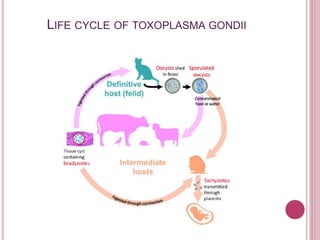
Toxoplasmosis, caused by the protozoan Toxoplasma gondii, is a widely distributed parasite infecting up to 60–80% of the elderly worldwide and poses significant risks for immunocompromised individuals. The disease can be acquired through ingestion of contaminated food or through maternal transmission to the fetus, with symptoms ranging from mild to severe, including lymphadenopathy and ocular or neurological infections. Diagnosis involves serological tests for antibodies, and prevention strategies include avoiding contact with cat feces and undercooked meat, especially for vulnerable populations such as pregnant women.