associated
pneumonia
• Keep patient in semi-recumbent position (head of bed
elevation 30-45º)
• Use a closed suctioning system; periodically drain and
discard condensate in tubing
• Change heat moisture exchanger when it malfunctions,
when soiled, or every 5–7 days
3. Reduce incidence
of venous
thromboembolism
• Use pharmacological prophylaxis (low molecular-weight
heparin[preferred if available] or heparin 5000 units
subcutaneously twice daily) in adolescents and adults
without contraindications.
• For those with contraindications, use mechanical
prophylaxis (intermittent pneumatic compression
devices)
4. Reduce incidence
of catheter related
bloodstream
infection
• Use a checklist with completion verified by a real-time
observer as reminder of each step needed for sterile
insertion and as a daily reminder to remove catheter if
no longer needed
5. Reduce incidence
of pressure
• Turn patient every two hours
6. Reduce incidence
of stress ulcers and
gastrointestinal
bleeding
• Give early enteral nutrition (within 24–48 hours of
admission)
• Administer histamine-2 receptor blockers or proton-
pump inhibitors in patients with risk factors for GI
bleeding.](https://image.slidesharecdn.com/updatedmanagementprotocolcovid-19aiimsrishikeshversion4-220306064706/75/Updated-management-protocol-covid-19-aiims-rishikesh_version-4-0-20-2048.jpg)
























![@Dr. P. K. Panda (Nodal officer, Covid-19 Task Force, AIIMS Rishikesh) 46
*Urgent indication –
1. Lung collapse with significant hypoxemia due to mucous plug or blood clot, which cannot be managed by conservative methods.
2. Life-threatening hemoptysis.
3. Symptomatic/difficult-to-ventilate central airway obstruction due to airway stenosis, endobronchial growth or extrinsic airway
compression.
4. For obtaining BAL if diagnosis cannot be established with other less invasive techniques. (eg. sputum analysis in non-intubated
patients, ET aspirate/mini-BAL in intubated patients).
**Non urgent indication – Other indications for bronchoscopy.
2. Patients with suspected COVID-19 disease should NOT undergo bronchoscopy for purposes of establishing a diagnosis of COVID-19. (3A)
3. Patients with suspected or diagnosed COVID-19 disease with additional non-urgent pulmonary pathologies (e.g. new consolidation, mild
hemoptysis) should undergo a non-bronchoscopic intervention for evaluation preferentially. (UPP)
Comments for 1-3: Research for treatment of COVID-19 is currently in its early phase, and at present, there is no evidence-backed treatment
available. Hence, the most effective method of epidemiological control presently is prevention. Upper respiratory tract sampling for diagnosis of COVID-
19 is the method of choice. Bronchoscopy is classified as a procedure with high risk for aerosolization of infected material.[1] Thereby it is best advised
avoiding a bronchoscopic evaluation for purely diagnostic purposes. With a negative upper respiratory sampling and persistent suspicion, repeat upper
respiratory sampling is advisable. Similarly, suspects or proven COVID-19 cases with non-life-threatening indications for bronchoscopy are best
managed with conservative or empirical management rather than a routine bronchoscopic evaluation.
4. Patients with suspected or diagnosed COVID-19 disease with additional urgent pulmonary pathologies, or those with non-urgent pathologies
not resolved by all possible non-bronchoscopic means, should undergo a bronchoscopic evaluation as per a priority list based on the anticipated
outcome. (UPP)
Comments for 4: Some cases with suspected or diagnosed COVID-19 disease may have life-threatening pathologies needing urgent bronchoscopic
evaluation or where despite all methods of non-bronchoscopic evaluation there persists a treatment-dictating pathology which can be evaluated by
bronchoscopy. In times of pandemics, it is likely that there will be multiple such cases and limited resources. Thereby a priority list is essential before
proceeding for a bronchoscopy. This can be done keeping in mind the possible clinical outcome of the patient (in terms of salvageability) and availability
of resources.](https://image.slidesharecdn.com/updatedmanagementprotocolcovid-19aiimsrishikeshversion4-220306064706/75/Updated-management-protocol-covid-19-aiims-rishikesh_version-4-0-46-2048.jpg)
![@Dr. P. K. Panda (Nodal officer, Covid-19 Task Force, AIIMS Rishikesh) 47
(For this section, we write “without COVID disease,” so that means we have tested all.? Do we recommend checking
all before bronchoscopy, or do we term them as “not a COVID suspect,” and in that case, how?
5. Patients who are neither ‘COVID-19 suspects’ nor ‘laboratory-confirmed COVID-19 cases’, and present with
urgent pulmonary pathologies requiring bronchoscopic management, should undergo an evaluation as per
human and equipment resource availability in individual centres. (UPP)
6. Patients who are neither ‘COVID-19 suspects’ nor ‘laboratory-confirmed COVID-19 cases’, and present with
non-urgent pulmonary pathologies requiring bronchoscopic management, should be deferred and a priority list
for the same established for assessment in the post-pandemic period. (UPP)
Comments for 5&6: Patients with pulmonary pathologies but without COVID-19 are also likely to visit the hospital in
the times of a pandemic. Those with urgent pulmonary pathologies needing an assessment will have to be catered to as
per the availability of resources at the centre in question.
Those with non-urgent pathologies must be counselled regarding the same and deferred for post-pandemic
assessment. Given the possibility that the pandemic might extend over months, the list will also require prioritization to
appropriately address the backlog after tackling the pandemic.
7. Bronchoscopy should be performed in a negative pressure ventilation room with a minimum of 12 air exchanges
per hour and preferably at the patient’s place of care. (3A)
Comments for 7: As per Occupational Safety and Health Administration (OSHA)[1] and WHO[2] recommendations, for
aerosol-generating procedures (which include bronchoscopies), additional engineering controls as a part of airborne
precautions for prevention of exposure are essential. These include negative pressure ventilation rooms, installation of
high-efficiency particulate air (HEPA) filters, and increased ventilation rates.](https://image.slidesharecdn.com/updatedmanagementprotocolcovid-19aiimsrishikeshversion4-220306064706/75/Updated-management-protocol-covid-19-aiims-rishikesh_version-4-0-47-2048.jpg)
![@Dr. P. K. Panda (Nodal officer, Covid-19 Task Force, AIIMS Rishikesh) 48
Pre-bronchoscopy preparation:
1. The number of personnel for bronchoscopy should be restricted, preferably to two. For intubated patients, if the
bronchoscopist is not an intensivist, then intensivist may be included in the bronchoscopy team for assistance in
sedation and paralysis. (UPP)
2. Arrange all necessary bronchoscopy accessories, including drugs on the sterile trolley, before entering the isolation
room. (UPP) Use a disposable bronchoscope if possible; otherwise follow the routine recommendation for
sterilization of bronchoscope as per manufacturer instruction. (3A)
3. The complete plan of the procedure, including the role of each member, must be discussed within the team, and a
short rehearsal can be done outside the bronchoscopy room. (UPP)
4. For intubated patients, always check the size of the endotracheal tube/tracheostomy. The inner diameter of the
endotracheal/tracheostomy tube should be at least 2 mm more than the outer diameter of the bronchoscope to facilitate
smooth entry of the bronchoscope and for optimal ventilation during the procedure.[3] (3A)
5. Donning and doffing of PPE should be in a designated place outside the bronchoscopy room. All personnel for
bronchoscopy should wear full PPE including Filtering Face Piece (FFP) - 3, eyeshield/goggles, hood/cap, gown,
shoe covers, and double gloves. (3A)
6. The patient should be draped completely with sterile sheet. (UPP)
Comments: The minimum necessary personnel and equipment should be kept during the procedure so as to reduce the
risk of infection. As per CDC[4], WHO[2] and OSHA[1] guidelines, full PPE inclusive of an FFP3, eye shield/goggles, hood,
gown, shoe covers, and double gloves, should be made available for all involved personnel.[1,2,4] Given the limited
evidence currently available for the virus, a separate or disposable bronchoscope[5] must be considered for procedures in
COVID-19 suspected or proven cases. The recommendations for sterilization during the previous SARS epidemics have
varied, however, practicing high-level disinfection with routine bronchoscope reprocessing advice as per manufacturer
should continue till further evidence is available. Adequate planning of the procedure with role identification is essential
to minimize the duration of the procedure and ensure smooth entry and exit. An ante-room to the bronchoscopy area is
advisable as suggested by the CDC for airborne infection isolation measures,[6] which can serve the dual purpose of a
planning area and an area for donning and doffing of PPE.
7.](https://image.slidesharecdn.com/updatedmanagementprotocolcovid-19aiimsrishikeshversion4-220306064706/75/Updated-management-protocol-covid-19-aiims-rishikesh_version-4-0-48-2048.jpg)
![@Dr. P. K. Panda (Nodal officer, Covid-19 Task Force, AIIMS Rishikesh) 49
During the procedure:
During the procedure:
1. Position the sterile trolley and team members as decided outside of the procedure area (Figure 2). All team members
should position themselves at an arm’s length from the patient bed. (UPP)
Figure 2. Position of personnel during bronchoscopy.
2. The risk of aerosolization in bronchoscopy is higher in a patient who coughs during the procedure, thereby
appropriate measures to prevent the same need to be in place. These include:
a) Bronchoscopy should be done preferably in deep sedation (with an airway conduit if resources are available)
to minimize coughing and aerosol generation. (UPP) For intubated patients, pre-bronchoscopy medication
should include sedation and paralytic agents unless contraindicated otherwise. (3A)
b) For bronchoscopy, use of a trans-nasal approach[7,8] with a surgical face-mask is preferred over a transoral
approach.](https://image.slidesharecdn.com/updatedmanagementprotocolcovid-19aiimsrishikeshversion4-220306064706/75/Updated-management-protocol-covid-19-aiims-rishikesh_version-4-0-49-2048.jpg)
![@Dr. P. K. Panda (Nodal officer, Covid-19 Task Force, AIIMS Rishikesh) 50
3. In intubated patients, a three-way (swivel) adapter (Figure 3) for bronchoscope entry is recommended. This
avoids disconnection of ventilator circuit during bronchoscope introduction. Besides, it also helps in
maintaining positive end expiratory pressure. (UPP)
In intubated patients, use of a swivel adapter (Figure 3) allows optimal simultaneous ventilation and the snug
fit limits the air leak, thereby also the exposure during bronchoscopy.[9]
Figure. Swivel/three-way adapter
4. Procedure duration should be minimized as far as possible, and to achieve this, the following measures can be
taken:
a. Cricothyroid administration of local anaesthetic is advisable over the spray-as-you-go method, as the
former is associated with better patient comfort in terms of lesser cough and lower cumulative dose
of the local anaesthetic agent.[10]
b. Consider the evaluation of only those bronchopulmonary segments suspected to be involved as against
screening normal airways as well. (UPP)
c. In intubated patients, avoid instillation of local anaesthetic if patient is in complete paralysis. (UPP)](https://image.slidesharecdn.com/updatedmanagementprotocolcovid-19aiimsrishikeshversion4-220306064706/75/Updated-management-protocol-covid-19-aiims-rishikesh_version-4-0-50-2048.jpg)

![@Dr. P. K. Panda (Nodal officer, Covid-19 Task Force, AIIMS Rishikesh) 52
After the procedure:
1. Handle the bronchoscopy samples (if taken) as per infection control guidelines.[11] (3A)
2. Doffing of all personnel and disposal of PPE must be as per guidelines. (3A)
(https://www.cdc.gov/hai/prevent/ppe.html)
3. Standard disinfection protocols should be followed for cleaning the flexible bronchoscope and
accessories. (3A)
4. Post-procedure sterilization for reusable bronchoscopes should be as per routine recommendation for
sterilization of bronchoscope (as per manufacturer’s instruction).
5. For all personnel involved in the bronchoscopy, post-procedure decontamination with a shower is
recommended. (3A)
Comments: Given the highly infectious nature of the virus, lower respiratory tract samples should be handled
with utmost care. The ACCP recommendations for the same during the SARS epidemic may be followed.[11]](https://image.slidesharecdn.com/updatedmanagementprotocolcovid-19aiimsrishikeshversion4-220306064706/75/Updated-management-protocol-covid-19-aiims-rishikesh_version-4-0-52-2048.jpg)