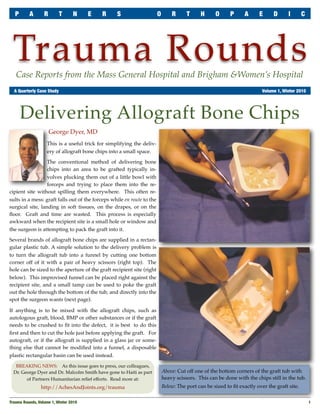
This document summarizes a technique for delivering allograft bone chips into a surgical site. It describes how the conventional method of using forceps often results in graft material being spilled. The technique involves cutting a corner off the plastic tub containing the allograft chips to create a makeshift funnel. This funnel can then be placed over the recipient site, and a tamp is used to push the graft material directly into place. An example is given of using this technique for a supracondylar humerus fracture repair. The document also notes that the trauma fellowship program it describes was recently awarded funding from a medical grants organization.