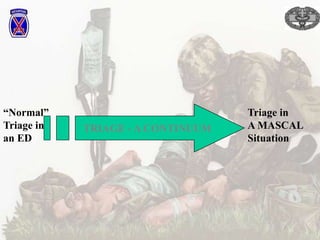
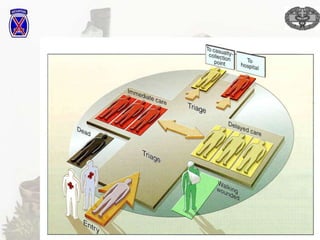
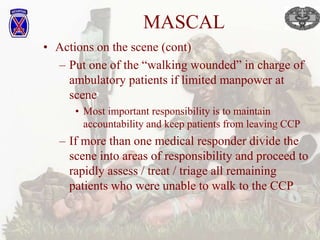
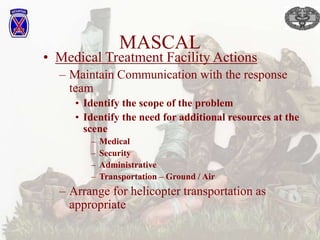
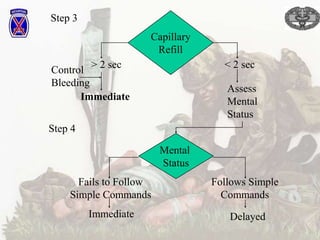
The document provides information on triage procedures for mass casualty incidents. It discusses sorting injured personnel into categories based on need for treatment. The categories include Immediate for life-threatening injuries, Urgent for injuries at risk if treatment is delayed, Delayed for non-life-threatening injuries, and Expectant for those unlikely to survive given available resources. It emphasizes that triage is a dynamic process that can change based on evolving conditions like available resources, patient status, or environmental factors. The document also discusses differences between military and civilian triage as well as considerations for treatment facilities in a mass casualty response.