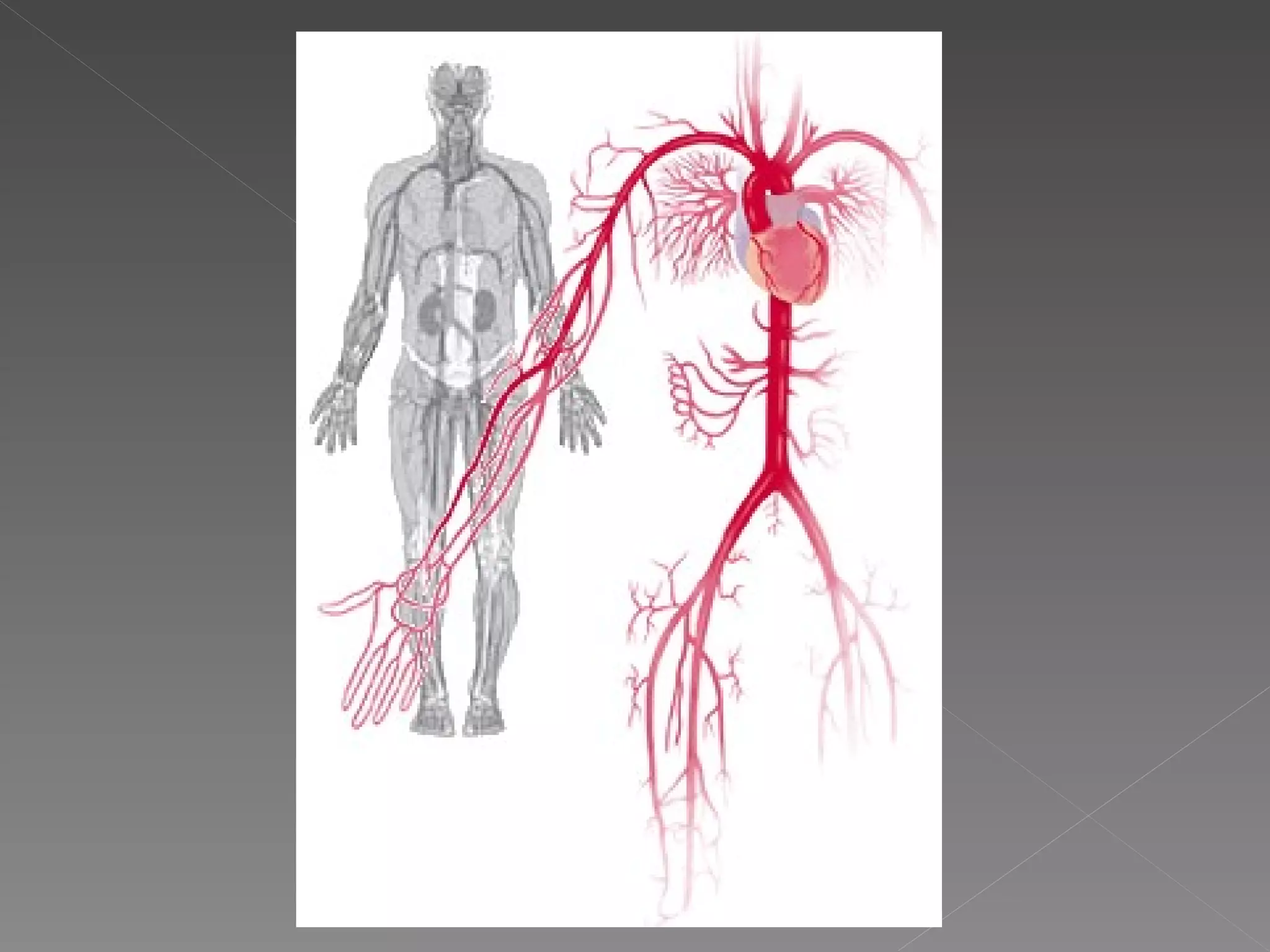
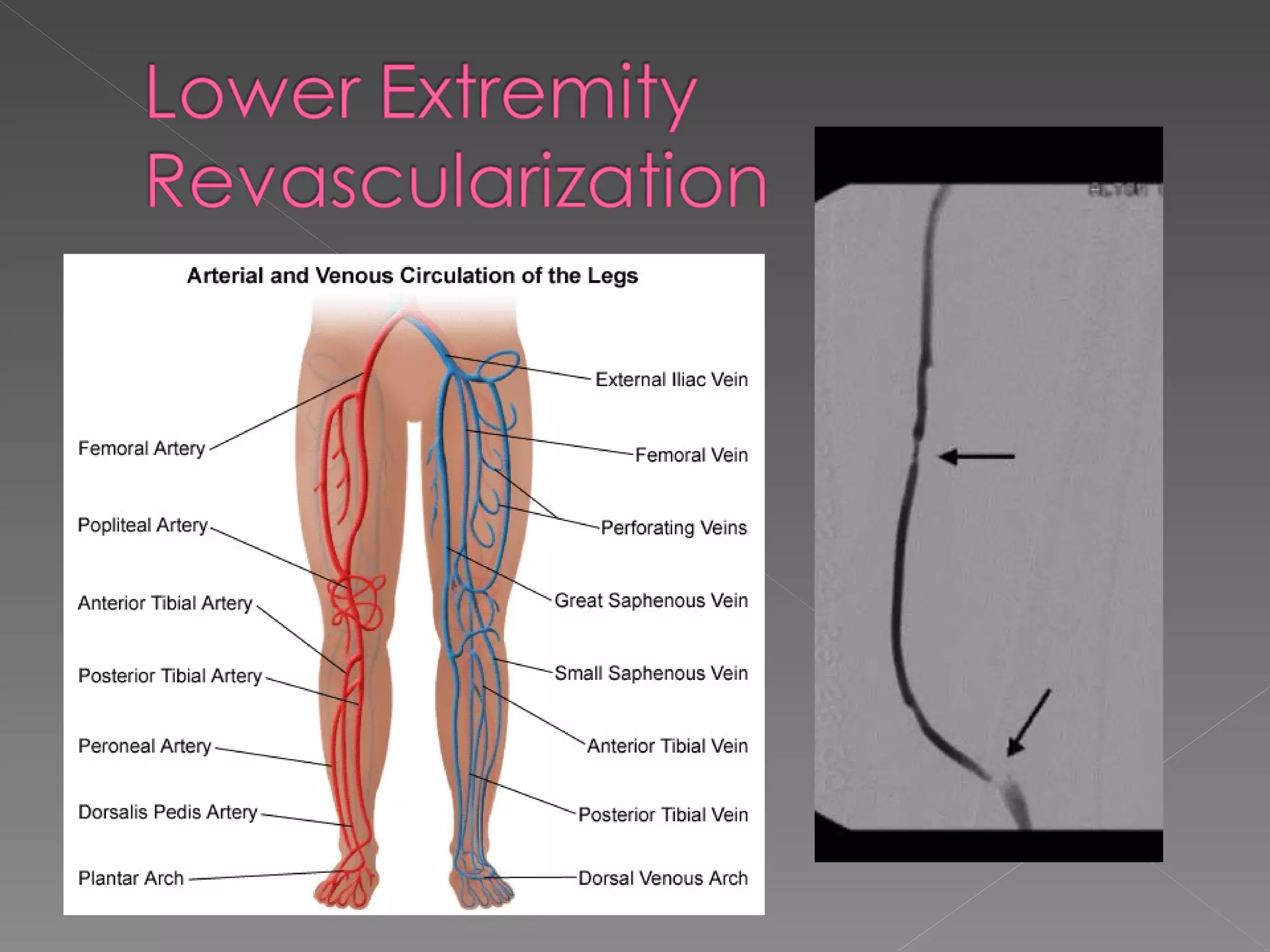
- Aorto-occlusive disease involves atherosclerotic changes in the aorta and iliac/femoral arteries, resulting in inadequate blood flow to organs and limbs. Myocardial dysfunction is a major cause of morbidity after vascular surgery.
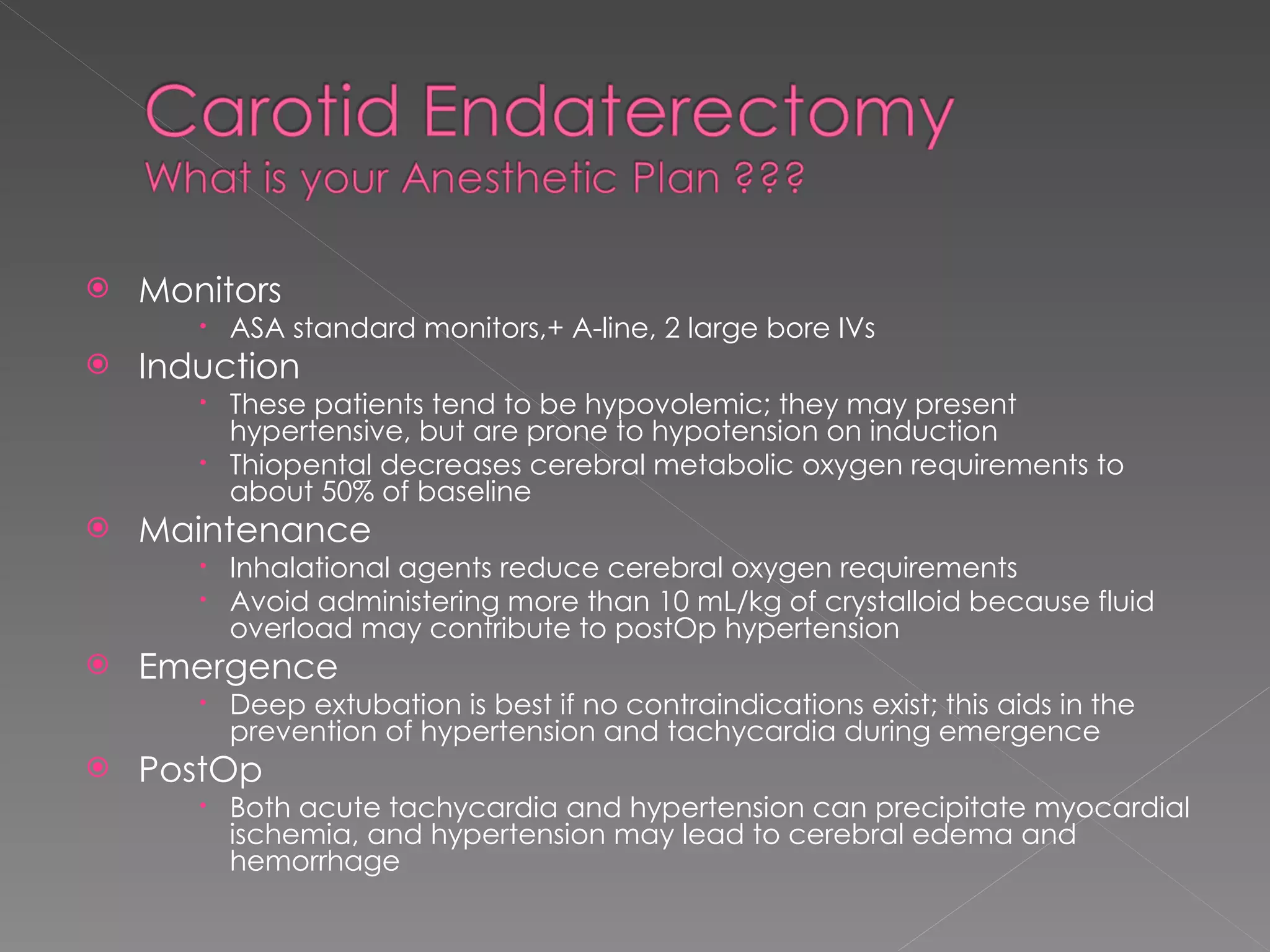
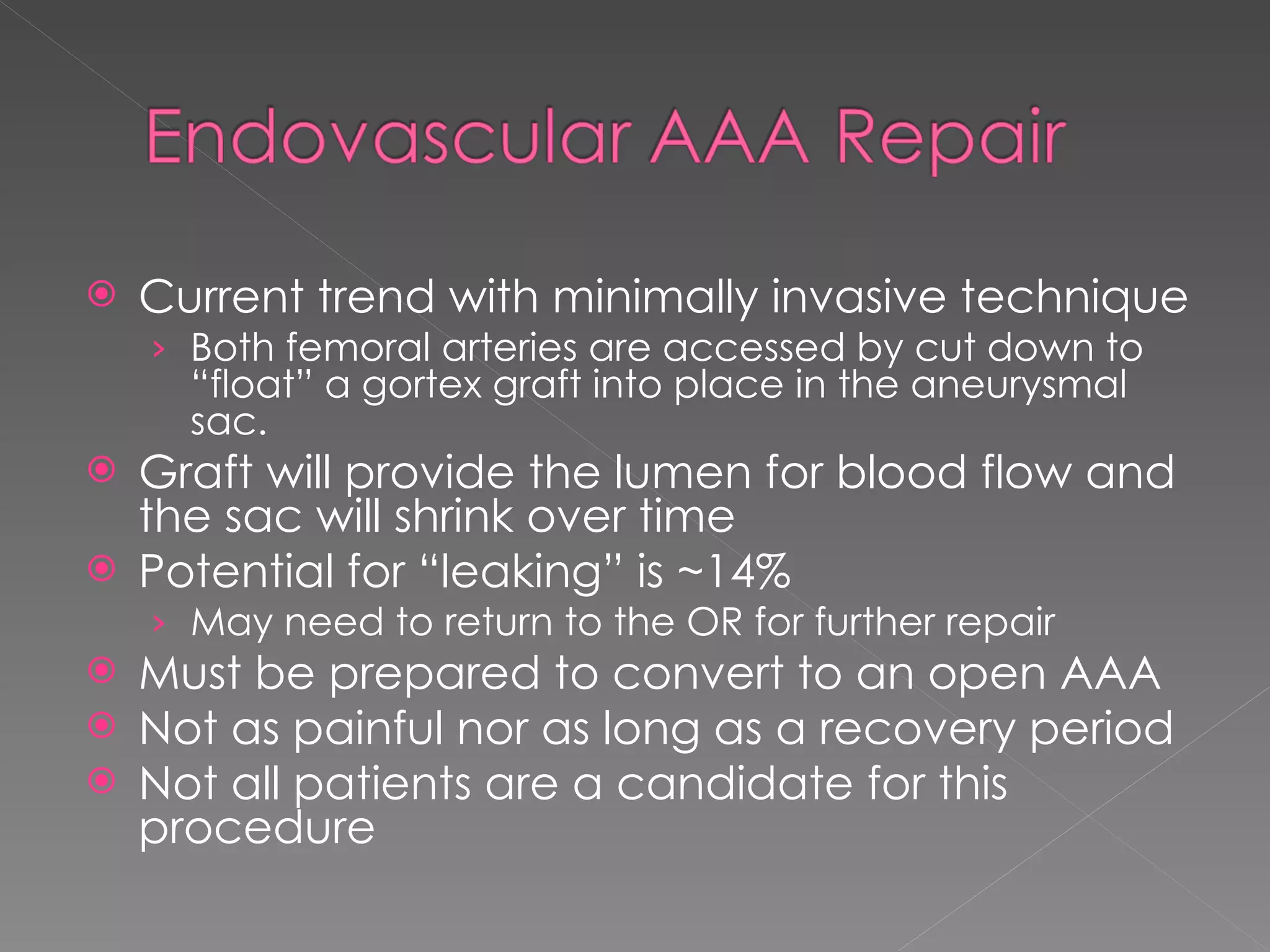
- Patients undergoing vascular surgery often have multiple comorbidities like coronary artery disease, hypertension, diabetes, and impaired cardiac function, placing them at high risk for perioperative complications. Careful monitoring and management of cardiovascular status is important during and after the procedures.
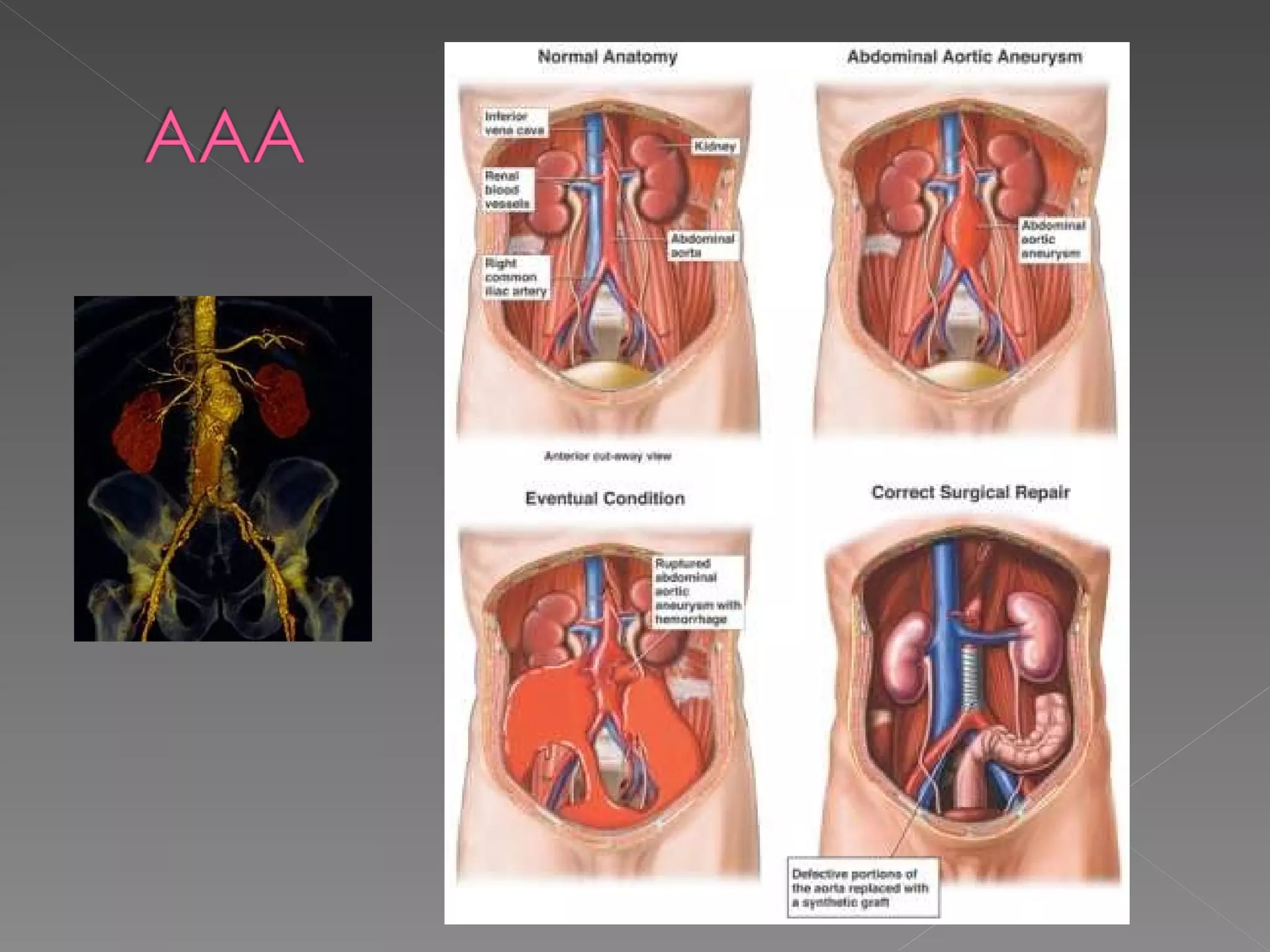
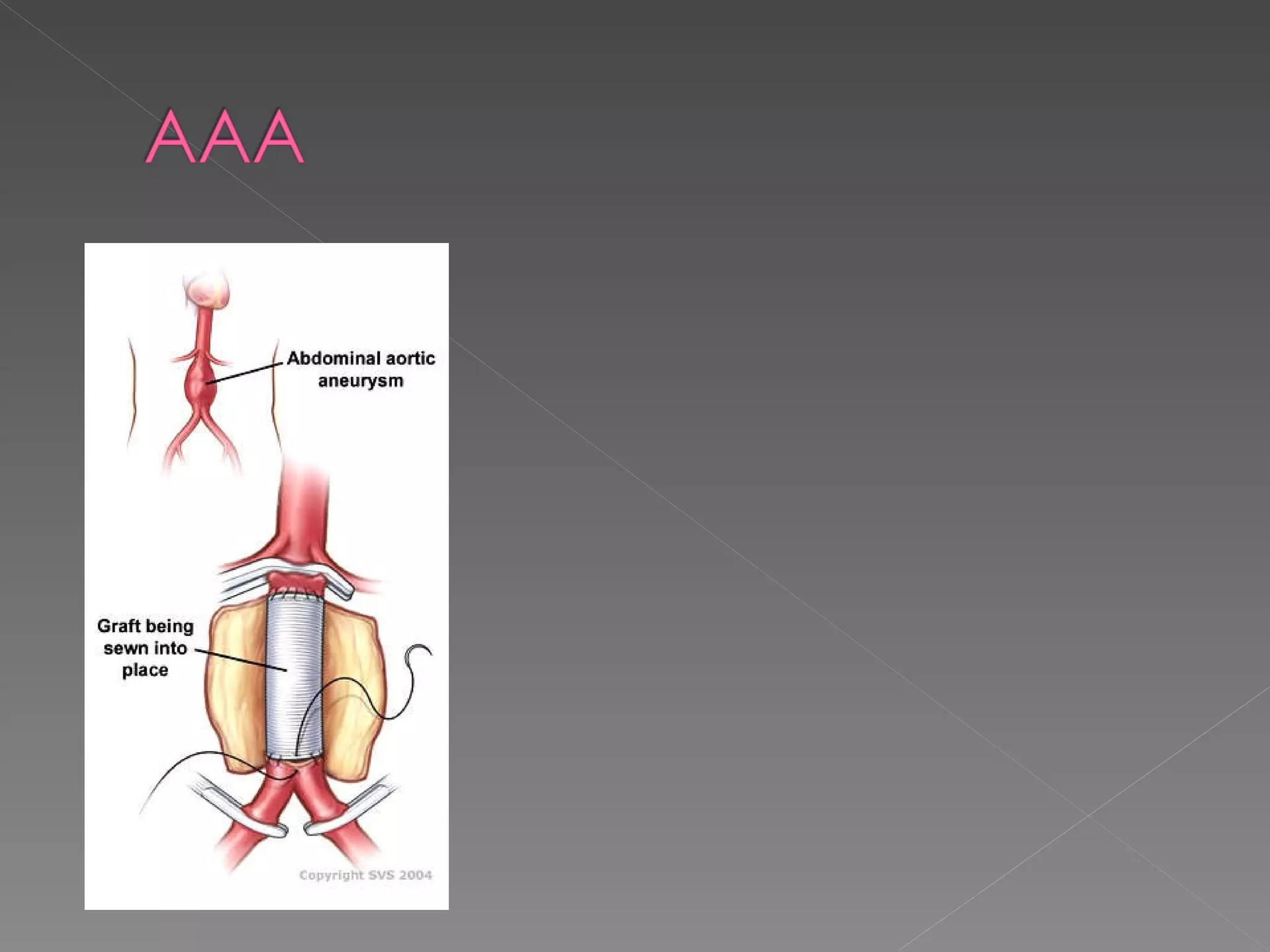
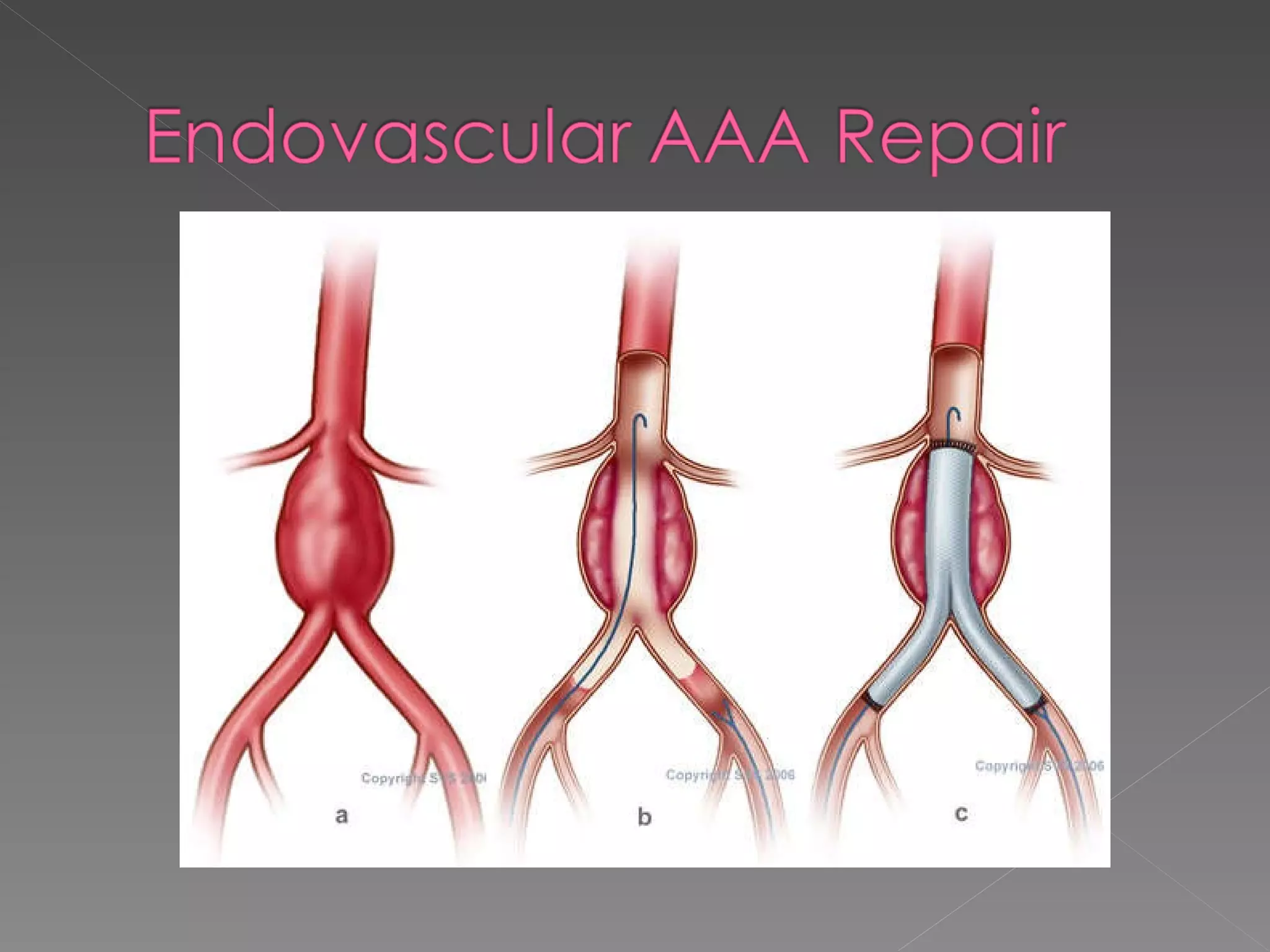
- Aneurysm rupture carries high mortality. Risk of rupture increases with aneurysm size over 4.5-5 cm. Surgery reduces long-term mortality from rupture but also carries risks, especially for emer