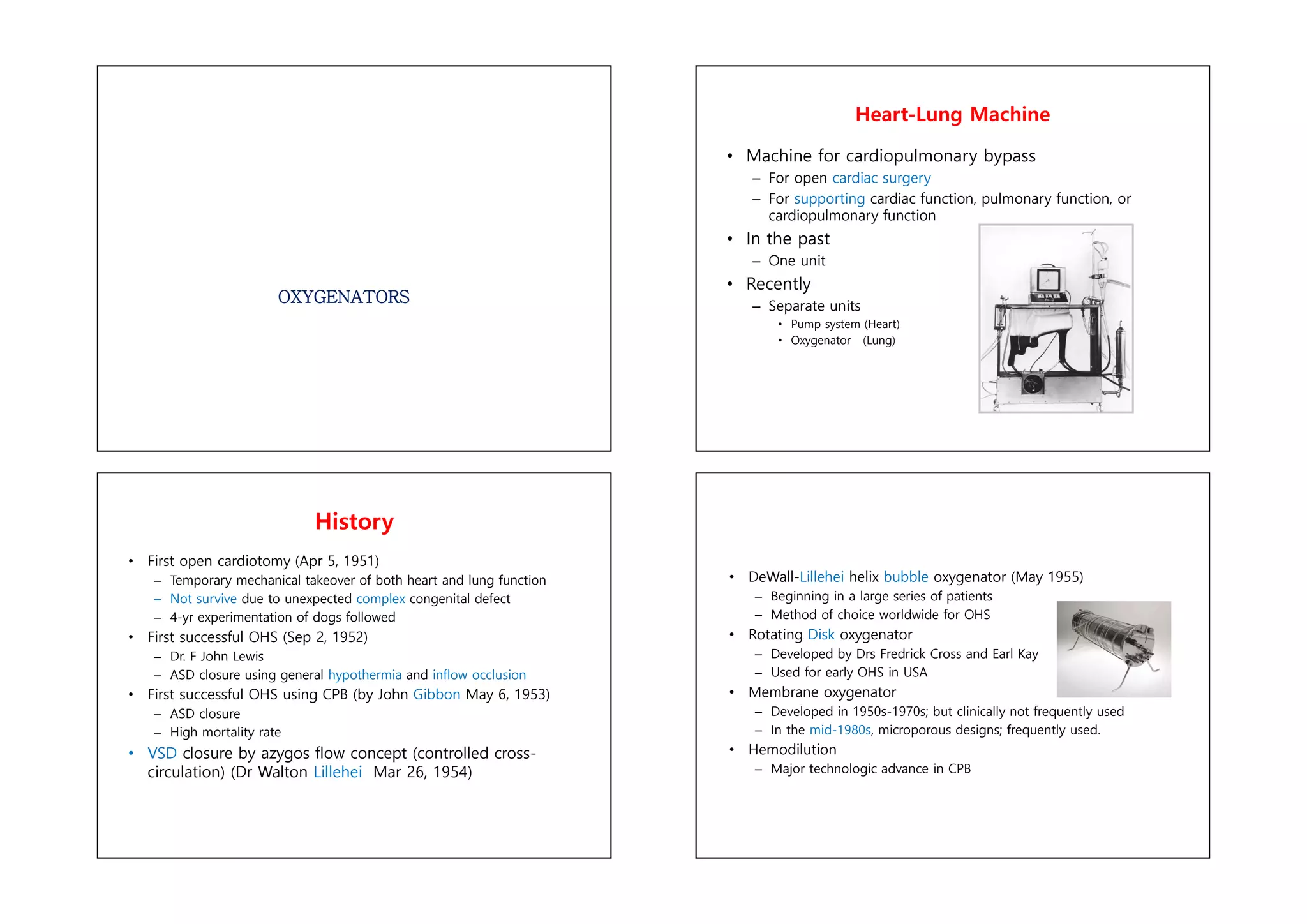
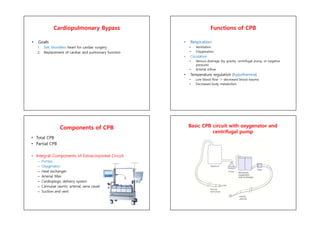
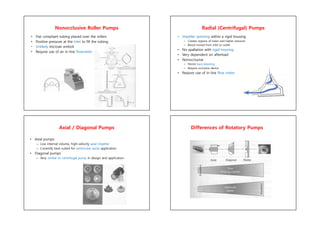
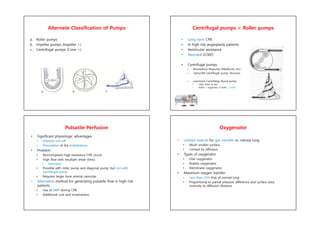
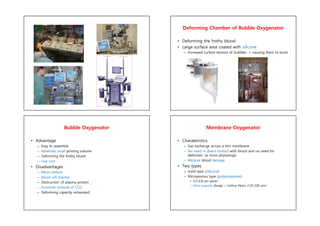
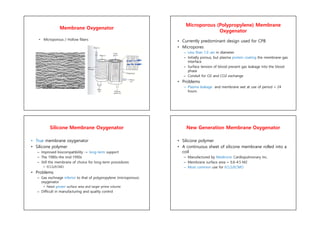
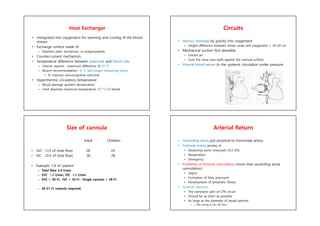
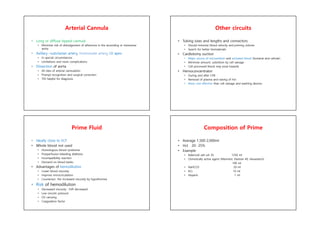
The document discusses the history and components of cardiopulmonary bypass (CPB) and oxygenators used for open heart surgery. It describes how CPB machines have evolved from using a single heart-lung unit to separate pump and oxygenator units. Modern oxygenators often use microporous membranes or hollow fibers for gas exchange with less blood trauma than older bubble or disk oxygenators. The document also outlines the typical components of a CPB circuit including pumps, oxygenators, heat exchangers and cannulae.