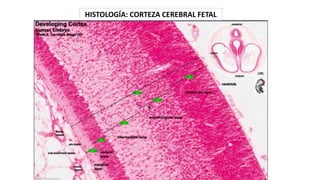
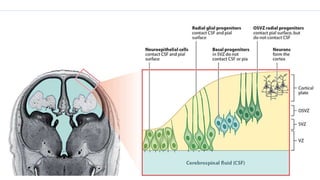
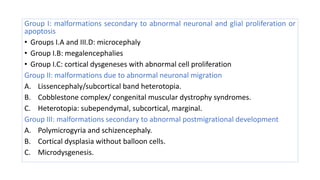
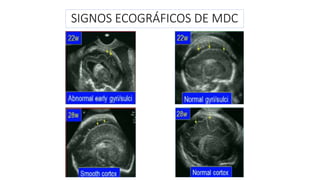
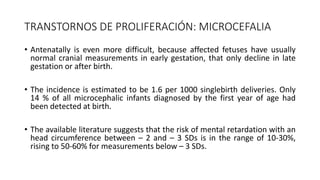
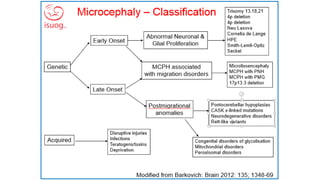
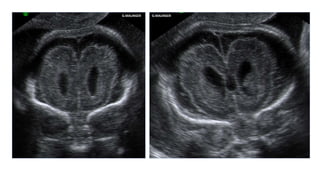
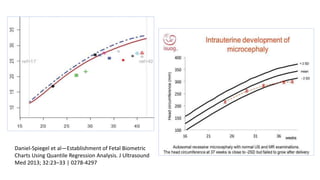
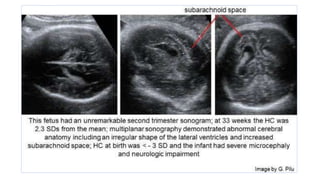
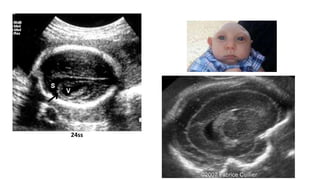
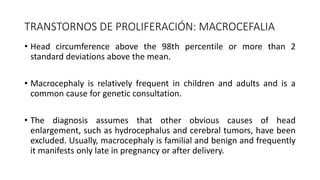
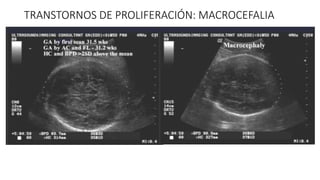
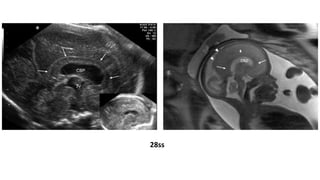
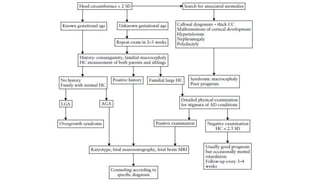
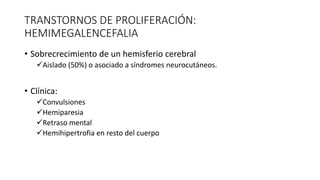
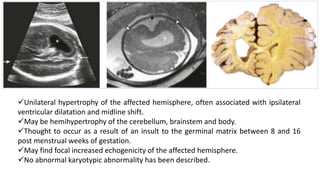
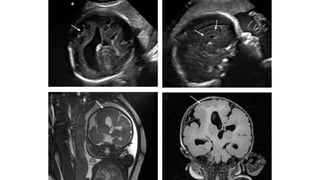
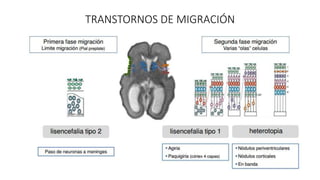
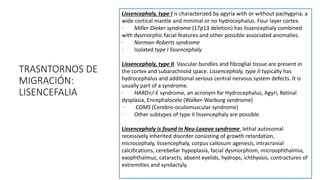
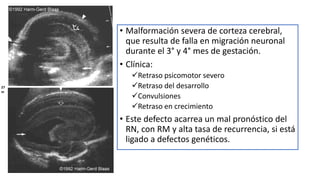
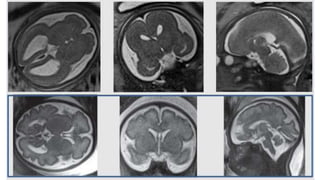
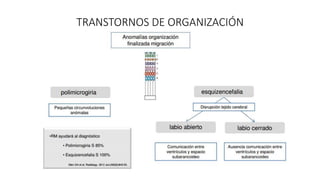
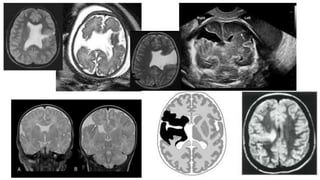
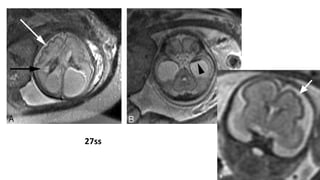
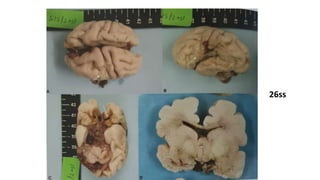
The document discusses fetal cortical development disorders, with an emphasis on microcephaly. It describes how the cerebral cortex develops in an orderly process involving neuronal and glial proliferation, migration from the periventricular zone, and organization. Injuries during this process can result in a wide range of cortical malformations that may cause neurological deficits or seizures. Specific disorders discussed include microcephaly from abnormal proliferation, macrocephaly, hemimegalencephalia from overgrowth of one hemisphere, lissencephaly from abnormal migration, and heterotopias from abnormal organization. The signatures of these disorders are described along with their typical clinical presentations and prognosis.